J Korean Assoc Oral Maxillofac Surg.
2011 Aug;37(4):278-286. 10.5125/jkaoms.2011.37.4.278.
New bone formation using fibrin rich block with concentrated growth factors in maxillary sinus augmentation
- Affiliations
-
- 1Division of Oral and Maxillofacial Surgery, Department of Dentistry, Daegu Catholic University Medical Center, Daegu, Korea. ispark@cu.ac.kr
- KMID: 1449060
- DOI: http://doi.org/10.5125/jkaoms.2011.37.4.278
Abstract
- INTRODUCTION
This study examined the predictability of new bone formation in the pneumatized maxillary sinus using only fibrin-rich blocks with concentrated growth factors as an alternative to bone grafts.
MATERIALS AND METHODS
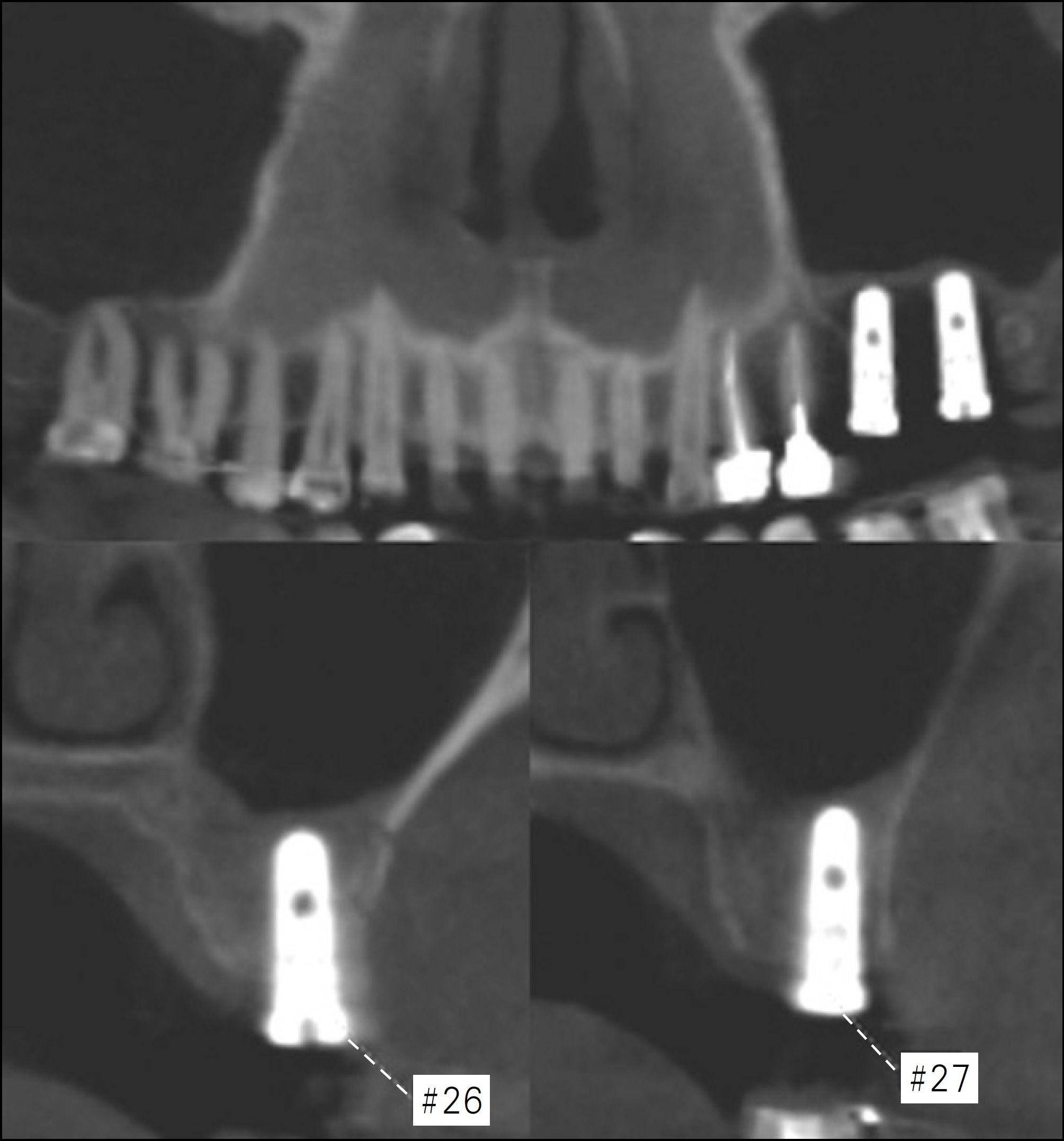
Maxillary sinus augmentation was performed in thirty-three patients with a deficient alveolar bone height (mean 3.9 mm). All patients were treated consecutively with sinus membrane elevation via the lateral window approach and panoramic radiograms and cone-beam computed tomograms were taken to evaluate the remaining bone height and the new bone formation in the maxillary sinus, before and after surgery. Four biopsy specimens were taken at the time of implant consolidation (after an average of five months healing) and were stained by H & E and Trichrome staining.
