Korean J Radiol.
2012 Dec;13(6):784-794. 10.3348/kjr.2012.13.6.784.
Radiofrequency Ablation for Viable Hepatocellular Carcinoma around Retained Iodized Oil after Transcatheter Arterial Chemoembolization: Usefulness of Biplane Fluoroscopy Plus Ultrasound Guidance
- Affiliations
-
- 1Department of Radiology and Center for Imaging Science, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul 135-710, Korea. leeminwoo0@gmail.com
- 2Department of Radiology and Research Institute of Biomedical Science, Konkuk University School of Medicine, Seoul 143-701, Korea.
- KMID: 1397510
- DOI: http://doi.org/10.3348/kjr.2012.13.6.784
Abstract
OBJECTIVE
To assess the technical feasibility and local efficacy of biplane fluoroscopy plus US-guided percutaneous radiofrequency ablation (RFA) for viable hepatocellular carcinoma (HCC) around retained iodized oil after transcatheter arterial chemoembolization (TACE).
MATERIALS AND METHODS
Our prospective study was approved by our institutional review board and informed consent was obtained from all participating patients. For patients with viable HCC around retained iodized oil after TACE, biplane fluoroscopy plus US-guided RFA was performed. We evaluated the rate of technical success and major complications on a post-RFA CT examination and local tumor progression with a follow-up CT.
