Korean J Physiol Pharmacol.
2011 Jun;15(3):163-169. 10.4196/kjpp.2011.15.3.163.
Direct Corticosteroid Modulation of GABAergic Neurons in the Anterior Hypothalamic Area of GAD65-eGFP Mice
- Affiliations
-
- 1Laboratory of Veterinary Pharmacology, College of Veterinary Medicine and Research Institute for Veterinary Science, Seoul National University, Seoul 151-742, Korea. pdryu@snu.ac.kr
- 2Department of Oral Physiology and BK21 Program, School of Dentistry and Institute of Oral Bioscience, Chonbuk National University, Jeonju 561-756, Korea.
- 3Department of Physiology, School of Medicine, Chungnam National University, Daejeon 301-747, Korea.
- 4Laboratory of Molecular Biology and Genetics, Institute of Experimental Medicine, 1450 Budapest, Hungary.
- KMID: 1448920
- DOI: http://doi.org/10.4196/kjpp.2011.15.3.163
Abstract
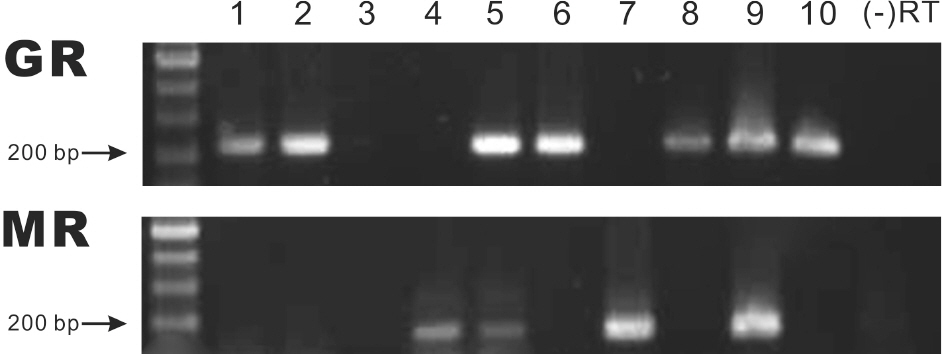
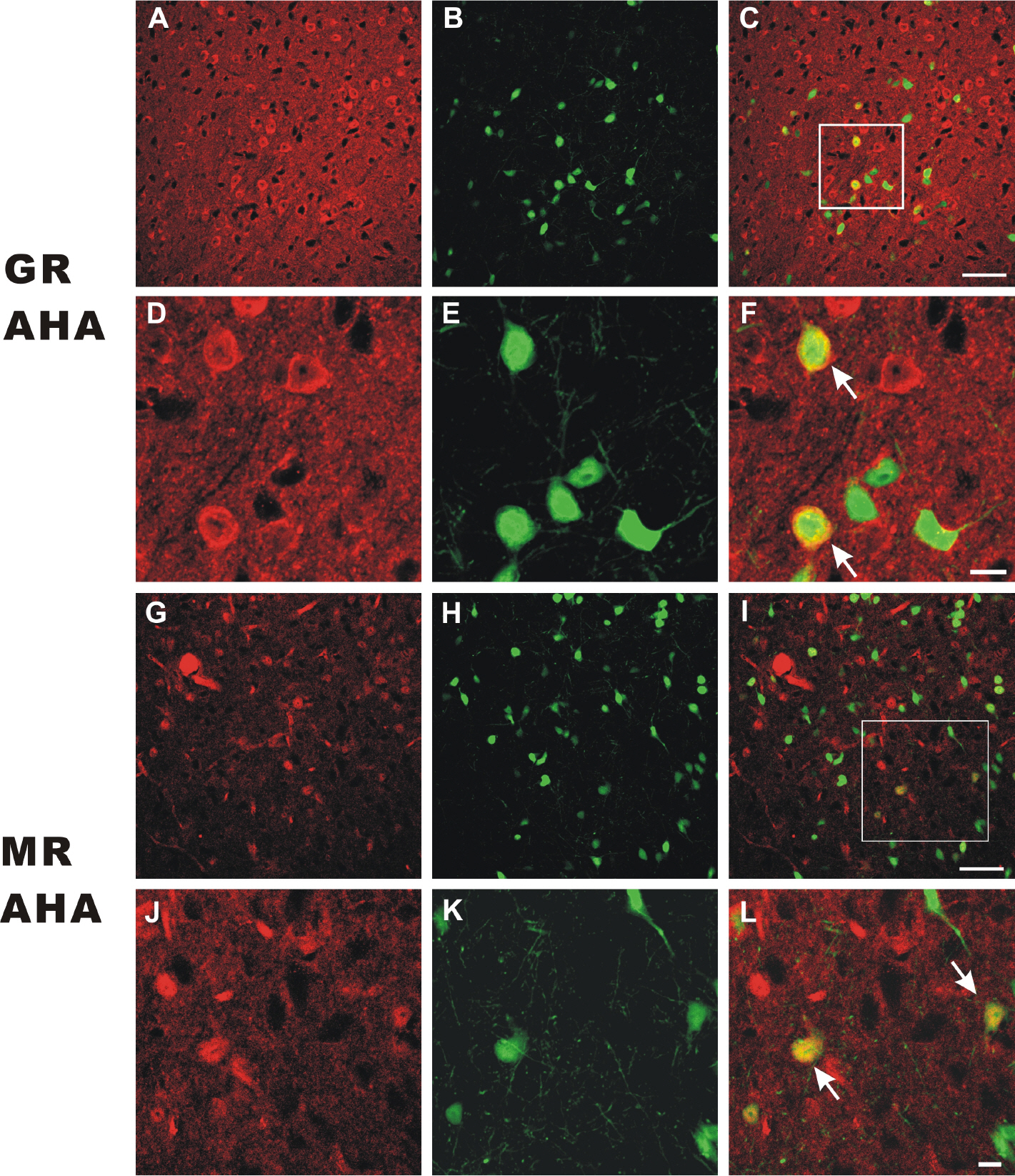
- Corticosterone is known to modulate GABAergic synaptic transmission in the hypothalamic paraventricular nucleus. However, the underlying receptor mechanisms are largely unknown. In the anterior hypothalamic area (AHA), the sympathoinhibitory center that project GABAergic neurons onto the PVN, we examined the expression of glucocorticoid receptor (GR) and mineralocorticoid receptor (MR) of GABAergic neurons using intact GAD65-eGFP transgenic mice, and the effects of corticosterone on the burst firing using adrenalectomized transgenic mice. GR or MR immunoreactivity