Ann Lab Med.
2012 Jul;32(4):298-303. 10.3343/alm.2012.32.4.298.
Lung Infection Caused by Mycobacterium riyadhense Confused with Mycobacterium tuberculosis: The First Case in Korea
- Affiliations
-
- 1Department of Laboratory Medicine, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea. 690519@hitel.net
- 2Department of Internal Medicine, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea.
- KMID: 1380091
- DOI: http://doi.org/10.3343/alm.2012.32.4.298
Abstract
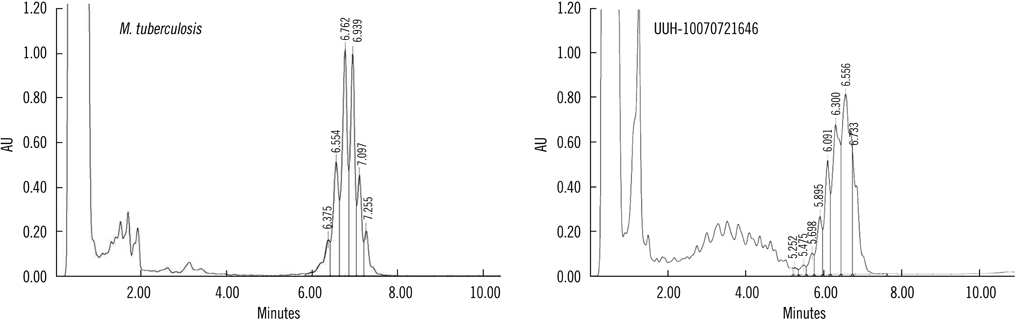
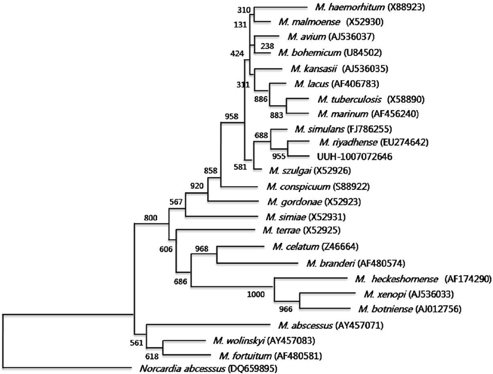
- A slowly growing, non-chromogenic mycobacterial strain was isolated from sputum and bronchial lavage fluid samples of a patient presenting with productive cough, blood-tinged sputum, low-grade fever, and weakness. A positive acid-fast bacilli sputum smear result prompted the initiation of an anti-tuberculosis regimen. Multiplex real-time PCR showed a negative result for Mycobacterium tuberculosis complex and a positive result for nontuberculous mycobacteria. The DNA chip test confirmed this organism as a member of the genus Mycobacterium, but could not specify the species. Interestingly, the mycolic acid patterns obtained by HPLC nearly overlapped with those of M. simulans. The sequences of the Mycobacterium 16S rRNA gene and 16S-23S internal transcribed spacer region were unique and were found to have 100% similarity with those of M. riyadhense. After a review of the literature, we report this case as the first Korean case of M. riyadhense lung infection.
Keyword
MeSH Terms
-
Adult
Antitubercular Agents/pharmacology
Chromatography, High Pressure Liquid
Female
Humans
Lung Diseases/*microbiology
Microbial Sensitivity Tests
Mycobacterium/classification/drug effects/*isolation & purification
Mycobacterium Infections/microbiology
Mycobacterium tuberculosis/genetics/isolation & purification
Mycolic Acids/analysis
Oligonucleotide Array Sequence Analysis
Phylogeny
RNA, Ribosomal, 16S/chemistry/genetics
RNA, Ribosomal, 23S/chemistry/genetics
Republic of Korea
Sequence Analysis, DNA
Figure
Reference
-
1. Tortoli E. The new mycobacteria: an update. FEMS Immunol Med Microbiol. 2006. 48:159–178.
Article2. McNabb A, Eisler D, Adie K, Amos M, Rodrigues M, Stephens G, et al. Assessment of partial sequencing of the 65-kilodalton heat shock protein gene (hsp65) for routine identification of Mycobacterium species isolated from clinical sources. J Clin Microbiol. 2004. 42:3000–3011.3. Griffith DE, Aksamit T, Brown-Elliott BA, Catanzaro A, Daley C, Gordin F, et al. An official ATS/IDSA statement: diagnosis, treatment, and prevention of non-tuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007. 175:367–416.
Article4. Subcommittee of the Joint Tuberculosis Committee of the British Thoracic Society. Management of opportunist mycobacterial infections: Joint Tuberculosis Committee Guidelines 1999. Thorax. 2000. 55:210–218.5. Forbes BA, Sahm DF, editors. Bailey and Scott's Diagnostic Microbiology. 2007. 12th ed. St. Louis: Mosby Elsevier;481.6. Kim HJ. Current situation of tuberculosis and its control in Korea. J Korean Med Assoc. 2006. 49:762–772.