RESULTS
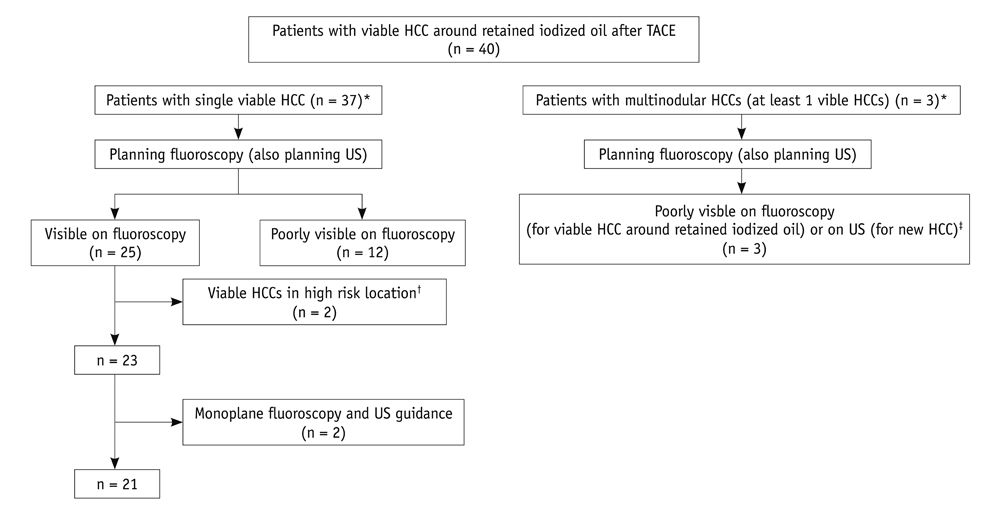
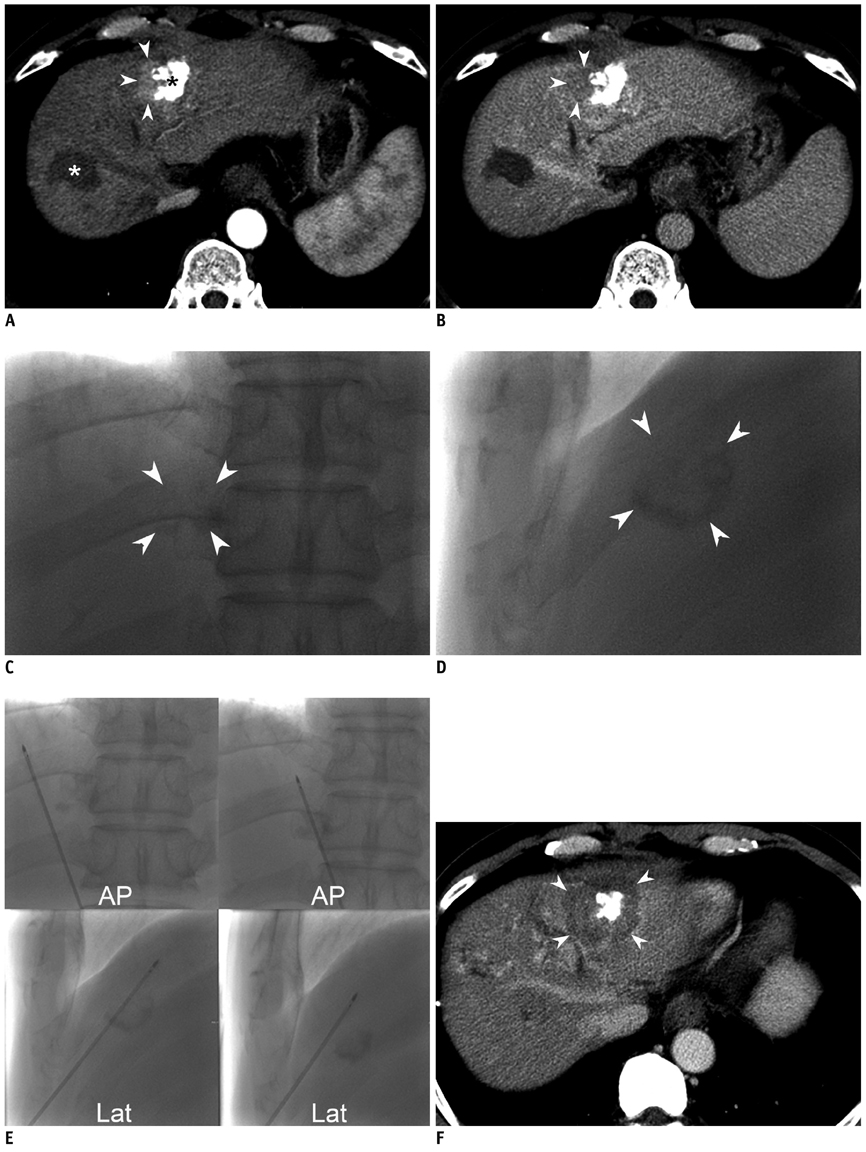
Among 40 consecutive patients, 19 were excluded due to one of the following reasons: poorly visible HCC on fluoroscopy (n = 13), high risk location (n = 2), RFA performed under monoplane fluoroscopy and US guidance (n = 2), and poorly identifiable new HCCs on US (n = 2). The remaining 21 patients with 21 viable HCCs were included. The size of total tumors ranged from 1.4 to 5.0 cm (mean: 3.2 cm) in the longest diameter. Technical success was achieved for all 21 HCCs, and major complications were observed in none of the patients. During the follow-up period (mean, 20.3 months; range, 6.5-29.9 months), local tumor progression was found in two patients (2/21, 9.5%). Distant intrahepatic metastasis developed in 76.2% (16/21) of patients.
CONCLUSION
When retained iodized oil around the tumor after TACE hampers the targeting of the viable tumor for RFA, biplane fluoroscopy plus US-guided RFA may be performed owing to its technical feasibility and effective treatment for viable HCCs.
