J Korean Soc Radiol.
2011 Jul;65(1):53-59. 10.3348/jksr.2011.65.1.53.
Intracranial Stent Implantation for Drug Resistant Atherosclerotic Stenosis: Results of 52 Cases
- Affiliations
-
- 1Department of Radiology, Hallym University Hangang Sacred Heart Hospital, Seoul, Korea. mddhhwang@naver.com
- 2Department of Neurosurgery, Myungji St. Mari's Hospital, Seoul, Korea.
- KMID: 1443493
- DOI: http://doi.org/10.3348/jksr.2011.65.1.53
Abstract
- PURPOSE
We evaluated the usefulness of intracranial stent implantation for treatment of drug resistant atherosclerotic stenoses.
MATERIALS AND METHODS
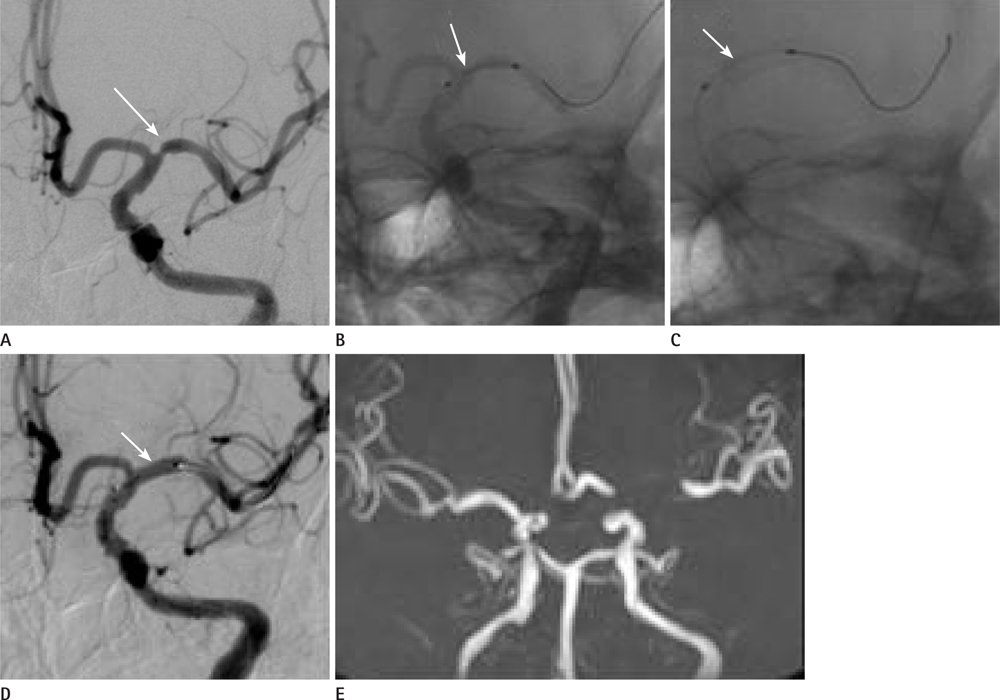
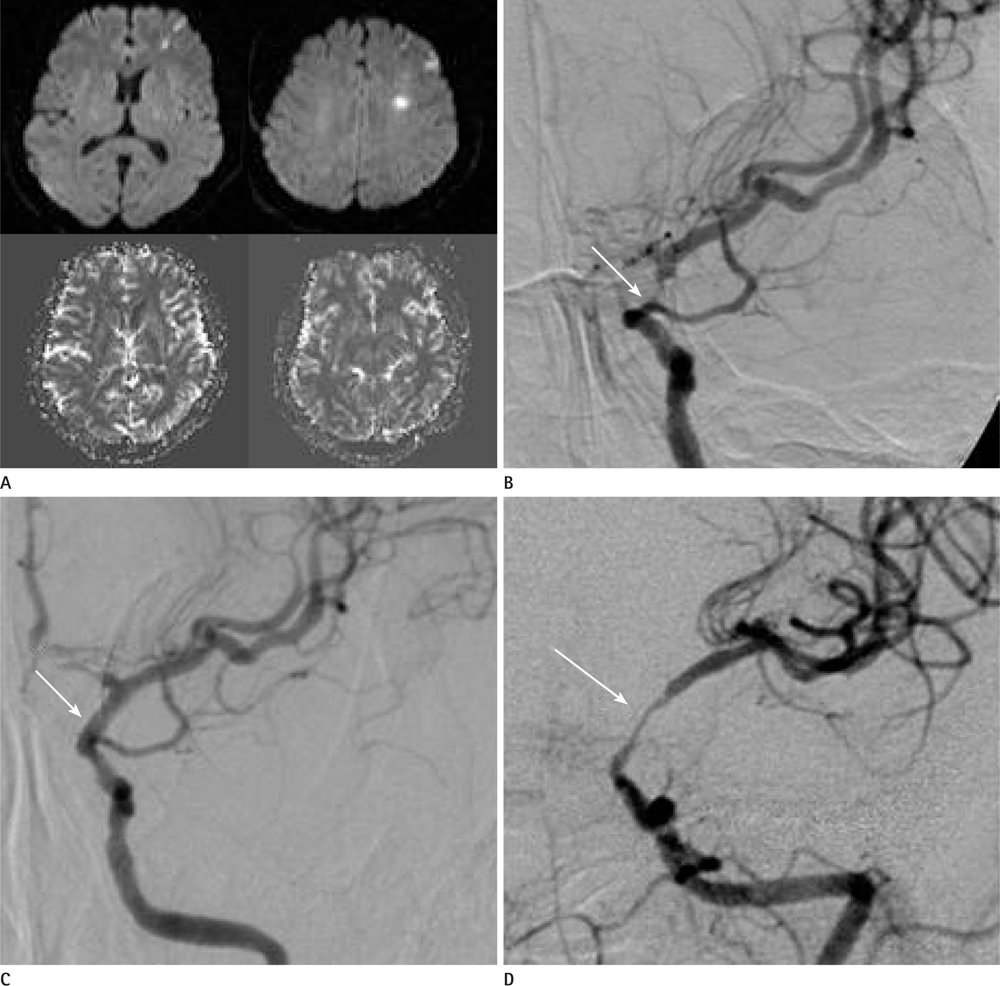
Between March 2004 and July 2007, we tried intracranial stent implantation in 49 patients with 52 lesions (anterior circulation 48 cases, posterior circulation 4 cases) who had an ischemic stroke with more than 50% of major cerebral artery stenosis. We classified the lesions by their location and morphology, analyzed the results in terms of the success rate, complication rate, and restenosis rate during the follow-up period.