was detected from the subpopulations of GABAergic neurons in the AHA. The AHA GABAergic neurons expressed mRNA of GR (42%), MR (38%) or both (8%). In addition, in brain slices incubated with corticosterone together with RU486 (MR-dominant group), the proportion of neurons showing a burst firing pattern was significantly higher than those in the slices incubated with vehicle, corticosterone, or corticosterone with spironolactone (GR-dominant group; 64 vs. 11~14%, p<0.01 by chi2-test). Taken together, the results show that the corticosteroid receptors are expressed on the GABAergic neurons in the AHA, and can mediate the corticosteroid-induced plasticity in the firing pattern of these neurons. This study newly provides the experimental evidence for the direct glucocorticoid modulation of GABAergic neurons in the AHA in the vicinity of the PVN.
Keyword
MeSH Terms
-
Animals
Anterior Hypothalamic Nucleus
Brain
Corticosterone
Fires
GABAergic Neurons
Mice
Mice, Transgenic
Mifepristone
Neurons
Paraventricular Hypothalamic Nucleus
Plastics
Receptors, Glucocorticoid
Receptors, Mineralocorticoid
Receptors, Steroid
RNA, Messenger
Spironolactone
Synaptic Transmission
Corticosterone
Mifepristone
Plastics
RNA, Messenger
Receptors, Glucocorticoid
Receptors, Mineralocorticoid
Receptors, Steroid
Spironolactone
Figure
Reference
-
References
1. De Kloet ER, Vreugdenhil E, Oitzl MS, Joëls M. Brain corticosteroid receptor balance in health and disease. Endocr Rev. 1998; 19:269–301.
