Hip Pelvis.
2013 Mar;25(1):37-43. 10.5371/hp.2013.25.1.37.
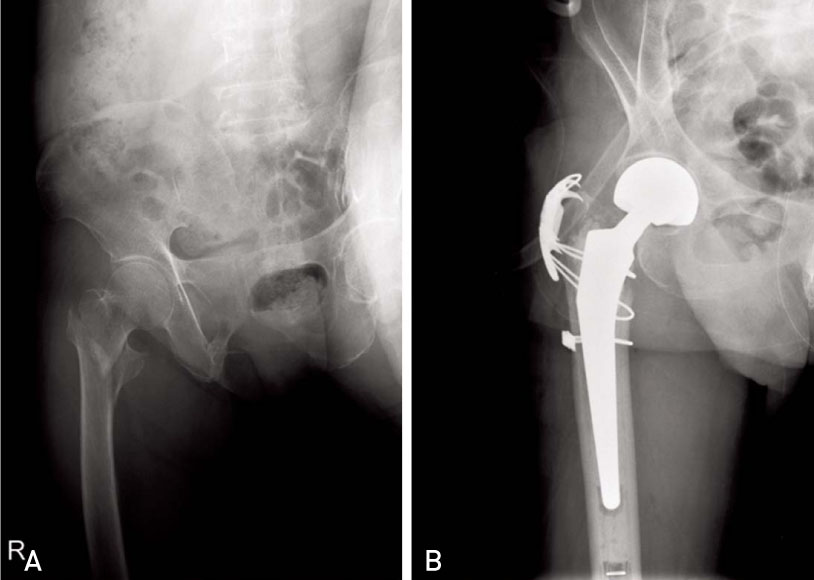
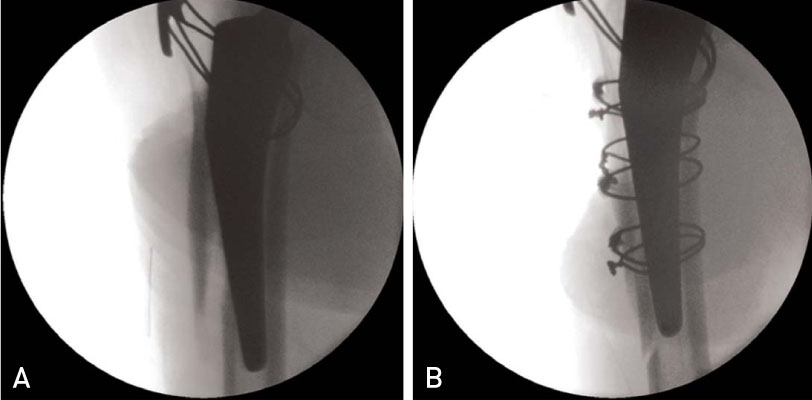
Comparison of Postoperative Bleeding and Complications between Cemented and Non-cemented Bipolar Hemiarthroplasty in Treatment of Unstable Pertrochanteric Fracture
- Affiliations
-
- 1Department of Orthopaedic Surgery, College of Medicine, The Catholic University of Korea, Daejeon, Korea. weonkim@hotmail.com
- KMID: 1425034
- DOI: http://doi.org/10.5371/hp.2013.25.1.37
Abstract
- PURPOSE
In cases of patients who underwent bipolar hemiarthroplasty (BPHA) for treatment of a pertrochanteric fracture, we compared and analyzed the amount of blood loss and complications between a group using the cemented stem and a group using the cementless stem.
MATERIALS AND METHODS
A total of 104 patients who underwent BPHA for treatment of a pertrochanteric fracture in our hospital for three years and 10 months (From January 2008 to October 2011) were included in this study. Among the 104 patients, 64 patients with a cemented stem were categorized into group 1, and the other 40 patients with an uncemented stem were categorized into group 2. Before surgery, the type of stem was determined by the bone quality of the proximal femur, which had been evaluated with a simple X-ray. Then, after surgery, the amount of blood loss and complications were compared between the two groups.
RESULTS
Expected blood loss during the operation was 389.8 cc in group 1, and 395.3 cc in group 2(P=0.88). Postoperatively, average drained blood loss was 219.6 cc in group 1, and 338.1 cc in group 2. Cemented stem was associated with significantly less blood loss (P=0.004). The average operation time in group 1 and in group 2 was 96 minutes and 72 minutes. There was no significant difference in operating time (P=0.85). In addition, there was no difference in INR (International Normalized Ratio) and BMI (Body Mass Index) (P=0.28 and 0.08) regarding total amount of postoperatively drained blood loss. There was no occurrence of hypotensive shock or fatal pulmonary embolism in either group. Three cases of periprosthetic fracture occurred in group 2.
