J Korean Surg Soc.
2011 Dec;81(6):408-413. 10.4174/jkss.2011.81.6.408.
Percutaneous ilioinguinal-iliohypogastric nerve block or step-by-step local infiltration anesthesia for inguinal hernia repair: what cadaveric dissection says?
- Affiliations
-
- 1Department of Surgery, Diskapi Yildirim Beyazit Teaching and Research Hospital, Ankara, Turkey. hakankulacoglu@hotmail.com
- 2Department of Anatomy, Ankara University School of Medicine, Ankara, Turkey.
- 3Department of Anesthesiology, Diskapi Yildirim Beyazit Teaching and Research Hospital, Ankara, Turkey.
- KMID: 1445770
- DOI: http://doi.org/10.4174/jkss.2011.81.6.408
Abstract
- PURPOSE
The repair of groin hernias with local anesthesia has gained popularity. Two main methods have been described for local anesthesia. This study was aimed at comparing percutaneous truncular ilioinguinal-iliohypogastric block and step-by-step infiltration technique by using cadaver dissections.
METHODS
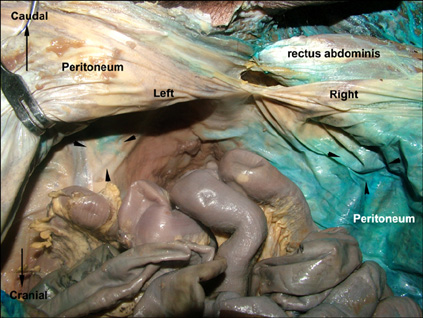
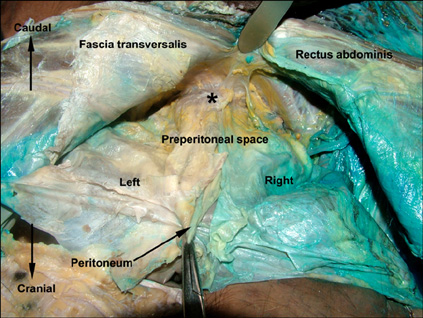
The study was performed on an adult male cadaver by using blue dye injection. A percutaneous nerve block simulation was done on right side and the dye was given in between the internal oblique and transversus muscles. On the left side, a skin incision was deepened and the dye was injected under the external oblique aponeurosis. Following the injections, stained areas were investigated superficially and within the deeper tissues with dissection.
RESULTS
There was a complete superficial staining covering the iliohypogastric and ilioinguinal nerves in the inguinal floor at both sides. On the right side, intraabdominal observation showed a wide and intense peritoneal staining, while almost no staining was seen on the left side. Preperitoneal dissection displayed a massive staining including testicular vascular pedicule and vas deferens on the right side. The dye solution also infiltrated the area of the femoral nerve prominently. On the contrary, a very limited staining was seen on the left.
CONCLUSION
It may not always be easy to keep the percutaneous block within optimum anatomical limits without causing adverse events. A step-by-step infiltration technique under direct surgical vision seems to be safer than percutaneous inguinal block for patients undergoing inguinal hernia repair.
MeSH Terms
Figure
Reference
-
1. Bowen JR, Thompson WR, Dorman BA, Soderberg CH Jr, Shahinian TK. Change in the management of adult groin hernia. Am J Surg. 1978. 135:564–569.2. Shoeibi G, Babakhani B, Mohammadi SS. The efficacy of ilioinguinal-iliohypogastric and intercostal nerve co-blockade for postoperative pain relief in kidney recipients. Anesth Analg. 2009. 108:330–333.3. Oriola F, Toque Y, Mary A, Gagneur O, Beloucif S, Dupont H. Bilateral ilioinguinal nerve block decreases morphine consumption in female patients undergoing nonlaparoscopic gynecologic surgery. Anesth Analg. 2007. 104:731–734.4. Bugedo GJ, Cárcamo CR, Mertens RA, Dagnino JA, Muñoz HR. Preoperative percutaneous ilioinguinal and iliohypogastric nerve block with 0.5% bupivacaine for post-herniorrhaphy pain management in adults. Reg Anesth. 1990. 15:130–133.5. Molloy RE. Benzon HT, Raja SN, Molloy RE, Liu SS, Fishman SM, editors. Truncal blocks: intercostal, paravertebral, interpleural, suprascapular, ilioinguinal, and iliohypogastric nevre blocks. Essentials of pain medicine and regional anesthesia. 2005. 2nd ed. Philadelphia: Elsevier-Churchill Livingstone;636–644.6. Weintraud M, Marhofer P, Bösenberg A, Kapral S, Willschke H, Felfernig M, et al. Ilioinguinal/iliohypogastric blocks in children: where do we administer the local anesthetic without direct visualization? Anesth Analg. 2008. 106:89–93. table of contents.7. Hu P, Harmon D, Frizelle H. Ultrasound guidance for ilioinguinal/iliohypogastric nerve block: a pilot study. Ir J Med Sci. 2007. 