J Korean Bone Joint Tumor Soc.
2011 Dec;17(2):65-72. 10.5292/jkbjts.2011.17.2.65.
How to Overcome Complications of Allograft Transplantation?
- Affiliations
-
- 1Department of Orthopedic Surgery, Armed Forces Capital Hospital, Seongnam, Korea.
- 2Department of Orthopaedic Surgery, Kosin University Gospel Hospital, Busan, Korea. jdkim@ns.kosinmed.or.kr
- KMID: 1444791
- DOI: http://doi.org/10.5292/jkbjts.2011.17.2.65
Abstract
- PURPOSE
We evaluated the complications of allograft reconstruction after a bone tumor resection, and reviewed literatures to overcome such complications.
MATERIALS AND METHODS
We retrospectively reviewed clinical records and radiographs of fifteen patients in whom reconstruction with allograft after bone tumor resection.
RESULTS
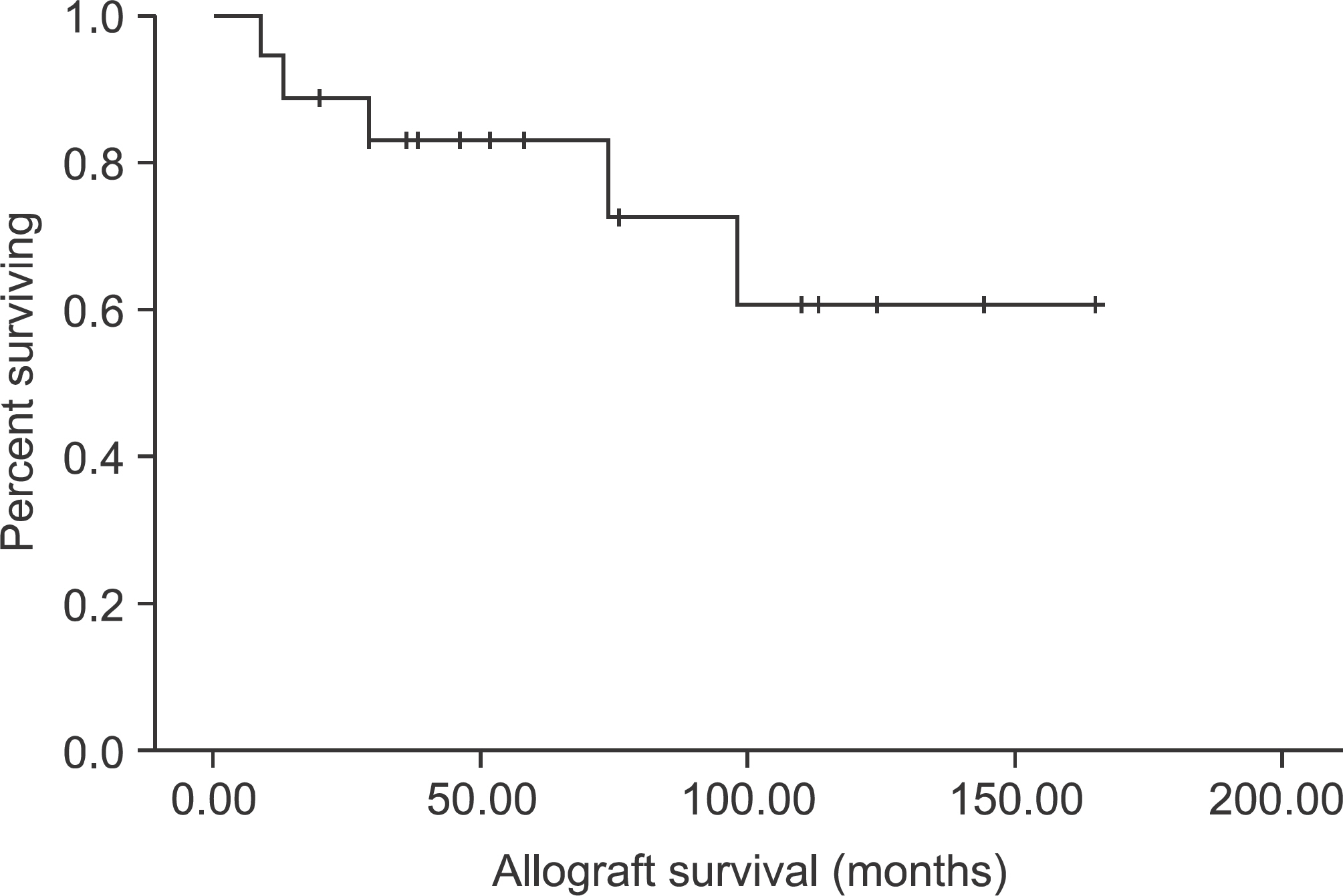
Eight patients were men and seven were women with a mean age of 27.1 years (1-56 years) and a mean follow-up period of 89.5 months (33-165 months). All postoperative complications related to the allograft were recorded. Twenty patients (80.0%) obtained a radiologic bony union at a mean of 8.35 months (4-12 months). The mean Musculoskeletal Tumor Society score was 73.5% (46.6-93.0%). Nine patients (60.0%) experienced one event and 3 (20.0%) patients experienced multiple events during the follow-up period. Recorded events were infection (3), fracture (2), nonunion (2), limb length discrepancy (2) and varus deformity (2). The mean event free survival period was 60.8 months (6-144 months). The mean allograft survival period was 80.2 months and the 5 year survival rate of the allografts was 83.0%.