CONCLUSION
Fewer occurrences of postoperative blood loss and fewer complications were observed in the cemented stem group than in the cementless stem group. Preoperative evaluation of bone quality and use of the cement stem for patients with poor bone quality may be a good treatment method that can help to reduce complications.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Comparative Study of Bipolar Hemiarthroplasty for Femur Neck Fractures Treated with Cemented versus Cementless Stem
Jung-Yun Choi, Yerl-Bo Sung, Joo-Hyung Kim
Hip Pelvis. 2016;28(4):208-216. doi: 10.5371/hp.2016.28.4.208.
Reference
-
1. Dhanwal DK, Dennison EM, Harvey NC, Cooper C. Epidemiology of hip fracture: Worldwide geographic variation. Indian J Orthop. 2011. 45:15–22.
Article2. Kim WY, Han CH, Park JI, Kim JY. Failure of intertrochanteric fracture fixation with a dynamic hip screw in relation to pre-operative fracture stability and osteoporosis. Int Orthop. 2001. 25:360–362.
Article3. Kim SY, Kim YG, Hwang JK. Cementless calcar-replacement hemiarthroplasty compared with intramedullary fixation of unstable intertrochanteric fractures. A prospective, randomized study. J Bone Joint Surg Am. 2005. 87:2186–2192.
Article4. Marya S, Thukral R, Hasan R, Tripathi M. Cementless bipolar hemiarthroplasty in femoral neck fractures in elderly. Indian J Orthop. 2011. 45:236–242.
Article5. Parvizi J, Holiday AD, Ereth MH, Lewallen DG. The Frank Stinchfield Award. Sudden death during primary hip arthroplasty. Clin Orthop Relat Res. 1999. (369):39–48.6. Foster AP, Thompson NW, Wong J, Charlwood AP. Periprosthetic femoral fractures--a comparison between cemented and uncemented hemiarthroplasties. Injury. 2005. 36:424–429.
Article7. Harwin SF, Stern RE, Kulick RG. Primary Bateman-Leinbach bipolar prosthetic replacement of the hip in the treatment of unstable intertrochanteric fractures in the elderly. Orthopedics. 1990. 13:1131–1136.
Article8. Green S, Moore T, Proano F. Bipolar prosthetic replacement for the management of unstable intertrochanteric hip fractures in the elderly. Clin Orthop Relat Res. 1987. (224):169–177.
Article9. Sinno K, Sakr M, Girard J, Khatib H. The effectiveness of primary bipolar arthroplasty in treatment of unstable intertrochanteric fractures in elderly patients. N Am J Med Sci. 2010. 2:561–568.
Article10. Dorr LD, Faugere MC, Mackel AM, Gruen TA, Bognar B, Malluche HH. Structural and cellular assessment of bone quality of proximal femur. Bone. 1993. 14:231–242.
Article11. Kim YS, Kwon SY, Sun DH, Han SK, Maloney WJ. Modified posterior approach to total hip arthroplasty to enhance joint stability. Clin Orthop Relat Res. 2008. 466:294–299.
Article12. Thomsen MN, Jakubowitz E, Seeger JB, Lee C, Kretzer JP, Clarius M. Fracture load for periprosthetic femoral fractures in cemented versus uncemented hip stems: an experimental in vitro study. Orthopedics. 2008. 31:653.
Article13. Parker MJ, Gurusamy KS, Azegami S. Arthroplasties (with and without bone cement) for proximal femoral fractures in adults. Cochrane Database Syst Rev. 2010. (6):CD001706.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment of trochanteric fractures of the femur in osteoporotic patients
- Treatment of Unstable Intertrochanteric Fracture in Elderly Patients : Comparison between the Results of Internal Fixation Using Compression Hip Screw and Cemented Bipolar Hemiarthroplasty
- Comparison between Cementless and Cemented Bipolar Hemiarthroplasty for Treatment of Unstable Intertrochanteric Fractures: Systematic Review and Meta-analysis
- Cemented Hemiarthroplasty in Femoral Neck Fractures over 70 Years : A Matched-Pair Analysis of unipolar and Bipolar Hemiarthroplasty
- Comparative Study of Bipolar Hemiarthroplasty for Femur Neck Fractures Treated with Cemented versus Cementless Stem