J Korean Assoc Oral Maxillofac Surg.
2011 Aug;37(4):272-277. 10.5125/jkaoms.2011.37.4.272.
Comparative study on the estimated blood loss follwing to orthognathic surgeries
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, School of Medicine, Ewha Womans University, Seoul, Korea. sjsj7777@ewha.ac.kr
- KMID: 1449059
- DOI: http://doi.org/10.5125/jkaoms.2011.37.4.272
Abstract
- PURPOSE
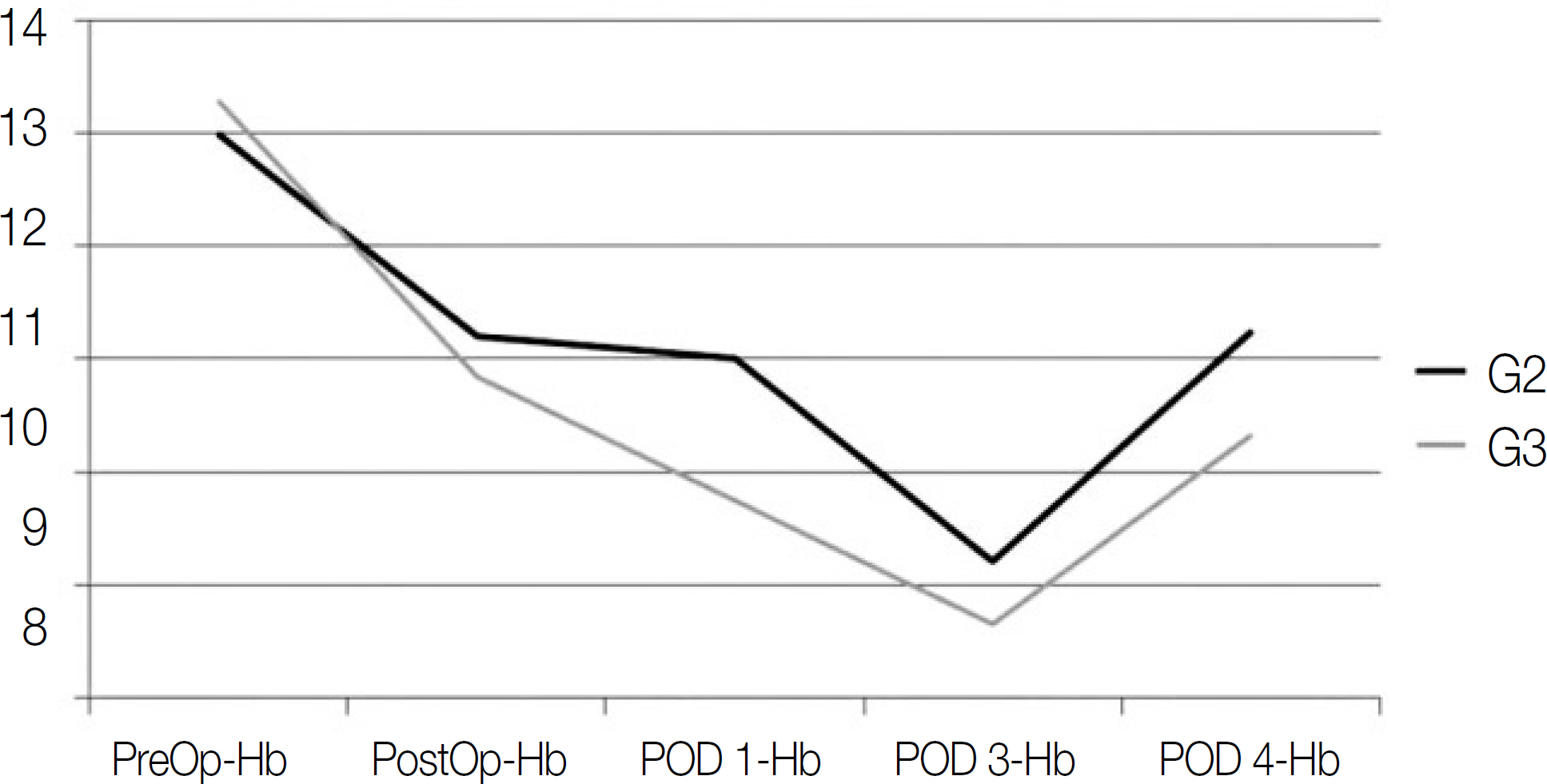
The aim of this study was to compare the estimated blood loss and determine the change in hemoglobin depending on the combination of each orthognathic surgery.
SUBJECTS AND METHODS
The subjects of this study were patients who underwent orthognathic surgery among those diagnosed with a dentofaical deformity in Mok-Dong hospital, Ewha Womans University from 2002 to 2009. One hundred patients (men - 36, women - 64, mean age of 24.5+/-4.6) participated in the study and were divided into four groups (group 1 - bilateral sagittal ramus osteotomy [BSSRO], group 2 - BSSRO+Genioplasty, group 3 - Lefort 1+BSSRO+genioplasty, group 4 - anterior segmental osteotomy on maxilla and mandible). A comparative study on the estimated blood loss (EBL), operation time, peri-operative changes in hemoglobin was performed using anesthesia records. The results were analyzed statistically using a Mann-Whitney U-test and Spearman's Rho test - SPSS 12.0 (SPSS Inc. Chicago, IL, USA).