Article7. Prince DS, Peterson DD, Steiner RM, Gottlieb JE, Scott R, Israel HL, et al. Infection with Mycobacterium avium complex in patients without predisposing conditions. N Engl J Med. 1989. 321:863–868.8. Arend SM, van Soolingen D, Ottenhoff TH. Diagnosis and treatment of lung infection with nontuberculous mycobacteria. Curr Opin Pulm Med. 2009. 15:201–208.
Article9. van Ingen J, Al-Hajoj SA, Boeree M, Al-Rabiah F, Enaimi M, de Zwaan R, et al. Mycobacterium riyadhense sp. nov., a non-tuberculous species identified as Mycobacterium tuberculosis complex by a commercial line-probe assay. Int J Syst Evol Microbiol. 2009. 59:1049–1053.10. Tortoli E, Rogasi PG, Fantoni E, Beltrami C, De Francisci A, Mariottini A. Infection due to a novel mycobacterium, mimicking multidrug-resistant Mycobacterium tuberculosis. Clin Microbiol Infect. 2010. 16:1130–1134.11. Lévy-Frébault VV, Portaels F. Proposed minimal standards for the genus Mycobacterium and for description of new slowly growing Mycobacterium species. Int J Syst Bacteriol. 1992. 42:315–323.12. Torkko P, Suutari M, Suomalainen S, Paulin L, Larsson L, Katila ML. Separation among species of Mycobacterium terrae complex by lipid analyses: comparison with biochemical tests and 16S rRNA sequencing. J Clin Microbiol. 1998. 36:499–505.13. Jeong J, Kim SR, Lee SH, Choi JI, Chang CH, Choi JY, et al. The use of High Perfomance Liquid Chromatography to speciate and characterize the epidemiology of Mycobacteria. Lab Med. 2011. 42:612–617.14. Schuurman T, de Boer RF, Kooistra-Smid AM, van Zwet AA. Prospective study of use of PCR amplification and sequencing of 16S ribosomal DNA from cerebrospinal fluid for diagnosis of bacterial meningitis in a clinical setting. J Clin Microbiol. 2004. 42:734–740.
Article15. Telenti A, Marchesi F, Balz M, Bally F, Bottger EC, Bodmer T. Rapid identification of mycobacteria to the species level by polymerase chain reaction and restriction enzyme analysis. J Clin Microbiol. 1993. 31:175–178.
Article16. Larkin MA, Blackshields G, Brown NP, Chenna R, McGettigan PA, McWilliam H, et al. Clustal W and Clustal X version 2. Bioinformatics. 2007. 23:2947–2948.17. Clinical and Laboratory Standards Institute. Susceptibility testing of Mycobacteria, Nocardia, and other aerobic actinomycetes. Approved Standard M24-A2. 2011. 2nd ed. Wayne, PA: Clinical and Laboratory Standards Institute.18. Rodríguez-Aranda A, Jimenez MS, Yubero J, Chaves F, Rubio-Garcia R, Palenque E, et al. Misidentification of Mycobacterium kumamotonense as M. tuberculosis. Emerg Infect Dis. 2010. 16:1178–1180.19. Godreuil S, Marchandin H, Michon AL, Ponsada M, Chyderiotis G, Brisou P, et al. Mycobacterium riyadhense pulmonary infection, France and Bahrain. Emerg Infect Dis. 2012. 18:176–178.20. Tortoli E, Nanetti A, Piersimoni C, Cichero P, Farina C, Mucignat G, et al. Performance assessment of new multiplex probe assay for identification of mycobacteria. J Clin Microbiol. 2001. 39:1079–1084.
Article21. Springer B, Stockman L, Teschner K, Roberts GD, Böttger EC. Two-laboratory collaborative study on identification of mycobacteria: molecular versus phenotypic methods. J Clin Microbiol. 1996. 34:296–303.
Article22. Burman WJ. Review of false-positive cultures for Mycobacterium tuberculosis and recommendations for avoiding unnecessary treatment. Clin Infect Dis. 2000. 31:1390–1395.23. Nah J, Huh JW, Lee SH, Kim BC, Koh YS, Pai CH. Identification of Mycobacterium tuberculosis complex using a gene probe method. Korean J Clin Pathol. 1997. 17:71–78.24. Reisner BS, Gatson AM, Woods GL. Use of Gen-Probe AccuProbes to identify Mycobacterium avium complex, Mycobacterium tuberculosis complex, Mycobacterium kansasii, and Mycobacterium gordonae directly from BACTEC TB broth cultures. J Clin Microbiol. 1994. 32:2995–2998.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Differentiation between Mycobacterium bovis and Mycobacterium tuberculosis Infection
- Mixed Infection of Mycobacterium abscessus subsp. abscessus and Mycobacterium tuberculosis in the Lung
- Lymphomatoid Papulosis with Mycobacterium Other Than Tuberculosis
- Acute pneumonia caused by mycobacterium intracellulare
- A Case of Pulmonary and Endobronchial Mycobacterium avium Infection Presenting as an Acute Pneumonia in an Immunocompetent Patient