176:111–115.8. van Schoor AN, Boon JM, Bosenberg AT, Abrahams PH, Meiring JH. Anatomical considerations of the pediatric ilioinguinal/iliohypogastric nerve block. Paediatr Anaesth. 2005. 15:371–377.9. Lim SL, Ng Sb A, Tan GM. Ilioinguinal and iliohypogastric nerve block revisited: single shot versus double shot technique for hernia repair in children. Paediatr Anaesth. 2002. 12:255–260.10. Amory C, Mariscal A, Guyot E, Chauvet P, Leon A, Poli-Merol ML. Is ilioinguinal/iliohypogastric nerve block always totally safe in children? Paediatr Anaesth. 2003. 13:164–166.11. Jöhr M, Sossai R. Colonic puncture during ilioinguinal nerve block in a child. Anesth Analg. 1999. 88:1051–1052.12. Lehmann JM, Beckermann S. Transient femoral nerve palsy complicating preoperative ilioinguinal nerve blockade for inguinal herniorrhaphy. Br J Surg. 1995. 82:853.13. Greig JD, McArdle CS. Transient femoral nerve palsy complicating preoperative ilioinguinal nerve blockade for inguinal herniorrhaphy. Br J Surg. 1994. 81:1829.14. Rosario DJ, Skinner PP, Raftery AT. Transient femoral nerve palsy complicating preoperative ilioinguinal nerve blockade for inguinal herniorrhaphy. Br J Surg. 1994. 81:897.15. Tsai TY, Huang YS, Tsai YC, Liu YC. Temporary femoral nerve palsy after ilioinguinal nerve blockade combined with splash block for post-inguinal herniorrhaphy analgesia in a pediatric patient. Acta Anaesthesiol Taiwan. 2007. 45:237–240.16. Choi CJ, Park KJ, Kim SH. Comparison of three types of hernioplasty using meshes for adult inguinal hernia: lichtenstein, mesh-plug, prolene hernia system. J Korean Surg Soc. 2009. 76:109–114.17. Kurzer M, Belsham PA, Kark AE. The Lichtenstein repair for groin hernias. Surg Clin North Am. 2003. 83:1099–1117.18. Park CY, Hur YH, Kim JC, Kim SK. Clinical characteristics of incarcerated inguinal hernias of the greater omentum. J Korean Surg Soc. 2009. 77:50–53.19. Amid PK, Shulman AG, Lichtenstein IL. Local anesthesia for inguinal hernia repair step-by-step procedure. Ann Surg. 1994. 220:735–737.20. Ghani KR, McMillan R, Paterson-Brown S. Transient femoral nerve palsy following ilio-inguinal nerve blockade for day case inguinal hernia repair. J R Coll Surg Edinb. 2002. 47:626–629.21. Weintraud M, Lundblad M, Kettner SC, Willschke H, Kapral S, Lönnqvist PA, et al. Ultrasound versus landmark-based technique for ilioinguinal-iliohypogastric nerve blockade in children: the implications on plasma levels of ropivacaine. Anesth Analg. 2009. 108:1488–1492.22. Thibaut D, de la Cuadra-Fontaine JC, Bravo MP, de la Fuente R. Ilioinguinal/iliohypogastric blocks: where is the anesthetic injected? Anesth Analg. 2008. 107:728–729.23. Willschke H, Bösenberg A, Marhofer P, Johnston S, Kettner S, Eichenberger U, et al. Ultrasonographic-guided ilioinguinal/iliohypogastric nerve block in pediatric anesthesia: what is the optimal volume? Anesth Analg. 2006. 102:1680–1684.24. Eichenberger U, Greher M, Kirchmair L, Curatolo M, Moriggl B. Ultrasound-guided blocks of the ilioinguinal and iliohypogastric nerve: accuracy of a selective new technique confirmed by anatomical dissection. Br J Anaesth. 2006. 97:238–243.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Comparison between Ilioinguinal and Iliohypogastric Nerve Block and Infiltration of Local Anesthetics for Postoperative Pain after Inguinal Herniorrhaphy in Children
- Utility of ultrasound-guided transversus abdominis plane block for day-case inguinal hernia repair
- Ilioinguinal and Iliohypogastric Nerve Block for Neuropathic Pain Following the Laparoscopic Surgery
- Continuous Ilioinguinal-iliohypogastric Nerve Block for Groin Pain in a Breast-feeding Patient after Cesarean Delivery
- Diagnosis of Ilioinguinal Nerve Injury Based on Electromyography and Ultrasonography: A Case Report