J Korean Med Sci.
2012 Jun;27(6):697-700. 10.3346/jkms.2012.27.6.697.
Disseminated Penicilliosis in a Korean Human Immunodeficiency Virus Infected Patient from Laos
- Affiliations
-
- 1Division of Infectious Disease, Department of Internal Medicine, National Medical Center, Seoul, Korea. moberrer@hanmail.net
- 2Department of Dermatology, National Medical Center, Seoul, Korea.
- 3Department of Laboratory Medicine, Chonnam National University Medical School, Gwangju, Korea.
- KMID: 1421625
- DOI: http://doi.org/10.3346/jkms.2012.27.6.697
Abstract
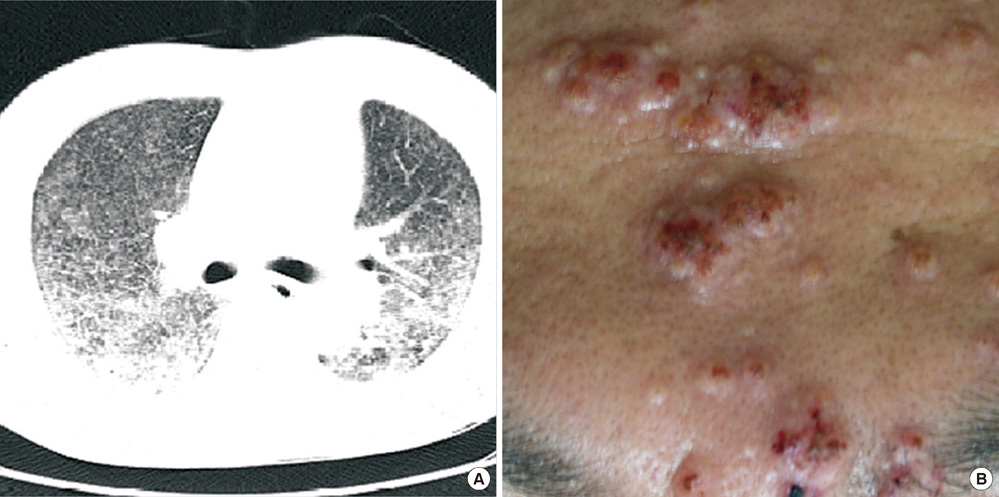
- Penicillium marneffei may cause life-threatening systemic fungal infection in immune-compromised patients and it is endemic in Southeast Asia. A 39-yr-old HIV-infected male, living in Laos, presented with fever, cough, and facial vesiculopapular lesions, which had been apparent for two weeks. CT scans showed bilateral micronodules on both lungs; Pneumocystis jirovecii was identified by bronchoscopic biopsy. Despite trimethoprim-sulfamethoxazole and anti-tuberculosis medications, the lung lesions progressed and the facial lesions revealed central umbilications. Biopsy of the skin lesions confirmed disseminated penicilliosis, with the culture showing P. marneffei hyphae and spores. The P. marneffei was identified by rRNA PCR. A review of the bronchoscopic biopsy indicated penicilliosis. The patient completely recovered after being prescribed amphotericin-B and receiving antiretroviral therapy. This is the first case of penicilliosis in a Korean HIV-infected patient. It is necessary to consider P. marneffei when immunocompromised patients, with a history of visits to endemic areas, reveal respiratory disease.