RESULTS
Intracranial stent implantation was performed successfully in 43 cases (82.7%). In eight of the nine cases, the stent implantation failure was due to the tortuosity of the target vessel. There was no major periprocedural complication. One patient showed cerebellar infarction after the procedure. Mean residual stenoses decreased from 70.2% to 13.0%. Four cases (9.3%) demonstrated in-stent restenoses and more than 50% during the mean and 25.3/month after the follow-up period.
CONCLUSION
Success rate of intracranial stent implantation may improve on developing technique and more experience. Low rate of complication and restenosis suggest that we can consider intracranial stent implantation for treatment of drug resistant atherosclerotic stenoses.
MeSH Terms
Figure
Reference
-
1. Kim JS. Stroke in Korea. Int Congr Ser. 2004; 1262:348–351.2. Suh DC, Lee SH, Kim KR, Park ST, Lim SM, Kim SJ, et al. Pattern of atherosclerotic carotid stenosis in Korean patients with stroke: different involvement of intracranial versus extracranial vessels. AJNR Am J Neuroradiol. 2003; 24:239–244.3. Lylyk P, Cohen JE, Ceratto R, Ferrario A, Miranda C. Angioplasty and stent placement in intracranial atherosclerotic stenoses and dissections. AJNR Am J Neuroradiol. 2002; 23:430–436.4. Groschel K, Schnaudigel S, Pilgram SM, Wasser K, Kastrup A. A systematic review on outcome after stenting for intracranial atherosclerosis. Stroke. 2009; 40:e340–e347.5. Choi HW, Koo YB, Lee TH, Kim HJ, Lee JW, Kim CW, et al. New Techniques for Intracranial Stent Navigation in Patients with Tortuous Arteries. J Korean Radiol Soc. 2005; 52:101–106.6. Suh DC, Kim JK, Choi JW, Choi BS, Pyun HW, Choi YJ, et al. Intracranial stenting of severe symptomatic intracranial stenosis: results of 100 consecutive patients. AJNR Am J Neuroradiol. 2008; 29:781–785.7. Bogousslavsky J, Barnett HJ, Fox AJ, Hachinski VC, Taylor W. . Atherosclerotic disease of the middle cerebral artery. Stroke. 1986; 17:1112–1120.8. Failure of extracranial-intracranial arterial bypass to reduce the risk of ischemic stroke. Results of an international randomized trial. The EC/IC Bypass Study Group. N Engl J Med. 1985; 313:1191–1200.9. Chimowitz MI, Kokkinos J, Strong J, Brown MB, Levine SR, Silliman S, et al. The Warfarin-Aspirin Symptomatic Intracranial Disease Study. Neurology. 1995; 45:1488–1493.10. Thijs VN, Albers GW. Symptomatic intracranial atherosclerosis: outcome of patients who fail antithrombotic therapy. Neurology. 2000; 55:490–497.11. Mazighi M, Tanasescu R, Ducrocq X, Vicaut E, Bracard S, Houdart E, et al. Prospective study of symptomatic atherothrombotic intracranial stenoses: the GESICA study. Neurology. 2006; 66:1187–1191.12. Siddiq F, Vazquez G, Memon MZ, Suri MF, Taylor RA, Wojak JC, et al. Comparison of primary angioplasty with stent placement for treating symptomatic intracranial atherosclerotic diseases: a multicenter study. Stroke. 2008; 39:2505–2510.13. Marks MP, Marcellus ML, Do HM, Schraedley-Desmond PK, Steinberg GK, Tong DC, et al. Intracranial angioplasty without stenting for symptomatic atherosclerotic stenosis: long-term follow-up. AJNR Am J Neuroradiol. 2005; 26:525–530.14. Lylyk P, Ferrario A, Pasbon B, Miranda C, Doroszuk G. Buenos Aires experience with the Neuroform self-expanding stent for the treatment of intracranial aneurysms. J Neurosurg. 2005; 102:235–241.15. Marks MP, Marcellus M, Norbash AM, Steinberg GK, Tong D, Albers GW. Outcome of angioplasty for atherosclerotic intracranial stenosis. Stroke. 1999; 30:1065–1069.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Long-term outcomes of drug-eluting stent implantation in patients with symptomatic extra- and intracranial atherosclerotic stenoses
- Usefulness of Stent Implantation for Treatment of Intracranial Atherosclerotic Stenoses
- Wingspan Stenting for Symptomatic Severe In-Stent Stenosis of a Closed-Cell Stent after Stent-Assisted Coiling of a Ruptured Intracranial Aneurysm
- Use of Drug-Eluting Stent with Provisional T-Stenting Technique in the Treatment of Renal Artery Bifurcation Stenosis; Long-term Angiographic Follow-up
- In-Stent Stenosis of Stent Assisted Endovascular Treatment on Intracranial Complex Aneurysms