RESULTS
None of the patients had postoperative complications during implant consolidation. After an average of 5 months since sinus augmentation, newly formed bone was observed in all cases by a radiographic evaluation. In 4 biopsy samples, newly formed bone was observed along the floor of the replaced bony window. The osteoblast lining and well distinguished Osteocytes in the lacunas were observed in the newly formed bone. Of the 74 implants (4 different surfaced implants - resorbable blast media-surfaced (RBM), Hydroxyapatite (HA) coated, acid-etched, sintered porous-surfaced implant) placed, one RBM implant failed. The success rate was 98.6% after a mean of 15 months. DISCUSSION: These results suggest that maxillary sinus augmentation using fibrin rich block with concentrated growth factors is a successful and predictable technique.
MeSH Terms
Figure
Cited by 1 articles
-
Regenerative medicine for the reconstruction of hard tissue defects in oral and maxillofacial surgery
Young-Kyun Kim
J Korean Assoc Oral Maxillofac Surg. 2012;38(2):69-70. doi: 10.5125/jkaoms.2012.38.2.69.
Reference
-
1. Misch CE. Maxillary sinus augmentation for endosteal implants: organized alternative treatment plans. Int J Oral Implantol. 1987; 4:49–58.2. Tatum H Jr. Maxillary and sinus implant reconstructions. Dent Clin North Am. 1986; 30:207–29.3. Boyne PJ, James RA. Grafting of the maxillary sinus floor with autogenous marrow and bone. J Oral Surg. 1980; 38:613–6.4. Aghaloo TL, Moy PK. Which hard tissue augmentation techniques are the most successful in furnishing bony support for implant placement? Int J Oral Maxillofac Implants. 2007; 22:49–70.5. Kent JN, Block MS. Simultaneous maxillary sinus floor bone grafting and placement of hydroxylapatite-coated implants. J Oral Maxillofac Surg. 1989; 47:238–42.
Article6. Adell R, Lekholm U, Gröndahl K, Brånemark PI, Lindström J, Jacobsson M. Reconstruction of severely resorbed edentulous maxillae using osseointegrated fixtures in immediate autogenous bone grafts. Int J Oral Maxillofac Implants. 1990; 5:233–46.7. Cordioli G, Mazzocco C, Schepers E, Brugnolo E, Majzoub Z. Maxillary sinus floor augmentation using bioactive glass granules and autogenous bone with simultaneous implant placement. Clinical and histological findings. Clin Oral Implants Res. 2001; 12:270–8.8. Raghoebar GM, Vissink A, Reintsema H, Batenburg RH. Bone grafting of the floor of the maxillary sinus for the placement of endosseous implants. Br J Oral Maxillofac Surg. 1997; 35:119–25.
Article9. Schlegel AK. Bio-Oss bone replacement material. Long-term results with Bio-Oss bone replacement material. Schweiz Monatsschr Zahnmed. 1996; 106:141–9.10. Schlegel AK, Donath K. BIO-OSS–a resorbable bone substitute? J Long Term Eff Med Implants. 1998; 8:201–9.11. Lundgren S, Andersson S, Gualini F, Sennerby L. Bone reformation with sinus membrane elevation: a new surgical technique for maxillary sinus floor augmentation. Clin Implant Dent Relat Res. 2004; 6:165–73.
Article12. Palma VC, Magro-Filho O, de Oliveria JA, Lundgren S, Salata LA, Sennerby L. Bone reformation and implant integration following maxillary sinus membrane elevation: an experimental study in primates. Clin Implant Dent Relat Res. 2006; 8:11–24.
Article13. Sohn DS, Lee JS, Ahn MR, Shin HI. New bone formation in the maxillary sinus without bone grafts. Implant Dent. 2008; 17:321–31.
