J Korean Soc Spine Surg.
2012 Sep;19(3):90-96. 10.4184/jkss.2012.19.3.90.
Incidentally Detected Concurrent Lower Thoracic Lesions in Extended Lumbar Spine MRI
- Affiliations
-
- 1Department of Orthopaedic Surgery, Chonnam National University Hospital, Gwangju, Korea.
- 2Department of Orthopaedic Surgery, Chonnam National University Hwasun Hospital, Jeonnam, Korea. presid50@naver.com
- KMID: 1435585
- DOI: http://doi.org/10.4184/jkss.2012.19.3.90
Abstract
- STUDY DESIGN: Retrospective study.
OBJECTIVES
To evaluate the prevalence and associated factors of the concurrent lower thoracic lesions in patients who have a lumbar spine disease, using the extended lumbar MRI. SUMMARY OF LITERATURE REVIEW: There are no studies regarding the concurrent thoracic lesions with lumbar disease.
MATERIALS AND METHODS
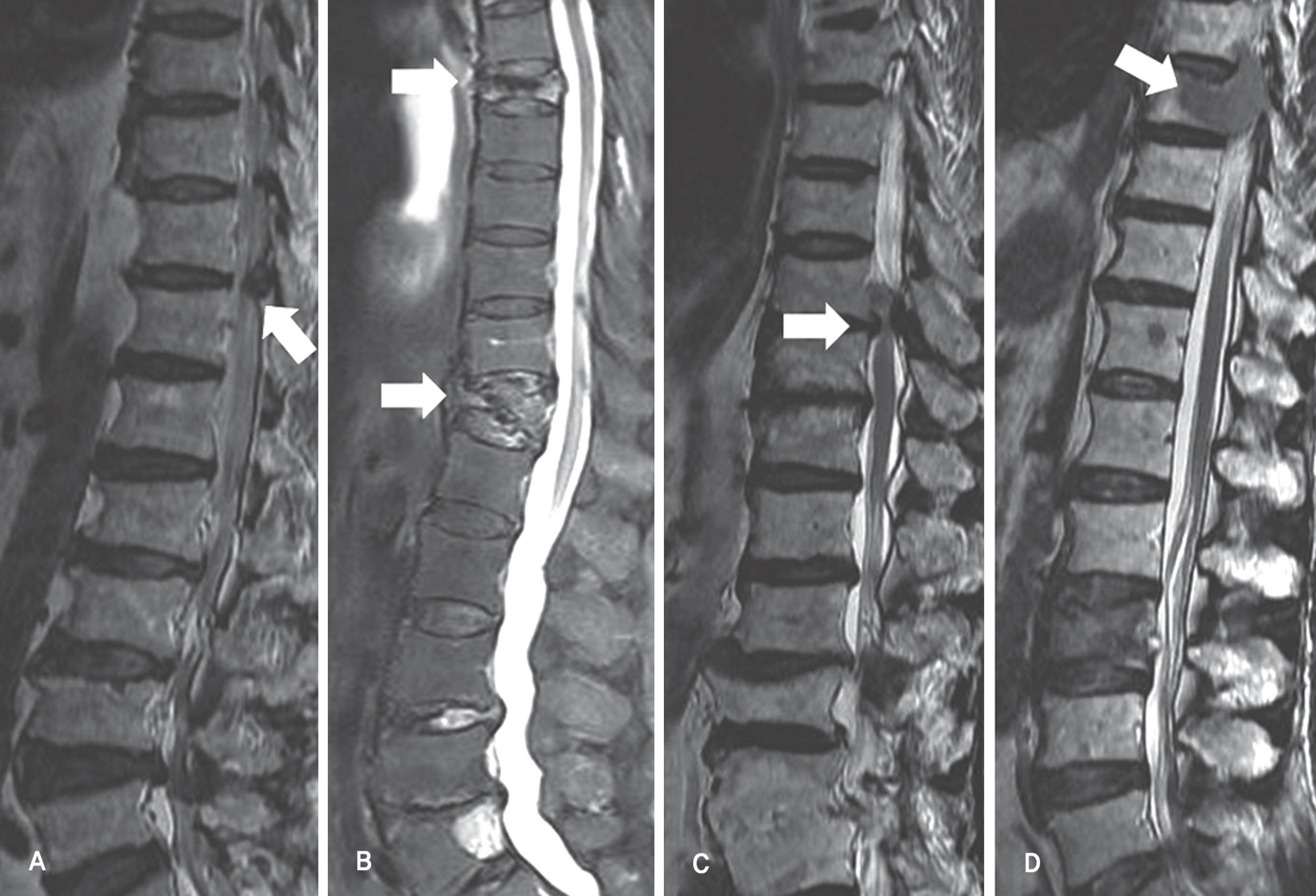
All the patients, who had visited the out-patient department (OPD) of orthopaedic surgery in our hospital and underwent lumbar spine MRI, were studied during 1 year. Totally, 750 patients were included. The extended lumbar spine MRI contained additional extended T2-weighted sagittal images that cover the lower thoracic vertebrae with 35 centimeters long. We analyzed the highest observable level, characteristics of detected thoracic lesions. Those lesions were classified according to the severity of compression of the spinal cord and investigation for associated factors of patients. Also, the times for additional tests were measured.
