J Korean Bone Joint Tumor Soc.
2012 Dec;18(2):104-108. 10.5292/jkbjts.2012.18.2.104.
Parosteal Lipoma of the Femur with Hyperostosis: A Case Report
- Affiliations
-
- 1Department of Orthopaedic Surgery, Sung-Ae Hospital, Seoul, Korea. osnoul@naver.com
- 2Department of Orthopaedic Surgery, Kwang-Myung Sung-Ae Hospital, Kwangmyung, Korea.
- KMID: 1431679
- DOI: http://doi.org/10.5292/jkbjts.2012.18.2.104
Abstract
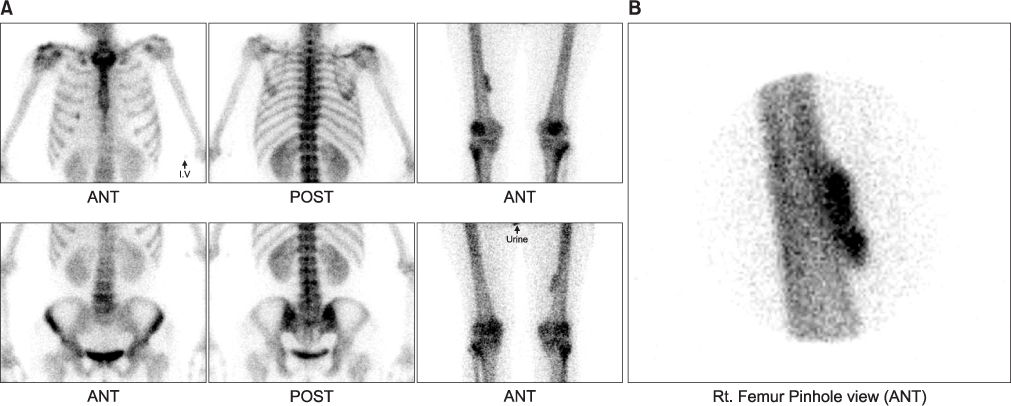
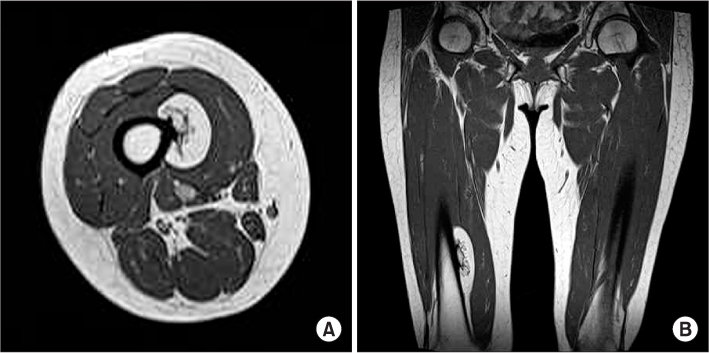
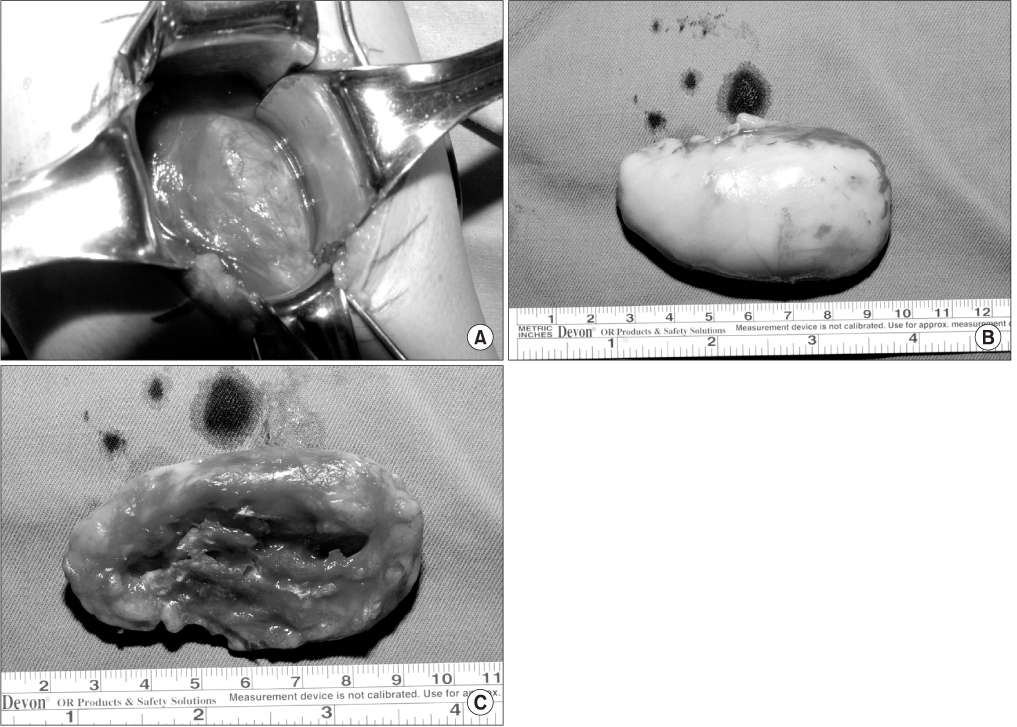
- Parosteal lipoma is a rare kind of lipoma that occurring adipous tissue around the periosteum. It has been reported most commonly in the femur, the radius, the tibia and the fibular. Treatment consists of resecting the lipomatous tumor with further exeresis of the bone and periosteal excrescence in cases with hyperostosis. The authors report a rare case of parosteal lipoma occurring at the medial portion of the femur shaft with a review of the relevant literatures.
Keyword
MeSH Terms
Figure
Reference
-
1. Fleming RJ, Alpert M, Garcia A. A parosteal lipoma. AJR. 1962. 87:1075–1084.2. Kim JY, Jung SL, Park YH, Park SH, Kang YK. Parosteal lipoma with hyperostosis. Eur Radiol. 1999. 9:1810–1812.3. Canale ST, Beaty JH. Campbell's operative orthopaedics. 2008. 11th ed. Philadelpia: Mosby;871.4. Moon N, Marmor L. Parostel lipoma of the proximal part of the radius. a clinical entity with frequent radial-nerve injury. J Bone Joint Surg Am. 1964. 