CONCLUSION
In order to overcome complications, the combination of an allograft and vascularized fibular graft is highly recommended. In the near future, the tissue engineering technique, the application of the stem cell and PRP, could reduce the complication of allograft such as resorption and nonunion.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Donati D, Colangeli M, Colangeli S, Di Bella C, Mercuri M. Allograft-prosthetic composite in the proximal tibia after bone tumor resection. Clin Orthop Relat Res. 2008; 466:459–65.
Article2. Mankin HJ, Gebhardt MC, Jennings LC, Springfield DS, Tomford WW. Long-term results of allograft replacement in the management of bone tumors. Clin Orthop Relat Res. 1996. 86–97.
Article3. Hornicek FJ Jr, Mnaymneh W, Lackman RD, Exner GU, Malinin TI. Limb salvage with osteoarticular allografts after resection of proximal tibia bone tumors. Clin Orthop Relat Res. 1998; 352:179–86.
Article4. Ogilvie CM, Crawford EA, Hosalkar HS, King JJ, Lackman RD. Long-term results for limb salvage with osteoarticular allograft reconstruction. Clin Orthop Relat Res. 2009; 467:2685–90.
Article5. Prarrish F. Allograft replacement of all or part of the end of a long bone following excision of a tumor. J Bone Joint Surg Am. 1973; 55:1–22.6. Ottolenghi CE. Massive osteo and osteoarticular bone grafts. Technique and results of 62 cases. Clin Orthop Relat Res. 1972; 87:156–64.7. Muscolo DL, Ayerza MA, Aponte-Tinao LA. Long-term results of allograft replacement after total calcanectomy. A report of two cases. J Bone Joint Surg Am. 2000; 82:109–12.8. Getty PJ, Peabody TD. Complications and functional outcomes of reconstruction with an osteoarticular allograft after intraarticular resection of the proximal aspect of the humerus. J Bone Joint Surg Am. 1999; 81:1138–46.
Article9. Dick HM, Malinin TI, Mnaymneh WA. Massive allograft implantation following radical resection of high-grade tumors requiring adjuvant chemotherapy treatment. Clin Orthop Relat Res. 1985. 88–95.
Article10. Ward WG, Heise E, Boles C, et al. Human leukocyte antigen sensitization after structural cortical allograft implantations. Clin Orthop Relat Res. 2005. 31–5.
Article11. Giannini S, Vannini F, Lisignoli G, Facchini A. Histological and immunohistochemical analysis of an allogenic bone graft engineered with autologous bone marrow mononuclear cells in the treatment of a large segmental defect of the ulna. A case report. Chir Organi Mov. 2008; 91:171–5.
Article12. Myerson MS, Neufeld SK, Uribe J. Fresh-frozen structural allografts in the foot and ankle. J Bone Joint Surg Am. 2005; 87:113–20.
Article13. Eward WC, Kontogeorgakos V, Levin LS, Brigman BE. Free vascularized fibular graft reconstruction of large skeletal defects after tumor resection. Clin Orthop Relat Res. 2010; 468:590–8.
Article14. Heitmann C, Erdmann D, Levin LS. Treatment of segmental defects of the humerus with an osteoseptocutaneous fibular transplant. J Bone Joint Surg Am. 2002; 84A:2216–23.
Article15. Enneking WF, Spanier SS, Goodman MA. Current concepts review. The surgical staging of musculoskeletal sarcoma. J Bone Joint Surg Am. 1980; 62:1027–30.
Article16. Enneking WF, Dunham W, Gebhardt MC, Malawar M, Pritchard DJ. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res. 1993; 286:241–6.
Article17. Brigman BE, Hornicek FJ, Gebhardt MC, Mankin HJ. Allografts about the knee in young patients with high-grade sarcoma. Clin Orthop Relat Res. 2004; 421:232–9.