Keyword
MeSH Terms
-
Aged
Aged, 80 and over
Carcinoma, Hepatocellular/radiography/*surgery/therapy
*Catheter Ablation
*Chemoembolization, Therapeutic
Complex Mixtures
*Contrast Media
Female
*Fluoroscopy/methods
Humans
Iodized Oil/*administration & dosage
Iohexol/analogs & derivatives/diagnostic use
Liver Neoplasms/radiography/*surgery/therapy
Male
Middle Aged
*Ultrasonography, Interventional
Figure
Reference
-
1. Lo CM, Ngan H, Tso WK, Liu CL, Lam CM, Poon RT, et al. Randomized controlled trial of transarterial lipiodol chemoembolization for unresectable hepatocellular carcinoma. Hepatology. 2002. 35:1164–1171.2. Saccheri S, Lovaria A, Sangiovanni A, Nicolini A, De Fazio C, Ronchi G, et al. Segmental transcatheter arterial chemoembolization treatment in patients with cirrhosis and inoperable hepatocellular carcinomas. J Vasc Interv Radiol. 2002. 13:995–999.3. Llovet JM, Bruix J. Systematic review of randomized trials for unresectable hepatocellular carcinoma: chemoembolization improves survival. Hepatology. 2003. 37:429–442.4. Bruix J, Sala M, Llovet JM. Chemoembolization for hepatocellular carcinoma. Gastroenterology. 2004. 127:5 Suppl 1. S179–S188.5. Decaens T, Roudot-Thoraval F, Bresson-Hadni S, Meyer C, Gugenheim J, Durand F, et al. Impact of pretransplantation transarterial chemoembolization on survival and recurrence after liver transplantation for hepatocellular carcinoma. Liver Transpl. 2005. 11:767–775.6. Uchida H, Matsuo N, Sakaguchi H, Nagano N, Nishimine K, Ohishi H. Segmental embolotherapy for hepatic cancer: keys to success. Cardiovasc Intervent Radiol. 1993. 16:67–71.7. Lee J, Lee JM, Yoon JH, Lee JY, Kim SH, Lee JE, et al. Percutaneous radiofrequency ablation with multiple electrodes for medium-sized hepatocellular carcinomas. Korean J Radiol. 2012. 13:34–43.8. Yamakado K, Nakatsuka A, Takaki H, Yokoi H, Usui M, Sakurai H, et al. Early-stage hepatocellular carcinoma: radiofrequency ablation combined with chemoembolization versus hepatectomy. Radiology. 2008. 247:260–266.9. Lee MW, Kim YJ, Park SW, Jeon HJ, Yi JG, Choe WH, et al. Percutaneous radiofrequency ablation of liver dome hepatocellular carcinoma invisible on ultrasonography: a new targeting strategy. Br J Radiol. 2008. 81:e130–e134.10. Lee MW, Kim YJ, Park SW, Yu NC, Choe WH, Kwon SY, et al. Biplane fluoroscopy-guided radiofrequency ablation combined with chemoembolisation for hepatocellular carcinoma: initial experience. Br J Radiol. 2011. 84:691–697.11. Bruix J, Sherman M. Practice Guidelines Committee, American Association for the Study of Liver Diseases. Management of hepatocellular carcinoma. Hepatology. 2005. 42:1208–1236.12. Llovet JM, Di Bisceglie AM, Bruix J, Kramer BS, Lencioni R, Zhu AX, et al. Design and endpoints of clinical trials in hepatocellular carcinoma. J Natl Cancer Inst. 2008. 100:698–711.13. Lencioni R, Llovet JM. Modified RECIST (mRECIST) assessment for hepatocellular carcinoma. Semin Liver Dis. 2010. 30:52–60.14. Rhim H, Choi D, Kim YS, Lim HK, Choe BK. Ultrasonography-guided percutaneous radiofrequency ablation of hepatocellular carcinomas: a feasibility scoring system for planning sonography. Eur J Radiol. 2010. 75:253–258.15. Song I, Rhim H, Lim HK, Kim YS, Choi D. Percutaneous radiofrequency ablation of hepatocellular carcinoma abutting the diaphragm and gastrointestinal tracts with the use of artificial ascites: safety and technical efficacy in 143 patients. Eur Radiol. 2009. 19:2630–2640.16. Kim SW, Rhim H, Park M, Kim H, Kim YS, Choi D, et al. Percutaneous radiofrequency ablation of hepatocellular carcinomas adjacent to the gallbladder with internally cooled electrodes: assessment of safety and therapeutic efficacy. Korean J Radiol. 2009. 10:366–376.17. Chung YH. A strategy for early detection of recurrent hepatocellular carcinoma following initial remission by transcatheter arterial chemoembolization. Intervirology. 