Clin Orthop Surg.
2012 Sep;4(3):200-208. 10.4055/cios.2012.4.3.200.
Transpedicular Curettage and Drainage of Infective Lumbar Spondylodiscitis: Technique and Clinical Results
- Affiliations
-
- 1Department of Orthopedic Surgery, Yonsei University College of Medicine, Seoul, Korea. shmoon@yuhs.ac
- KMID: 1392982
- DOI: http://doi.org/10.4055/cios.2012.4.3.200
Abstract
- BACKGROUND
Infective spondylodiscitis usually occurs in patients of older age, immunocompromisation, co-morbidity, and individuals suffering from an overall poor general condition unable to undergo reconstructive anterior and posterior surgeries. Therefore, an alternative, less aggressive surgical method is needed for these select cases of infective spondylodiscitis. This retrospective clinical case series reports our novel surgical technique for the treatment of infective spondylodiscitis.
METHODS
Between January 2005 and July 2011, among 48 patients who were diagnosed with pyogenic lumbar spondylodiscitis or tuberculosis lumbar spondylodiscitis, 10 patients (7 males and 3 females; 68 years and 48 to 78 years, respectively) underwent transpedicular curettage and drainage. The mean postoperative follow-up period was 29 months (range, 7 to 61 months). The pedicle screws were inserted to the adjacent healthy vertebrae in the usual manner. After insertion of pedicle screws, the drainage pedicle holes were made through pedicles of infected vertebra(e) in order to prevent possible seeding of infective emboli to the healthy vertebra, as the same instruments and utensils are used for both pedicle screws and the drainage holes. A minimum of 15,000 mL of sterilized normal saline was used for continuous irrigation through the pedicular pathways until the drained fluid looked clear.
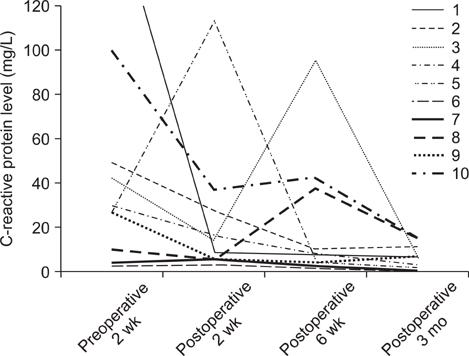
RESULTS
All patients' symptoms and inflammatory markers significantly improved clinically between postoperative 2 weeks and postoperative 3 months, and they were satisfied with their clinical results. Radiologically, all patients reached the spontaneous fusion between infected vertebrae and 3 patients had the screw pulled-out but they were clinically tolerable.
CONCLUSIONS
We suggest that our method of transpedicular curettage and drainage is a useful technique in regards to the treatment of infectious spondylodiscitic patients, who could not tolerate conventional combined anterior and posterior surgery due to multiple co-morbidities, multiple level infectious lesions and poor general condition.
Keyword
MeSH Terms
Figure
Reference
-
1. Calderone RR, Larsen JM. Overview and classification of spinal infections. Orthop Clin North Am. 1996. 27(1):1–8.
Article2. Muller EJ, Russe OJ, Muhr G. Osteomyelitis of the spine. Orthopade. 2004. 33(3):305–315.
Article3. McGuire RA, Eismont FJ. The fate of autogenous bone graft in surgically treated pyogenic vertebral osteomyelitis. J Spinal Disord. 1994. 7(3):206–215.
Article4. Ghanayem AJ, Zdeblick TA. Cervical spine infections. Orthop Clin North Am. 1996. 27(1):53–67.
Article5. Graziano GP, Sidhu KS. Salvage reconstruction in acute and late sequelae from pyogenic thoracolumbar infection. J Spinal Disord. 1993. 6(3):199–207.
Article6. Abramovitz JN, Batson RA, Yablon JS. Vertebral osteomyelitis: the surgical management of neurologic complications. Spine (Phila Pa 1976). 1986. 11(5):418–420.
Article7. Dimar JR, Carreon LY, Glassman SD, Campbell MJ, Hartman MJ, Johnson JR. Treatment of pyogenic vertebral osteomyelitis with anterior debridement and fusion followed by delayed posterior spinal fusion. Spine (Phila Pa 1976). 2004. 29(3):326–332.