MeSH Terms
-
Adult
Amphotericin B/therapeutic use
Anti-HIV Agents/therapeutic use
Antifungal Agents/therapeutic use
Bronchoscopy
Dermatomycoses/drug therapy/microbiology/pathology
HIV Infections/*diagnosis/drug therapy
Humans
Immunocompromised Host
Laos
Lung Diseases/drug therapy/*microbiology
Male
Penicillium/genetics/*isolation & purification
Pneumocystis jirovecii/isolation & purification
Tomography, X-Ray Computed
Anti-HIV Agents
Antifungal Agents
Amphotericin B
Figure
Reference
-
1. Capponi M, Sureau P, Segretain G. Penicilliosis de Rhizomys sinensis. Bull Sco Pathol Exot Filiales. 1956. 49:418–421.2. DiSalvo AF, Ficking AM, Ajello L. Infection caused by Penicillium marneffei: description of first natural infection in man. Am J Clin Pathol. 1973. 60:259–263.3. Piehl MR, Kaplan RL, Haber MH. Disseminated penicilliosis in a patient with acquired immunodeficiency syndrome. Arch Pathol Lab Med. 1988. 112:1262–1264.4. Supparatpinyo K, Khamwan C, Baosoung V, Nelson KE, Sirisanthana T. Disseminated Penicillium marneffei infection in southeast Asia. Lancet. 1994. 344:110–113.5. Yap FB, Thevarajah S, Asmah J. Penicillium marneffei infection in an African man. Dermatol Online J. 2010. 16:2.6. Kim MN, Shin JH, Sung H, Lee K, Kim EC, Ryoo N, Lee JS, Jung SI, Park KH, Kee SJ, et al. Candida haemulonii and closely related species at 5 university hospitals in Korea: identification, antifungal susceptibility, and clinical features. Clin Infect Dis. 2009. 48:e57–e61.7. Lu PX, Zhu WK, Liu Y, Chen XC, Zhan NY, Liu JQ, Zang J, Yang GD, Ye RX, Cai LS. Acquired immunodeficiency syndrome associated disseminated Penicillium marneffei infection: report of 8 cases. Chin Med J. 2005. 118:1395–1399.8. Zhao DW, Zhang T, Ma DQ, Wang W, Yuan CW, Duan Y. Disseminated Penicillium marneffei infection in acquired immunodeficiency syndrome: a case report. Chin Med J. 2005. 118:1054–1056.9. Wu TC, Chan JW, Ng CK, Tsang DN, Lee MP, Li PC. Clinical presentations and outcomes of Penicillium marneffei infections: a series from 1994 to 2004. Hong Kong Med J. 2008. 14:103–109.10. Thomas CF Jr, Limper AH. Pneumocystis pneumonia. N Engl J Med. 2004. 350:2487–2498.11. King LJ, Padley SP. Imaging of the thorax AIDS. Imaging. 2002. 14:60–76.12. Kuhlman JE, Kavuru M, Fisherman EK, Siegelman SS. Pneumocystis carinii pneumonia: spectrum of parenchymal CT findings. Radiology. 1990. 175:711–714.13. Chiewchanvit S, Mahanupab P, Hirunsri P, Vanittanakom N. Cutaneous manifestations of disseminated Penicillium marneffei mycosis in five HIV-infected patients. Mycoses. 1991. 34:245–249.14. Ho KK. Penicillium marneffei infection in a chinese man with HIV infection. Hong Kong Dermatol Venereol Bull. 2000. 28–30.15. Wong SS, Wong KH, Hui WT, Lee SS, Lo JY, Cao L, Yuen KY. Differences in clinical and laboratory diagnostic characteristics of Penicilliosis marneffei in human immunodeficiency virus (HIV)- and non-HIV-infected patients. J Clin Microbiol. 2001. 39:4535–4540.16. Vanittanakom N, Cooper CR Jr, Fisher MC, Sirisanthana T. Penicillium marneffei infection and recent advances in the epidermiology and molecular biology aspects. Clin Microbiol Rev. 2006. 19:95–110.17. Han SH, Choi HY, Lee SC, Goo YS, Chang KH, Kang SW, Choi KH, Kim JM, Lee HY, Han DS, et al. A case of Penicilium marneffei CAPD peritonitis. Korean J Nephrol. 2002. 21:680–685.18. Seo JY, Ma YE, Lee JH, Lee ST, Ki CS, Lee NY. A case of disseminated Penicillium marneffei infection in a liver transplant recipient. Korean J Lab Med. 2010. 30:400–405.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Ankylosing Spondylitis in a Patient with Human Immunodeficiency Virus
- Esophago-Pleural Fistula with Multiple Esophageal Ulcers in Human Immunodeficiency Virus Infected Patient: A Case Report
- A Case of Acute Erythroleukemia in a Human Immunodeficiency Virus-Infected Patient
- A Case of Disseminated Varicella-zoster Virus Infection with Pneumonia in a Patient with AIDS
- Malignancies in HIV-infected patients