2005. 48:46–51.18. Goldberg SN, Gazelle GS, Dawson SL, Rittman WJ, Mueller PR, Rosenthal DI. Tissue ablation with radiofrequency: effect of probe size, gauge, duration, and temperature on lesion volume. Acad Radiol. 1995. 2:399–404.19. Morimoto M, Numata K, Kondou M, Nozaki A, Morita S, Tanaka K. Midterm outcomes in patients with intermediate-sized hepatocellular carcinoma: a randomized controlled trial for determining the efficacy of radiofrequency ablation combined with transcatheter arterial chemoembolization. Cancer. 2010. 116:5452–5460.20. Shibata T, Isoda H, Hirokawa Y, Arizono S, Shimada K, Togashi K. Small hepatocellular carcinoma: is radiofrequency ablation combined with transcatheter arterial chemoembolization more effective than radiofrequency ablation alone for treatment? Radiology. 2009. 252:905–913.21. Goldberg SN, Grassi CJ, Cardella JF, Charboneau JW, Dodd GD 3rd, Dupuy DE, et al. Image-guided tumor ablation: standardization of terminology and reporting criteria. J Vasc Interv Radiol. 2009. 20:7 Suppl. S377–S390.22. Goldberg SN, Grassi CJ, Cardella JF, Charboneau JW, Dodd GD 3rd, Dupuy DE, et al. Image-guided tumor ablation: standardization of terminology and reporting criteria. Radiology. 2005. 235:728–739.23. Yamakado K, Nakatsuka A, Ohmori S, Shiraki K, Nakano T, Ikoma J, et al. Radiofrequency ablation combined with chemoembolization in hepatocellular carcinoma: treatment response based on tumor size and morphology. J Vasc Interv Radiol. 2002. 13:1225–1232.24. Miura H, Yamagami T, Terayama K, Yoshimatsu R, Matsumoto T, Nishimura T. Pneumothorax induced by radiofrequency ablation for hepatocellular carcinoma beneath the diaphragm under real-time computed tomography-fluoroscopic guidance. Acta Radiol. 2010. 51:613–618.25. Shibata T, Shibata T, Maetani Y, Kubo T, Itoh K, Togashi K, et al. Transthoracic percutaneous radiofrequency ablation for liver tumors in the hepatic dome. J Vasc Interv Radiol. 2004. 15:1323–1327.26. Toyoda M, Kakizaki S, Horiuchi K, Katakai K, Sohara N, Sato K, et al. Computed tomography-guided transpulmonary radiofrequency ablation for hepatocellular carcinoma located in hepatic dome. World J Gastroenterol. 2006. 12:608–611.27. Kato T, Yamagami T, Hirota T, Matsumoto T, Yoshimatsu R, Nishimura T. Transpulmonary radiofrequency ablation for hepatocellular carcinoma under real-time computed tomography-fluoroscopic guidance. Hepatogastroenterology. 2008. 55:1450–1453.28. Paulson EK, Sheafor DH, Enterline DS, McAdams HP, Yoshizumi TT. CT fluoroscopy--guided interventional procedures: techniques and radiation dose to radiologists. Radiology. 2001. 220:161–167.29. Min JH, Lee MW, Rhim H, Choi D, Kim YS, Kim YJ, et al. Recurrent hepatocellular carcinoma after transcatheter arterial chemoembolization: planning sonography for radio frequency ablation. J Ultrasound Med. 2011. 30:617–624.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Radiofrequency Ablation Combined with Chemoembolization for Intermediate-Sized (3-5 cm) Hepatocellular Carcinomas Under Dual Guidance of Biplane Fluoroscopy and Ultrasonography
- Ultraselective conventional transarterial chemoembolization: When and how?
- Comparison of Combined Therapy Using Conventional Chemoembolization and Radiofrequency Ablation Versus Conventional Chemoembolization for Ultrasound-Invisible Early-Stage Hepatocellular Carcinoma (Barcelona Clinic Liver Cancer Stage 0 or A)
- Computed Tomographic-Guided Radiofrequency Ablation of Recurrent or Residual Hepatocellular Carcinomas around Retained Iodized Oil after Transarterial Chemoembolization
- Chemoembolization combined with radiofrequency ablation is the best option for the local treatment of early hepatocellular carcinoma?