Article8. Fukuta S, Miyamoto K, Masuda T, et al. Two-stage (posterior and anterior) surgical treatment using posterior spinal instrumentation for pyogenic and tuberculotic spondylitis. Spine (Phila Pa 1976). 2003. 28(15):E302–E308.
Article9. Carragee EJ. Instrumentation of the infected and unstable spine: a review of 17 cases from the thoracic and lumbar spine with pyogenic infections. J Spinal Disord. 1997. 10(4):317–324.
Article10. Chen WJ, Wu CC, Jung CH, Chen LH, Niu CC, Lai PL. Combined anterior and posterior surgeries in the treatment of spinal tuberculous spondylitis. Clin Orthop Relat Res. 2002. (398):50–59.
Article11. Dietze DD Jr, Fessler RG, Jacob RP. Primary reconstruction for spinal infections. J Neurosurg. 1997. 86(6):981–989.
Article12. Fayazi AH, Ludwig SC, Dabbah M, Bryan Butler R, Gelb DE. Preliminary results of staged anterior debridement and reconstruction using titanium mesh cages in the treatment of thoracolumbar vertebral osteomyelitis. Spine J. 2004. 4(4):388–395.
Article13. Lee MC, Wang MY, Fessler RG, Liauw J, Kim DH. Instrumentation in patients with spinal infection. Neurosurg Focus. 2004. 17(6):E7.
Article14. Rath SA, Neff U, Schneider O, Richter HP. Neurosurgical management of thoracic and lumbar vertebral osteomyelitis and discitis in adults: a review of 43 consecutive surgically treated patients. Neurosurgery. 1996. 38(5):926–933.
Article15. Perronne C, Saba J, Behloul Z, et al. Pyogenic and tuberculous spondylodiskitis (vertebral osteomyelitis) in 80 adult patients. Clin Infect Dis. 1994. 19(4):746–750.
Article16. Klockner C, Valencia R. Sagittal alignment after anterior debridement and fusion with or without additional posterior instrumentation in the treatment of pyogenic and tuberculous spondylodiscitis. Spine (Phila Pa 1976). 2003. 28(10):1036–1042.
Article17. Erkan S, Wu C, Mehbod AA, Cho W, Transfeldt EE. Biomechanical comparison of transpedicular versus extrapedicular vertebroplasty using polymethylmethacrylate. J Spinal Disord Tech. 2010. 23(3):180–185.
Article18. Chen L, Yang H, Tang T. Unilateral versus bilateral balloon kyphoplasty for multilevel osteoporotic vertebral compression fractures: a prospective study. Spine (Phila Pa 1976). 2011. 36(7):534–540.
Article19. Suk SI, Lee CK, Min HJ, Cho KH, Oh JH. Comparison of Cotrel-Dubousset pedicle screws and hooks in the treatment of idiopathic scoliosis. Int Orthop. 1994. 18(6):341–346.20. Suk SI. Pedicle screw instrumentation for adolescent idiopathic scoliosis: the insertion technique, the fusion levels and direct vertebral rotation. Clin Orthop Surg. 2011. 3(2):89–100.21. Okada Y, Miyamoto H, Uno K, Sumi M. Clinical and radiological outcome of surgery for pyogenic and tuberculous spondylitis: comparisons of surgical techniques and disease types. J Neurosurg Spine. 2009. 11(5):620–627.
Article22. Chen YC, Chang MC, Wang ST, Yu WK, Liu CL, Chen TH. One-stage posterior surgery for treatment of advanced spinal tuberculosis. J Chin Med Assoc. 2003. 66(7):411–417.
Article23. Beronius M, Bergman B, Andersson R. Vertebral osteomyelitis in Goteborg, Sweden: a retrospective study of patients during 1990-95. Scand J Infect Dis. 2001. 33(7):527–532.
Article24. Patzakis MJ, Rao S, Wilkins J, Moore TM, Harvey PJ. Analysis of 61 cases of vertebral osteomyelitis. Clin Orthop Relat Res. 1991. (264):178–183.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Spondylodiscitis with Epidural Abscess Caused by Klebsiella pneumoniae
- Transforaminal Endoscopic Surgery: Outside-In Technique
- Pyogenic L4-5 Spondylitis Managed with Percutaneous Drainage Followed by Posterior Lumbar Interbody Fusion: A Case Report
- A case of infective endocarditis presented as cervical spondylodiscitis
- Spondylodiscitis after Cervical Nucleoplasty without Any Abnormal Laboratory Findings