Korean J Ophthalmol.
2012 Oct;26(5):331-338. 10.3341/kjo.2012.26.5.331.
Satisfaction Level of Physicians Who Have Undergone Corneal Refractive Surgery
- Affiliations
-
- 1Department of Ophthalmology, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea. eye129@paran.com
- 2Department of Ophthalmology, Myong ji Hospital, Kwandong University College of Medicine, Goyang, Korea.
- 3Department of Ophthalmology, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea.
- 4Department of Ophthalmology, Seoul National University Boramae Hospital, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 1397483
- DOI: http://doi.org/10.3341/kjo.2012.26.5.331
Abstract
- PURPOSE
To evaluate the levels of satisfaction among physicians who have undergone corneal refractive surgery.
METHODS
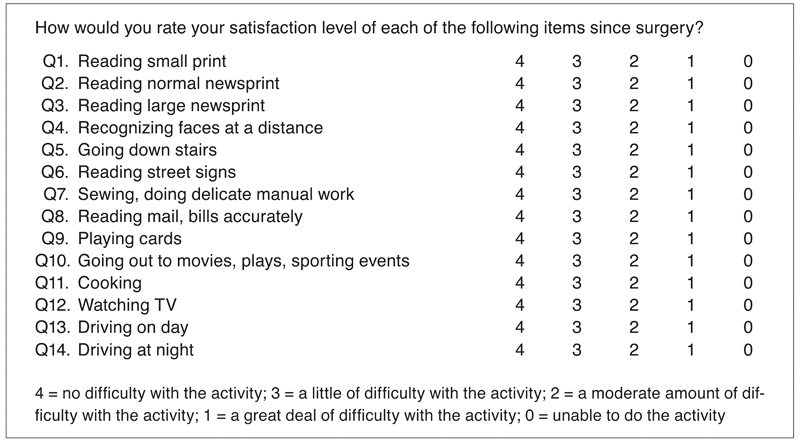
This study included 212 eyes of 107 consecutive patients who underwent laser in situ keratomileusis or laser sub-epithelial keratomileusis surgery. Patients were divided into two groups: one group of physicians and one group of other healthcare workers (HCWs). The physicians' group was also subdivided into two different groups: surgeons or doctors using microscopes and medical physicians. The main outcome measures were scale scores obtained by using the Visual Function Index-14 questionnaires; uncorrected distance visual acuity (UDVA), residual spherical equivalent (SE), optical zone diameter, and residual corneal thickness were also compared between the groups.
RESULTS
No significant differences in preoperative parameters, with the exception of the ratio of types of refractive surgery, were noted between the physicians and the HCWs group. Additionally, no differences between the groups were noted in the postoperative UDVA, residual SE, optical zone diameter, residual corneal thickness, and level of satisfaction. When comparing the two subgroups of physicians, the differences in satisfaction rates were not statistically significant, even in terms of the performance of delicate manual work.
CONCLUSIONS
No statistically significant differences in the clinical outcomes and satisfaction scores were detected after surgery between the physicians and HCWs groups, nor were any significant differences detected between the surgeons and medical physicians groups. Corneal refractive surgery can conceivably be recommended even for physicians who perform intensive near vision-dependent activities and delicate operations.
MeSH Terms
Figure
Reference
-
1. Tahzib NG, Bootsma SJ, Eggink FA, et al. Functional outcomes and patient satisfaction after laser in situ keratomileusis for correction of myopia. J Cataract Refract Surg. 2005. 31:1943–1951.2. Tuan KM. Visual experience and patient satisfaction with wavefront-guided laser in situ keratomileusis. J Cataract Refract Surg. 2006. 32:577–583.3. Lin DJ, Sheu IC, Pai JY, et al. Measuring patient's expectation and the perception of quality in LASIK services. Health Qual Life Outcomes. 2009. 7:63.4. Bailey MD, Mitchell GL, Dhaliwal DK, et al. Patient satisfaction and visual symptoms after laser in situ keratomileusis. Ophthalmology. 2003. 110:1371–1378.5. Solomon KD, Fernandez de Castro LE, Sandoval HP, et al. LASIK world literature review: quality of life and patient satisfaction. Ophthalmology. 2009. 116:691–701.6. Schmidt GW, Yoon M, McGwin G, et al. Evaluation of the relationship between ablation diameter, pupil size, and visual function with vision-specific quality-of-life measures after laser in situ keratomileusis. Arch Ophthalmol. 2007. 125:1037–1042.7. Hammond SD Jr, Puri AK, Ambati BK. Quality of vision and patient satisfaction after LASIK. Curr Opin Ophthalmol. 2004. 15:328–332.8. Chan A, Manche EE. Effect of preoperative pupil size on quality of vision after wavefront-guided LASIK. Ophthalmology. 2011. 118:736–741.9. Steinberg EP, Tielsch JM, Schein OD, et al. The VF-14: an index of functional impairment in patients with cataract. Arch Ophthalmol. 1994. 112:630–638.10. Levinson BA, Rapuano CJ, Cohen EJ, et al. Referrals to the Wills Eye Institute Cornea Service after laser in situ keratomileusis: reasons for patient dissatisfaction. J Cataract Refract Surg. 2008. 34:32–39.11. Yu J, Chen H, Wang F. Patient satisfaction and visual symptoms after wavefront-guided and wavefront-optimized LASIK with the WaveLight platform. J Refract Surg. 2008. 24:477–486.12. Brunette I, Gresset J, Boivin JF, et al. Functional outcome and satisfaction after photorefractive keratectomy. Part 1: development and validation of a survey questionnaire. Ophthalmology. 2000. 107:1783–1789.13. Morse JS, Schallhorn SC, Hettinger K, Tanzer D. Role of depressive symptoms in patient satisfaction with visual quality after laser in situ keratomileusis. J Cataract Refract Surg. 2009. 35:341–346.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effect of Strabismus Surgery on Refractive Error Measured with Corneal Topography
- Corneal Topographic Changes after Surgery in Epiblepharon Children
- Agreement of Actual Corneal Power and Corneal Power Using Topography in Cataract Patients Undergone Refractive Surgery
- Comparison of Measured Intraocular Pressure Change According to the Methods of Corneal Refractive Surgery
- Comparison of Four Systems of IOL Calculation after Keratorefractive Surgery in Eyes Requiring Cataract Surgery