Article2. de Kloet ER, Joëls M, Holsboer F. Stress and the brain: from adaptation to disease. Nat Rev Neurosci. 2005; 6:463–475.
Article3. Karst H, Berger S, Turiault M, Tronche F, Schütz G, Joëls M. Mineralocorticoid receptors are indispensable for nongenomic modulation of hippocampal glutamate transmission by corticosterone. Proc Natl Acad Sci USA. 2005; 102:19204–19207.
Article4. Di S, Malcher-Lopes R, Halmos KC, Tasker JG. Nongenomic glucocorticoid inhibition via endocannabinoid release in the hypothalamus: a fast feedback mechanism. J Neurosci. 2003; 23:4850–4857.
Article5. Herman JP, Cullinan WE, Ziegler DR, Tasker JG. Role of the paraventricular nucleus microenvironment in stress integration. Eur J Neurosci. 2002; 16:381–385.
Article6. Cullinan WE, Ziegler DR, Herman JP. Functional role of local GABAergic influences on the HPA axis. Brain Struct Funct. 2008; 213:63–72.
Article7. Roland BL, Sawchenko PE. Local origins of some GABAergic projections to the paraventricular and supraoptic nuclei of the hypothalamus in the rat. J Comp Neurol. 1993; 332:123–143.
Article8. Cullinan WE, Herman JP, Watson SJ. Ventral subicular interaction with the hypothalamic paraventricular nucleus: evidence for a relay in the bed nucleus of the stria terminalis. J Comp Neurol. 1993; 332:1–20.
Article9. Miklós IH, Kovács KJ. GABAergic innervation of corticotropin-releasing hormone (CRH)-secreting parvocellular neurons and its plasticity as demonstrated by quantitative immunoelectron microscopy. Neuroscience. 2002; 113:581–592.
Article10. Yang JH, Li LH, Lee S, Jo IH, Lee SY, Ryu PD. Effects of adrenalectomy on the excitability of neurosecretory parvocellular neurones in the hypothalamic paraventricular nucleus. J Neuroendocrinol. 2007; 19:293–301.
Article11. Yang JH, Li LH, Shin SY, Lee S, Lee SY, Han SK, Ryu PD. Adrenalectomy potentiates noradrenergic suppression of GABA-ergic transmission in parvocellular neurosecretory neurons of hypothalamic paraventricular nucleus. J Neurophysiol. 2008; 99:514–523.
Article12. Verkuyl JM, Joëls M. Effect of adrenalectomy on miniature inhibitory postsynaptic currents in the paraventricular nucleus of the hypothalamus. J Neurophysiol. 2003; 89:237–245.
Article13. Verkuyl JM, Karst H, Joëls M. GABAergic transmission in the rat paraventricular nucleus of the hypothalamus is suppressed by corticosterone and stress. Eur J Neurosci. 2005; 21:113–121.
Article14. Verkuyl JM, Hemby SE, Joëls M. Chronic stress attenuates GABAergic inhibition and alters gene expression of parvo-cellular neurons in rat hypothalamus. Eur J Neurosci. 2004; 20:1665–1673.
Article15. Bali B, Erdélyi F, Szabó G, Kovács KJ. Visualization of stress-responsive inhibitory circuits in the GAD65-eGFP transgenic mice. Neurosci Lett. 2005; 380:60–65.
Article16. Shin SY, Yang JH, Lee H, Erdélyi F, Szabó G, Lee SY, Ryu PD. Identification of the adrenoceptor subtypes expressed on GABAergic neurons in the anterior hypothalamic area and rostral zona incerta of GAD65-eGFP transgenic mice. Neurosci Lett. 2007; 422:153–157.
