J Korean Surg Soc.
2011 Oct;81(4):281-286. 10.4174/jkss.2011.81.4.281.
Synchronous double primary cancers associated with a choledochal cyst and anomalous pancreaticobiliary ductal union
- Affiliations
-
- 1Department of Surgery, Yonsei University College of Medicine, Seoul, Korea. kskim88@yuhs.ac
- 2Department of Surgery, Korea University College of Medicine, Seoul, Korea.
- 3Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea.
- 4Department of Pathology, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 1445750
- DOI: http://doi.org/10.4174/jkss.2011.81.4.281
Abstract
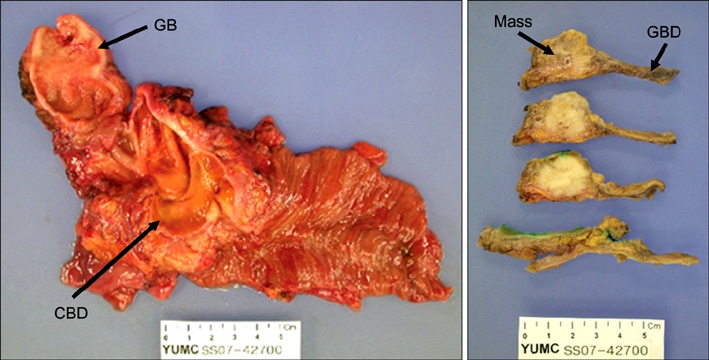
- A 60-year-old female was admitted with epigastric pain lasting a month. Preoperative diagnosis was choledochal cyst with anomalous pancreaticobiliaryductal union (APBDU), C-P type. A papillary mass measuring 2.5 x 1.9 cm was found adjacent to the pancreaticocholedochal junction. Gallbladder (GB) cancer was also observed. Pyloric-preserving pancreaticoduodenectomy (PPPD) was performed. The patient received adjuvant chemotherapy/radiation therapy on the tumor bed. The gallbladder cancer showed serosal invasion, while the bile duct cancer extended into the pancreas. Although common bile duct (CBD) cancer lesion showed focally positive for p53 and the gallbladder cancer lesion showed negative for p53, the Ki-67 labeling index of the CBD cancer and GB cancer were about 10% and 30%, respectively. Nine months after curative resection, a stricture on the subhepatic colon developed due to adjuvant radiation therapy. Localized peritoneal seedings were incidentally found during a right hemicolectomy. The patient underwent chemotherapy and had no evidence of tumor recurrence for two years after PPPD.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Intra-tumoral Metastatic Double Primary Carcinoma: Synchronous Metastatic Tumor in Lung from Breast and Thyroid Carcinoma
Lee Chun Park, Ji Yun Jeong, Jun Ho Ji, Silvia Park, Jin Seok Ahn, Young-Hyuck Im, Yeon Hee Park
Cancer Res Treat. 2014;46(2):200-203. doi: 10.4143/crt.2014.46.2.200.
Reference
-
1. The Japanese Study Group on Pancreaticobiliary Maljunction (JSPBM). The Committee of JSPBM for Diagnostic Criteria. Diagnostic criteria of pancreaticobiliary maljunction. J Hepatobiliary Pancreat Surg. 1994. 1:219–221.2. Yamaguchi M. Congenital choledochal cyst. Analysis of 1,433 patients in the Japanese literature. Am J Surg. 1980. 140:653–657.3. Funabiki T, Matsubara T, Miyakawa S, Ishihara S. Pancreaticobiliary maljunction and carcinogenesis to biliary and pancreatic malignancy. Langenbecks Arch Surg. 2009. 394:159–169.4. Sandoh N, Shirai Y, Hatakeyama K. Incidence of anomalous union of the pancreaticobiliary ductal system in biliary cancer. Hepatogastroenterology. 1997. 44:1580–1583.5. Jan YY, Chen HM, Chen MF. Malignancy in choledochal cysts. Hepatogastroenterology. 2002. 49:100–103.6. Kang CM, Kim KS, Choi JS, Lee WJ, Kim BR. Gallbladder carcinoma associated with anomalous pancreaticobiliary duct junction. Can J Gastroenterol. 2007. 21:383–387.7. Tashiro S, Imaizumi T, Ohkawa H, Okada A, Katoh T, Kawaharada Y, et al. Pancreaticobiliary maljunction: retrospective and nationwide survey in Japan. J Hepatobiliary Pancreat Surg. 2003. 10:345–351.8. Pitt HA. Gallbladder cancer: what is an aggressive approach? Ann Surg. 2005. 241:395–396.9. Cho SY, Kim SH, Park SJ, Han SS, Kim YK, Lee KW, et al. Adjuvant chemoradiation therapy in gallbladder cancer. J Surg Oncol. 2010. 102:87–93.10. Mondragón-Sánchez R, González-Geroniz M, Oñate-Ocaña LF, Garduño-López AL, Mondragón-Sánchez A, Bernal-Maldonado R, et al. A retrospective analysis of patients with gallbladder cancer treated with radical resection versus cholecystectomy plus external radiotherapy. Hepatogastroenterology. 2003. 50:1806–1810.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Choledochal Cyst with Anomalous Pancreaticobiliary Ductal Union
- Clinical Significance of Anomalous Pancreaticobiliary Ductal Union Diagnosed by Endoscopic Retrograde Cholangiopancreatography
- A Case of Choledochal Cyst (Type IVa) and Anomalous Pancreaticobiliary Ductal Union Combined with Pancreatic Duct Stone
- Biliary Intraepithelial Neoplasia (BilIN) Diagnosed From Choledochal Cyst in 7-Year-Old Girl With Underlying Anomalous Pancreaticobiliary Ductal Union (APBDU)
- Gallbladder Cancer Associated with an Anomalous Union of the Pancreaticobiliary Duct and a Choledochal Cyst