46:608–614.5. Kong GM, Kim SH, Oh HK. Parosteal lipoma of the proximal radius causing posterior interosseous nerve palsy: a case report. J Korean Bone Joint Tumor Soc. 2009. 15:165–170.6. Power DA. Parosteal lipoma, or congenital fatty tumor, connected with periosteum of femur. Trans Pathol Soc, London. 1888. 39:270–272.7. Murphey MD, Johnson DL, Bhatia PS, Neff JR, Rosenthal HG, Walker CW. Parosteal lipoma: MR imaging characteristics. AJR Am J Roentgenol. 1994. 162:105–110.8. Rhee SK, Kang YK, Park WJ, Chung YG, Lee HJ. Parosteal lipoma with hyperostosis - two cases report. J Korean Bone Joint Tumor Soc. 2001. 10:105–109.9. Rodriguez-Peralto JL, Lopez-Barea F, Gonzalez-Lopez J, Lamas-Lorenzo M. Case report 821: Parosteal ossifying lipoma of femur. Skeletal Radiol. 1994. 23:67–69.10. Bispo Junior RZ, Guedes AV. Parosteal lipoma of the femur with hyperostosis: case report and literature review. Clinics (Sao Paulo). 2007. 62:647–652.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Parosteal Lipoma Associated with Underlying Recurrent Bizarre Parosteal Osteochondromatous Proliferation (Nora's Lesion) of the Hand
- Parosteal Lipoma of the Tibia: A Case Report
- Parosteal Ossifying Lipoma of Femur: A Case Report
- Parosteal Lipoma Associated with a Growing Osteochondroma of the Right Ilium
- Two cases of Parosteal Lipoma on the Forehead