Article17. Oparil S, Chen YF, Peng N, Wyss JM. Anterior hypothalamic norepinephrine, atrial natriuretic peptide, and hypertension. Front Neuroendocrinol. 1996; 17:212–246.
Article18. Kim E, Seo S, Chung H, Park S. Role of glucocorticoids in fasting-induced changes in hypothalamic and pituitary components of the growth hormone (GH)-axis. Korean J Physiol Pharmacol. 2008; 12:217–223.
Article19. Han TH, Lee K, Park JB, Ahn D, Park JH, Kim DY, Stern JE, Lee SY, Ryu PD. Reduction in synaptic GABA release contributes to target-selective elevation of PVN neuronal activity in rats with myocardial infarction. Am J Physiol Regul Integr Comp Physiol. 2010; 299:R129–139.
Article20. Krugers HJ, Alfarez DN, Karst H, Parashkouhi K, van Gemert N, Joëls M. Corticosterone shifts different forms of synaptic potentiation in opposite directions. Hippocampus. 2005; 15:697–703.
Article21. Goldberg JH, Lacefield CO, Yuste R. Global dendritic calcium spikes in mouse layer 5 low threshold spiking interneurones: implications for control of pyramidal cell bursting. J Physiol. 2004; 558:465–478.
Article22. Kawaguchi Y, Shindou T. Noradrenergic excitation and inhibition of GABAergic cell types in rat frontal cortex. J Neurosci. 1998; 18:6963–6976.
Article23. Kim D, Song I, Keum S, Lee T, Jeong MJ, Kim SS, McEnery MW, Shin HS. Lack of the burst firing of thalamocortical relay neurons and resistance to absence seizures in mice lacking alpha(1G) T-type Ca(2+) channels. Neuron. 2001; 31:35–45.24. Perez-Reyes E. Molecular physiology of low-voltage-activated t-type calcium channels. Physiol Rev. 2003; 83:117–161.
Article25. Lee S, Han TH, Sonner PM, Stern JE, Ryu PD, Lee SY. Molecular characterization of T-type Ca(2+) channels responsible for low threshold spikes in hypothalamic paraventricular nucleus neurons. Neuroscience. 2008; 155:1195–1203.
Article26. Lalevée N, Rebsamen MC, Barrére-Lemaire S, Perrier E, Nargeot J, Bénitah JP, Rossier MF. Aldosterone increases T-type calcium channel expression and in vitro beating frequency in neonatal rat cardiomyocytes. Cardiovasc Res. 2005; 67:216–224.27. Lesouhaitier O, Chiappe A, Rossier MF. Aldosterone increases T-type calcium currents in human adrenocarcinoma (H295R) cells by inducing channel expression. Endocrinology. 2001; 142:4320–4330.
Article28. Rossier MF, Lesouhaitier O, Perrier E, Bockhorn L, Chiappe A, Lalevée N. Aldosterone regulation of T-type calcium channels. J Steroid Biochem Mol Biol. 2003; 85:383–388.
Article29. Beurrier C, Congar P, Bioulac B, Hammond C. Subthalamic nucleus neurons switch from single-spike activity to burst-firing mode. J Neurosci. 1999; 19:599–609.
Article30. Zhan XJ, Cox CL, Rinzel J, Sherman SM. Current clamp and modeling studies of low-threshold calcium spikes in cells of the cat's lateral geniculate nucleus. J Neurophysiol. 1999; 81:2360–2373.
Article31. Bessaïh T, Leresche N, Lambert RC. T current potentiation increases the occurrence and temporal fidelity of synaptically evoked burst firing in sensory thalamic neurons. Proc Natl Acad Sci USA. 2008; 105:11376–11381.32. Herman JP, Tasker JG, Ziegler DR, Cullinan WE. Local circuit regulation of paraventricular nucleus stress integration: glutamate-GABA connections. Pharmacol Biochem Behav. 2002; 71:457–468.33. Borkowski KR, Finch L. Cardiovascular changes in anaesthetised rats after the intra-hypothalamic administration of adrenaline. Clin Exp Hypertens. 1978; 1:279–291.