RESULTS
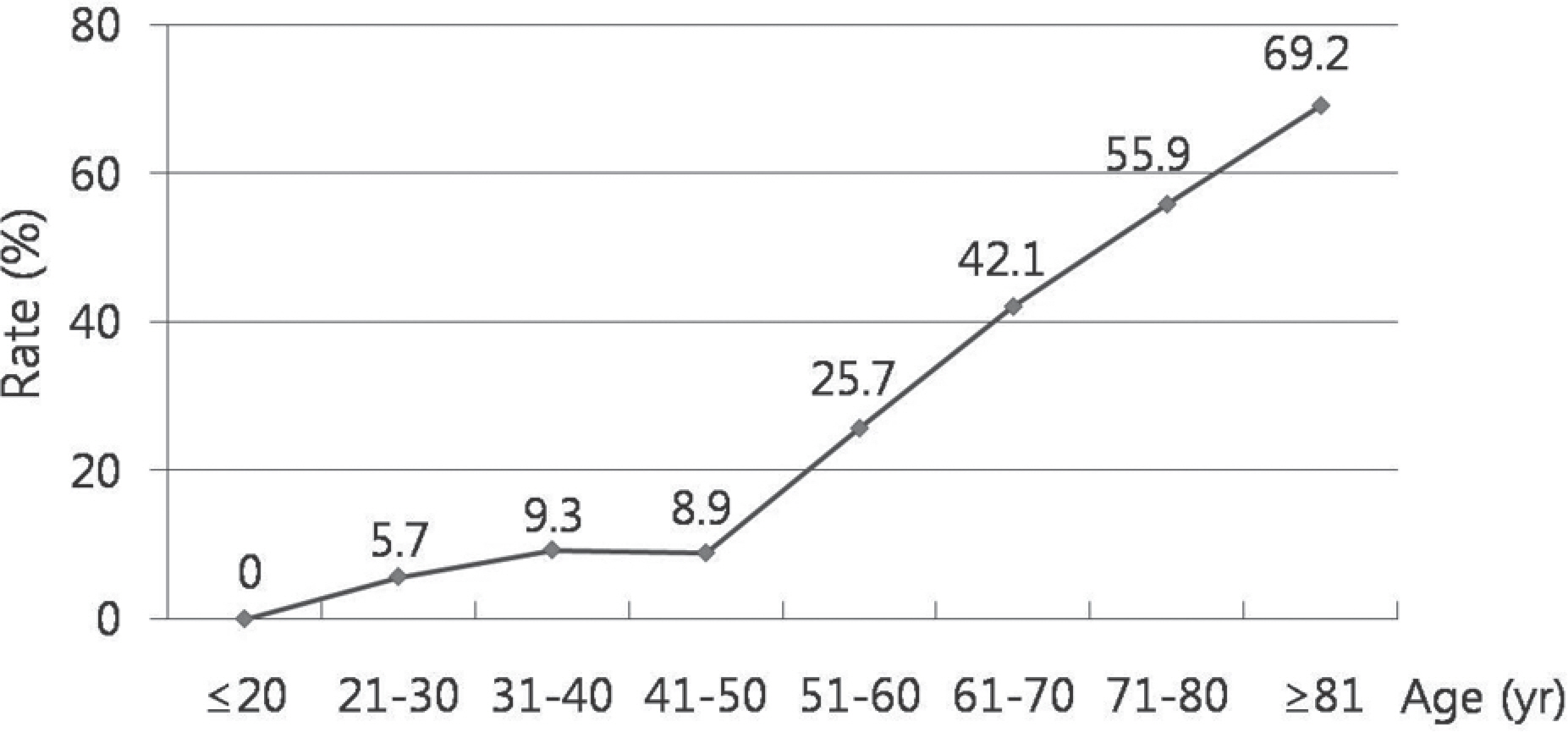
Additional tests were able to observe up to the 7th thoracic vertebrae. In 257 cases (34.3%), the lower thoracic lesions were detected and increased with aging (p<0.001). A total of 48 patients (6%) had the lesion compressing the spinal cord and 28 patients needed further evaluation for the lower thoracic lesion. Further, 2 cases were treated surgically for lower thoracic lesions. Scanning extra time for additional test were 3 minutes.