Article14. Hatano N, Sennerby L, Lundgren S. Maxillary sinus augmentation using sinus membrane elevation and peripheral venous blood for implant-supported rehabilitation of the atrophic posterior maxilla: case series. Clin Implant Dent Relat Res. 2007; 9:150–5.
Article15. Moon JW, Sohn DS, Heo JU. New Bone Formation in the Maxillary Sinus Using Peripheral Venous Blood Alone. J Oral Maxillofac Surg. 2011; 28:[Epub ahead of print].
Article16. Sohn DS, Moon JW, Moon KN, Cho SC, Kang PS. New bone formation in the maxillary sinus using only absorbable gelatin sponge. J Oral Maxillofac Surg. 2010; 68:1327–33.
Article17. Anitua E, Orive G, Pla R, Roman P, Serrano V, Andl′a I. The effects of PRGF on bone regeneration and on titanium implant osseointegration in goats: a histologic and histomorphometric study. J Biomed Mater Res A. 2009; 91:158–65.
Article18. Plachokova AS, Nikolidakis D, Mulder J, Jansen JA, Creugers NH. Effect of platelet-rich plasma on bone regeneration in dentistry: a systematic review. Clin Oral Implants Res. 2008; 19:539–45.
Article19. Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, Gogly B. Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part I: technological concepts and evolution. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006; 101:e37–44.
Article20. Choukroun J, Diss A, Simonpieri A, Girard MO, Schoeffler C, Dohan SL, et al. Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part IV: clinical effects on tissue healing. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006; 101:e56–60.
Article21. Choukroun J, Diss A, Simonpieri A, Girard MO, Schoeffler C, Dohan SL, Dohan AJ, Mouhyi J, Dohan DM. Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part V: histologic evaluations of PRF effects on bone allograft maturation in sinus lift. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006; 101:299–303.
Article22. Sohn DS, Moon JW, Moon YS, Park JS, Jung HS. The use of concentrated growth factor (CGF) for sinus augmentation. J Oral Implants. 2009; 38:25–38.23. Rodella LF, Favero G, Boninsegna R, Buffoli B, Labanca M, Scari G, et al. Growth factors, CD34 positive cells, and fibrin network analysis in concentrated growth factors fraction. Microsc Res Tech. 2011; 74:772–7.
Article24. Pikos MA. Maxillary sinus membrane repair: report of a technique for large perforations. Implant Dent. 1999; 8:29–34.25. Buser D, Mericske-Stern R, Bernard JP, Behneke A, Behneke N, Hirt HP, Belser UC, Lang NP, et al. Long-term evaluation of non-submerged ITI implants. Part 1: 8-year life table analysis of a prospective multicenter study with 2359 implants. Clin Oral Implants Res. 1997; 8:161–72.
Article26. Sohn DS, Kim WS, An KM, Song KJ, Lee JM, Mun YS. Comparative histomorphometric analysis of maxillary sinus augmentation with and without bone grafting in rabbit. Implant Dent. 2010; 19:259–70.
Article27. Vercellotti T, De Paoli S, Nevins M. The piezoelectric bony window osteotomy and sinus membrane elevation: introduction of a new technique for simplification of the sinus augmentation procedure. Int J Periodontics Restorative Dent. 2001; 21:561–7.28. Sohn DS, Ahn MR, Jang BY. Sinus Bone Graft using Piezoelectric Surgery. Implantology. 2003; 9:48–55.29. Sohn DS, Moon JW, Lee HW, Choi BJ, Shin IH. Comparison of two piezoelectric cutting inserts for lateral bony window osteotomy: a retrospective study of 127 consecutive sites. Int J Oral Maxillofac Implants. 2010; 25:571–6.30. Lioubavina-Hack N, Lang NP, Karring T. Significance of primary stability for osseointegration of dental implants. Clin Oral Implants Res. 2006; 17:244–50.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Vertical Augmentation of Maxillary Posterior Alveolar Ridge Using Allogenic Block Bone Graft and Simultaneous Maxillary Sinus Graft
- SINUS GRAFT AND VERTICAL AUGMENTATION OF MAXILLARY POSTERIOR ALVEOLAR RIDGE USING MANDIBULAR RAMAL BLOCK BONE GRAFT
- Maxillary sinus floor augmentation with anorganic bovine bone: Histologic evaluation in humans
- A Case of Maxillary Sinusitis after Sinus Floor Augmentation
- Management of Perioperative Pathologic Conditions Involving Maxillary Sinus for Dental Implant Placement and Sinus Augmentation: Report of Case Series and Literature Review