Korean J Ophthalmol.
2012 Aug;26(4):309-311. 10.3341/kjo.2012.26.4.309.
Recurrent Bilateral Retinal Vasculitis as a Manifestation of Post-streptococcal Uveitis Syndrome
- Affiliations
-
- 1Institute of Vision Research, Department of Ophthalmology, Yonsei University College of Medicine, Seoul, Korea.
- 2Department of Ophthalmology, CHA Bundang Medical Center, CHA University, Seongnam, Korea. songwkmd@daum.net
- KMID: 1387401
- DOI: http://doi.org/10.3341/kjo.2012.26.4.309
Abstract
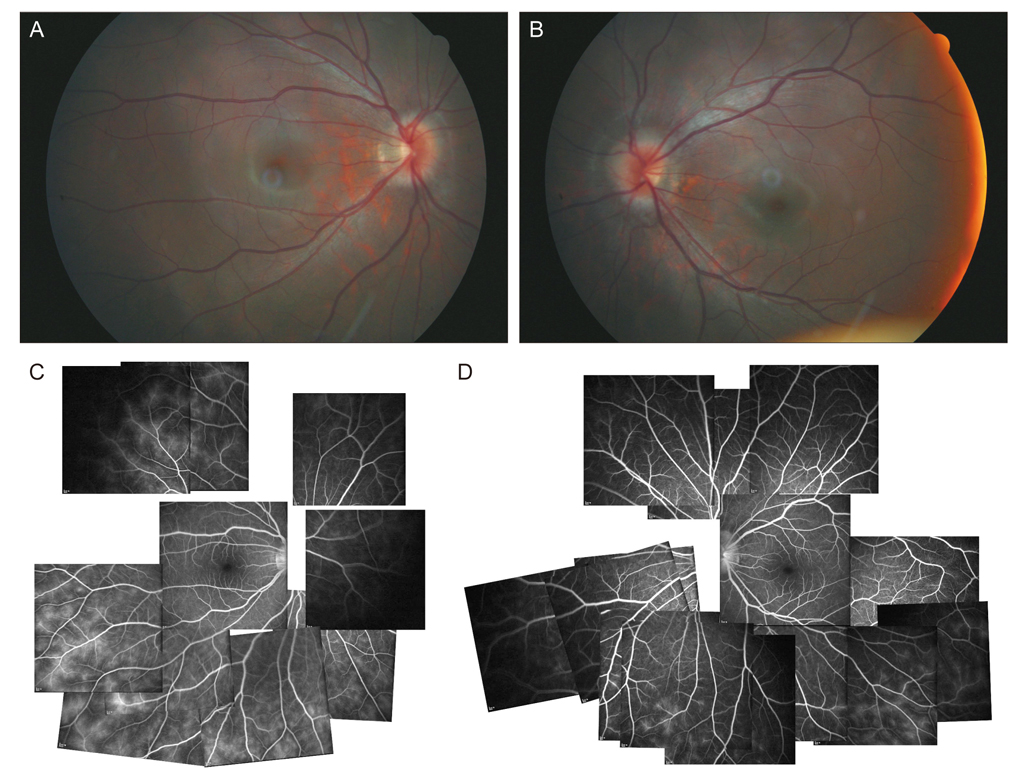
- We report a case of post-streptococcal uveitis mainly presenting with bilateral recurrent retinal vasculitis in Korea. A 14-year-old Asian female presented with decreased visual acuity of 20 / 30 in the right eye and 20 / 25 in the left eye. The patient had a history of glomerulonephritis nine months before onset of uveitis. The manifestation of uveitis was predominantly retinal vasculitis. We presumed post-streptococcal uveitis because probable streptococcal infection was confirmed by anti-streptolysin O titer elevation. With topical and oral steroid treatments, the patient experienced complete vision recovery. Post-streptococcal uveitis occurs rarely and mostly involves young patients in the form of non-granulomatous anterior uveitis. However, as this case shows, it may primarily involve the posterior uvea without anterior inflammation and may recur.
Keyword
MeSH Terms
Figure
Reference
-
1. Reddy UP, Albini TA, Banta JT, Davis JL. Post-streptococcal vasculitis. Ocul Immunol Inflamm. 2008. 16:35–36.2. Cokingtin CD, Han DP. Bilateral nongranulomatous uveitis and a poststreptococcal syndrome. Am J Ophthalmol. 1991. 112:595–596.3. Wirostko WJ, Connor TB Jr, Wagner PF. Recurrent post-streptococcal uveitis. Arch Ophthalmol. 1999. 117:1649–1650.4. Ur Rehman S, Anand S, Reddy A, et al. Poststreptococcal syndrome uveitis: a descriptive case series and literature review. Ophthalmology. 2006. 113:701–706.5. Gallagher MJ, Muqit MM, Jones D, Gavin M. Post-streptococcal uveitis. Acta Ophthalmol Scand. 2006. 84:424–428.6. De Smet MD. Papillophlebitis and uveitis as a manifestation of post-streptococcal uveitis syndrome. Eye (Lond). 2009. 23:985–987.7. Fox A, Hammer ME, Lill P, et al. Experimental uveitis. Elicited by peptidoglycan-polysaccharide complexes, lipopolysaccharide, and muramyl dipeptide. Arch Ophthalmol. 1984. 102:1063–1067.8. Wells A, Pararajasegaram G, Baldwin M, et al. Uveitis and arthritis induced by systemic injection of streptococcal cell walls. Invest Ophthalmol Vis Sci. 1986. 27:921–925.9. Feldon M, Dorfman L, Tauber T, et al. Post-streptococcal glomerulonephritis and uveitis: a case report. Pediatr Nephrol. 2010. 25:2351–2353.