CONCLUSIONS
The prevalence of lower thoracic lesions accompanied with the lumbar disease was 34% in this study. Therefore, additional extended lumbar spine MRI is needed to check possible concurrent lesions in the lower thoracic spine.
Keyword
Figure
Reference
-
1.Epstein NE., Epstein JA., Carras R., Murthy VS., Hyman RA. Coexisting cervical and lumbar spinal stenosis: diagnosis and management. Neurosurgery. 1984. 15:489–96.
Article2.Smith DE., Godersky JC. Thoracic spondylosis: an unusual cause of myelopathy. Neurosurgery. 1987. 20:589–93.
Article3.Moon ES., Kim HS., Park JO, et al. The incidence of new vertebral compression fractures in women after kyphoplasty and factors involved. Yonsei Med J. 2007. 48:645–52.
Article4.Benoist M. Natural history of the aging spine. Eur Spine J. 2003. 12(Suppl):86–9.
Article5.Barnett GH., Hardy RW Jr., Little JR., Bay JW., Sypert GW. Thoracic spinal canal stenosis. J Neurosurg. 1987. 66:338–44.
Article6.Niemelainen R., Battie MC., Gill K., Videman T. The prevalence and characteristics of thoracic magnetic reso-nance imaging findings in men. Spine (Phila Pa 1976). 2008. 33:2552–9.7.Abhaykumar S., Tyagi A., Towns GM. Thoracic vertebral osteophyte-causing myelopathy: early diagnosis and treatment. Spine (Phila Pa 1976). 2002. 27:E334–6.
Article8.Bosacco SJ., Berman AT., Raisis LW., Zamarin RI. High lumbar disk herniations. Case reports. Orthopedics. 1989. 12:275–8.
Article9.Fukuta S., Miyamoto K., Iwata A, et al. Unusual back pain caused by intervertebral disc degeneration associated with schmorl node at Th11/12 in a young athlete, successfully treated by anterior interbody fusion: a case report. Spine (Phila Pa 1976). 2009. 34:E195–8.10.Okada Y., Shimizu K., Ido K., Kotani S. Multiple thoracic disc herniations: case report and review of the literature. Spinal Cord. 1997. 35:183–6.
Article11.Benjamin V. Diagnosis and management of thoracic disc disease. Clin Neurosurg. 1983. 30:577–605.
Article12.Chen CF., Chang MC., Liu CL., Chen TH. Acute noncontig-uous multiple-level thoracic disc herniations with myelopathy: a case report. Spine (Phila Pa 1976). 2004. 29:E157–60.13.Otani K., Yoshida M., Fujii E., Nakai S., Shibasaki K. Thoracic disc herniation. Surgical treatment in 23 patients. Spine (Phila Pa 1976). 1988. 13:1262–7.14.Fink HA., Milavetz DL., Palermo L, et al. What proportion of incident radiographic vertebral deformities is clinically di-agnosed and vice versa? J Bone Miner Res. 2005. 20:1216–22.
Article15.Lindsay R., Silverman SL., Cooper C, et al. Risk of new vertebral fracture in the year following a fracture. JAMA. 2001. 285:320–23.
Article16.Adachi JD., Adami S., Gehlbach S, et al. Impact of prevalent fractures on quality of life: baseline results from the global longitudinal study of osteoporosis in women. Mayo Clin Proc. 2010. 85:806–13.
Article17.Delmas PD., van de Langerijt L., Watts NB, et al. Underdi-agnosis of vertebral fractures is a worldwide problem: the IMPACT study. J Bone Miner Res. 2005. 20:557–63.
Article18.Bates D., Ruggieri P. Imaging modalities for evaluation of the spine. Radiol Clin North Am. 1991. 29:675–90.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Asymptomatic Cervical or Thoracic Lesions in Elderly Patients who Have Undergone Decompressive Lumbar Surgery for Stenosis
- The Value of Additional Cervicothoracic Spine Sagittal T2-weighted Images Included in Routine Lumbar Spine MR Imaging
- Clinical Utility of Limited T2-Weighted-Only Lumbar Spine MRI in Pain Intervention Clinics
- Paraplegia due to Missed Thoracic Meningioma after Laminotomy for Lumbar Spinal Stenosis: Report of Two Cases
- Coexisting Spine Lesions on Whole Spine T2 Sagittal MRI in Evaluating Spinal Degenerative Disease