Article18. Fox EJ, Hau MA, Gebhardt MC, Hornicek FJ, Tomford WW, Mankin HJ. Long-term followup of proximal femoral allografts. Clin Orthop Relat Res. 2002; 397:106–13.
Article19. Muscolo DL, Ayerza MA, Aponte-Tinao LA. Survivorship and radiographic analysis of knee osteoarticular allografts. Clin Orthop Relat Res. 2000; 373:73–9.
Article20. Ortiz-Cruz E, Gebhardt MC, Jennings LC, Springfield DS, Mankin HJ. The results of transplantation of intercalary allografts after resection of tumors. A longterm follow-up study. J Bone Joint Surg Am. 1997; 79:97–106.
Article21. Capanna R, Bufalini C, Campanacci M. A new technique for reconstruction of large metadiaphyseal bone defects. A combined graft(allograft shell plus vascularized fibula). Orthop Traumatol. 1993; 2:159–77.22. Innocenti M, Abed YY, Beltrami G, Delcroix L, Manfrini M, Capanna R. Biological reconstruction after resection of bone tumors of the proximal tibia using allograft shell and intramedullary free vascularized fibular graft: longterm results. Microsurgery. 2009; 29:361–72.
Article23. Bae D, Waters P, Gebhardt M. Results of free vascularized fibula grafting for allograft nonunion after limb salvage surgery for malignant bone tumors. J Pediatr Orthop. 2006; 26:809–14.
Article24. Sorger JI, Hornicek F, Zavatta M, et al. Allograft fractures revisited. Clin Orthop Relat Res. 2001; 382:66–74.
Article25. Enneking WF, Campanacci DA. Retrieved human allografts: a clinicopathological study. J Bone Joint Surg Am. 2001; 83A:971–86.26. Lord CF, Gebhardt MC, Tomford WW, Mankin HJ. Infection in bone allografts: incidence, nature, and treatment. J Bone Joint Surg Am. 1988; 70:369–76.
Article27. Mnaymneh W, Malinin TI, Makley JT, Dick HM. Massive osteoarticular allografts in the reconstruction of extremities following resection of tumors not requiring chemotherapy and radiation. Clin Orthop Relat Res. 1985; 197:76–87.
Article28. Berrey BH Jr, Lord CF, Gebhardt MC, Mankin HJ. Fractures of allografts. Frequency, treatment, and end-results. J Bone Joint Surg Am. 1990; 72:825–33.
Article29. Vander Griend RA. The effect of internal fixation on the healing of large allografts. J Bone Joint Surg Am. 1994; 76:657–63.
Article30. Hornicek FJ, Gebhardt MC, Tomford WW, et al. Factors affecting nonunion of the allograft-host junction. Clin Orthop Relat Res. 2001; 382:87–98.
Article31. Ceruso M, Taddei F, Bigazzi P, Manfrini M. Vascularised fibula graft inlaid in a massive bone allograft: considerations on the biomechanical behaviour of the combined graft in segmental bone reconstructions after sarcoma resection. Injury. 2008; 39(Suppl 3):S68–74.
Article32. Friedrich JB, Moran SL, Bishop AT, Wood CM, Shin AY. Free vascularized fibular graft salvage of complications of long-bone allograft after tumor reconstruction. J Bone Joint Surg Am. 2008; 90:93–100.
Article33. Chang DW, Weber KL. Use of a vascularized fibula bone flap and intercalary allograft for diaphyseal reconstruction after resection of primary extremity bone sarcomas. Plast Reconstr Surg. 2005; 116:1918–25.
Article34. Chang DW, Weber KL. Segmental femur reconstruction using an intercalary allograft with an intramedullary vascularized fibula bone flap. J Reconstr Microsurg. 2004; 20:195–9.35. Moran SL, Shin AY, Bishop AT. The use of massive bone allograft with intramedullary free fibular flap for limb salvage in a paediatric and adolescent population. Plast Reconstr Surg. 2006; 118:413–9.36. Lucarelli E, Fini M, Beccheroni A, et al. Stromal stem cells and platelet-rich plasma improve bone allograft integraftion. Clin Orthop Relat Res. 2005; 435:62–8.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intraoperative Templating in Lateral Meniscal Allograft Transplantation
- Medical Complications of Lung Transplantation
- The worth emphasizing surgical technique: ureteropyelostomy to manage urinary tract complications
- Bone Reconstruction: Structural Allograft and Autograft
- Allograft Immune Reaction of Kidney Transplantation: Part 1. Mechanism of Allograft Rejection