RESULTS
In group 1 (BSSRO), the mean EBL, operation time and change in hemoglobin was 394.43+/-52.69 ml, 184+/-42.33 minutes, and 1.43, respectively, In group 2 (BSSRO+genioplasty), it was 556.32+/-63.42 ml, 231+/-37.45 minutes, and 1.80, respectively. In group 3 (Lefort 1+BSSRO+Genioplasty), it was 820.55+/-105.54 ml, 320+/-15.41 minutes, and 2.73, respectively. In group 4 (segmental osteotomy), it was 1025.39+/-160.21 ml, 355+/-20.10 minutes, and 3.33, respectively. In particular, in group 3, significant differences were observed depending on the method of the orthognathic surgery. The mean EBL in a Lefort 1 osteotomy with advancement was only 687 ml, whereas Lefort 1 osteotomy with canting correction (992 ml), even impaction (764 ml), and posterior nasal spine impaction (100 ml) showed a much higher EBL.
CONCLUSION
From these results, the EBL and peri-operation hemoglobin increased as treatment plans became more complicated and increasing operation time. Safe orthognathic surgery should be performed by applying proper autologous transfusion plans based on the average EBL of each orthognathic surgery type.
MeSH Terms
Figure
Reference
-
1. Patel PK, Morris DE, Gassman A. Complications of orthognathic surgery. J Craniofac Surg. 2007; 18:975–85.
Article2. Rohling RG, Zimmermann AP, Biro P, Haers PE, Sailer HF. Alternative methods for reduction of blood loss during elective orthognathic surgery. Int J Adult Orthodon Orthognath Surg. 1999; 14:77–82.3. Chan W, Smeth DE, Ware WH. Effects of hypotensive anesthesia in anterior maxillary osteotomy. J Oral Surg. 1980; 38:504–8.4. Schaberg SJ, Kelly JF, Terry BC, Posner MA, Anderson EF. Blood loss and hypotensive anaesthesia in oral-facial corrective surgery. J Oral Surg. 1976; 34:147–56.5. Moenning JE, Bussard DA, Lapp TH, Garrison BT. Average blood loss and the risk of requiring perioperative blood transfusion in 506 orthognathic surgical procedures. J Oral Maxillofac Surg. 1995; 53:880–3.
Article6. Ervens J, Marks C, Hechler M, Plath T, Hansen D, Hoffmeister B. Effect of induced hypotensive anaesthesia vs isovolaemic ae-modilution on blood loss and transfusion requirements in orthognathic surgery: a prospective, single-blinded, randomized, controlled clinical study. Int J Oral Maxillofac Surg. 2010; 39:1168–74.7. Samman N, Cheung LK, Tong AC, Tideman H. Blood loss and transfusion requirements in orthognathic surgery. J Oral Maxillofac Surg. 1996; 54:21–4.8. Stramer SL. Current risks of transfusion-transmitted agents: a review. Arch Pathol Lab Med. 2007; 131:702–7.
Article9. Hegtvedt AK, Ollins ML, White RP Jr, Turvey TA. Minimizing the risk of transfusion in orthognathic surgery: use ofpredeposit-ed autologous blood. Int J Adult Orthodon Orthognath Surg. 1987; 2:185–92.10. Puelacher W, Hinteregger G, Nussbaumer W, Braito I, Waldhart E. Preopreative autologous blood donation in orthognathic surgery: a followup study of 179 patients. J Craniomaxillofac Surg. 1998; 26:121–5.11. Ueki K, Marukawa K, Shimada M, Nakagawa K, Yamamoto E. The assessment of blood loss in orthognathic surgery for prog-nathia. J Oral Maxillofac Surg. 2005; 63:350–4.
Article12. Dolman RM, Bentley KC, Head TW, English M. The effect of hypotensive anesthesia on blood loss and operative time during Le Fort I osteotomies. J Oral Maxillofac Surg. 2000; 58:834–9. discussion 840.
Article13. Kemmochi M, Ichinohe T, Kaneko Y. Remifentanil decreases mandibular bone marrow blood flow during propofol or sevoflurane anesthesia in rabbits. J Oral Maxillofac Surg. 2009; 67:1245–50.
Article14. Marciani RD, Dickson LG. Autologous transfusion in orthognathic surgery. J Oral Maxillofac Surg. 1985; 43:201–4.
Article15. Neuwirth BR, White RP Jr, Collins ML, Phillips C. Recovery following orthognathic surgery and autologous blood transfusion. Int J Adult Orthodon Orthognath Surg. 1992; 7:221–8.16. Petz LD, Swisher SN, Kleinman S, Spence RK, Strauss RG. Clinical practice of transfusion medicine. 3rd ed.New York: Churchill Livingstone;1996.17. Posnick JC, Rabinovich A, Richardson DT. Blood replacement practices for complex orthognathic surgery: a single surgeon's experience. J Oral Maxillofac Surg. 2010; 68:54–9.
Article18. Dickerson HS, White RP Jr, McMichael DL, Turvey TA, Phillips C, Mohorn DJ. Recovery following orthognathic surgery: mandibular bilateral sagittal split osteotomy and Le fort I osteotomy. Int J Adult Orthodon Orthognath Surg. 1993; 8:237–43.19. Mohorn DJ, Vande Berg B, White RP Jr. Recovery of red blood cell mass following orthognathic surgery. Int J Adult Orthodon Orthognath Surg. 1995; 10:7–13.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Blood Loss And Hematologic Change After Orthognathic Surgery
- A clinical study of the blood loss and transfusion on orthognathic surger
- A hematologic study of orthognathic surgery patients
- Changes in temporo-mandibular disorders following the orthognathic surgeries
- Adjunctive facial contouring surgery in combination with orthognathic surgery