Article34. Pitts DK, Beuthin FC, Commissaris RL. Cardiovascular effects of perfusion of the rostral rat hypothalamus with clonidine: differential interactions with prazosin and yohimbine. Eur J Pharmacol. 1986; 124:67–74.
Article35. Poole S. Cardiovascular responses of rats to intrahypothalamic injection of carbachol and noradrenaline. Br J Pharmacol. 1983; 79:693–700.
Article36. Wyss JM, Chen YF, Jin H, Gist R, Oparil S. Spontaneously hypertensive rats exhibit reduced hypothalamic noradrenergic input after NaCl loading. Hypertension. 1987; 10:313–320.
Article37. Chen YF, Meng QC, Wyss JM, Jin H, Oparil S. High NaCl diet reduces hypothalamic norepinephrine turnover in hypertensive rats. Hypertension. 1988; 11:55–62.
Article38. Yang RH, Jin H, Chen SJ, Wyss JM, Oparil S. Blocking hypothalamic AT1 receptors lowers blood pressure in salt-sensitive rats. Hypertension. 1992; 20:755–762.
Article39. Oparil S, Yang RH, Jin HG, Chen SJ, Meng QC, Berecek KH, Wyss JM. Role of anterior hypothalamic angiotensin II in the pathogenesis of salt sensitive hypertension in the spontaneously hypertensive rat. Am J Med Sci. 1994; 307 Suppl. 1:S26–37.40. Kubo T, Yamaguchi H, Tsujimura M, Hagiwara Y, Fukumori R. An angiotensin system in the anterior hypothalamic area anterior is involved in the maintenance of hypertension in spontaneously hypertensive rats. Brain Res Bull. 2000; 52:291–296.
Article41. Kvetnanský R, Pacák K, Fukuhara K, Viskupic E, Hiremagalur B, Nankova B, Goldstein DS, Sabban EL, Kopin IJ. Sympathoadrenal system in stress. Interaction with the hypothalamicpituitary-adrenocortical system. Ann N Y Acad Sci. 1995; 771:131–158.42. Usuku T, Nishi M, Morimoto M, Brewer JA, Muglia LJ, Sugimoto T, Kawata M. Visualization of glucocorticoid receptor in the brain of green fluorescent protein-glucocorticoid receptor knockin mice. Neuroscience. 2005; 135:1119–1128.
Article43. Ito T, Morita N, Nishi M, Kawata M. In vitro and in vivo immunocytochemistry for the distribution of mineralocorticoid receptor with the use of specific antibody. Neurosci Res. 2000; 37:173–182.44. Han F, Ozawa H, Matsuda K, Nishi M, Kawata M. Colocalization of mineralocorticoid receptor and glucocorticoid receptor in the hippocampus and hypothalamus. Neurosci Res. 2005; 51:371–381.
Article45. Sarabdjitsingh RA, Meijer OC, de Kloet ER. Specificity of glucocorticoid receptor primary antibodies for analysis of receptor localization patterns in cultured cells and rat hippocampus. Brain Res. 2010; 1331:1–11.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Dopaminergic Neurons in the Diencephalon of Striped Field Mouse[Apodemus agrarius coreae]
- Coexistence of Tyrosine Hydroxylase and Nicotinamide Adenine Dinucleotide Phosphate-Diaphorase in Hypothalamic Neurons of the Rat
- Aucubin Promotes Differentiation of Neural Precursor Cells into GABAergic Neurons
- GABAergic neuronal development in the embryonic mesencephalon of mice
- Muscarine M2 Receptor-mediated Presynaptic Inhibition of GABAergic Transmission in Rat Meynert Neurons