J Korean Med Sci.
2012 May;27(5):556-559. 10.3346/jkms.2012.27.5.556.
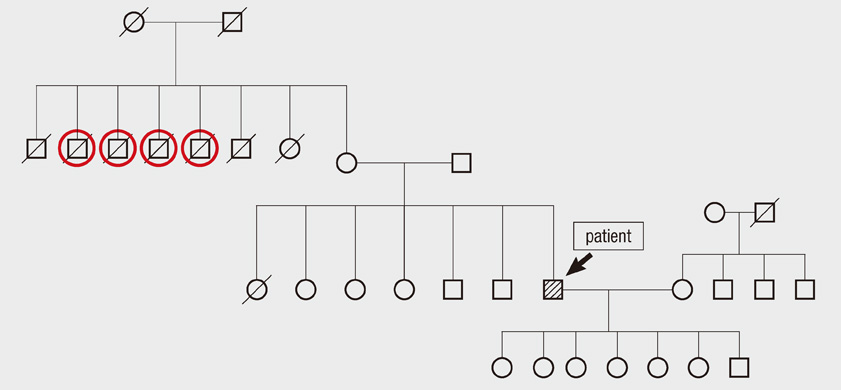
Hyperammonemia in a Patient with Late-Onset Ornithine Carbamoyltransferase Deficiency
- Affiliations
-
- 1Department of Internal Medicine, Chungnam National University Hospital, Daejeon, Korea. drngr@cnu.ac.kr
- KMID: 1372801
- DOI: http://doi.org/10.3346/jkms.2012.27.5.556
Abstract
- Ornithine carbamoyltransferase (OTC) deficiency is a urea cycle disorder that causes the accumulation of ammonia, which can lead to encephalopathy. Adults presenting with hyperammonemia who are subsequently diagnosed with urea cycle disorders are rare. Herein, we report a case of a late-onset OTC deficient patient who was successfully treated with arginine, benzoate and hemodialysis. A 59-yr-old man was admitted to our hospital with progressive lethargy and confusion. Although hyperammonemia was suspected as the cause of the patient's mental changes, there was no evidence of chronic liver disease. A plasma amino acid and urine organic acid analysis revealed OTC deficiency. Despite the administration of a lactulose enema, the patient's serum ammonia level increased and he remained confused, leading us to initiate acute hemodialysis. After treatment with arginine, sodium benzoate and hemodialysis, the patient's serum ammonia level stabilized and his mental status returned to normal.
Keyword
MeSH Terms
Figure
Reference
-
1. Brusilow SW, Maestri NE. Urea cycle disorders: diagnosis, pathophysiology, and therapy. Adv Pediatr. 1996. 43:127–170.2. Applegarth DA, Toone JR, Lowry RB. Incidence of inborn errors of metabolism in British Columbia, 1969-1996. Pediatrics. 2000. 105:e10.3. Tuchman M, Jaleel N, Morizono H, Sheehy L, Lynch MG. Mutations and polymorphisms in the human ornithine transcarbamylase gene. Hum Mutat. 2002. 19:93–107.4. Kang ES, Snodgrass PJ, Gerald PS. Ornithine transcarbamylase deficiency in the newborn infant. J Pediatr. 1973. 82:642–649.5. McCullough BA, Yudkoff M, Batshaw ML, Wilson JM, Raper SE, Tuchman M. Genotype spectrum of ornithine transcarbamylase deficiency: correlation with the clinical and biochemical phenotype. Am J Med Genet. 2000. 93:313–319.6. Tuchman M, McCullough BA, Yudkoff M. The molecular basis of ornithine transcarbamylase deficiency. Eur J Pediatr. 2000. 159:S196–S198.7. Tuchman M, Morizono H, Rajagopal BS, Plante RJ, Allewell NM. The biochemical and molecular spectrum of ornithine transcarbamylase deficiency. J Inherit Metab Dis. 1998. 21:40–58.8. Gordon N. Ornithine transcarbamylase deficiency: a urea cycle defect. Eur J Paediatr Neurol. 2003. 7:115–121.9. Ellaway CJ, Bennetts B, Tuck RR, Wilcken B. Clumsiness, confusion, coma, and valproate. Lancet. 1999. 353:1408.10. Hauser ER, Finkelstein JE, Valle D, Brusilow SW. Allopurinol-induced orotidinuria. A test for mutations at the ornithine carbamoyltransferase locus in women. N Engl J Med. 1990. 322:1641–1645.11. Bisanzi S, Morrone A, Donati MA, Pasquini E, Spada M, Strisciuglio P, Parenti G, Parini R, Papadia F, Zammarchi E. Genetic analysis in nine unrelated italian patients affected by OTC deficiency: detection of novel mutations in the OTC gene. Mol Genet Metab. 2002. 76:137–144.12. Brusilow SW. Arginine, an indispensable amino acid for patients with inborn errors of urea synthesis. J Clin Invest. 1984. 74:2144–2148.13. Mathias RS, Kostiner D, Packman S. Hyperammonemia in urea cycle disorders: role of the nephrologist. Am J Kidney Dis. 2001. 37:1069–1080.14. Wiegand C, Thompson T, Bock GH, Mathis RK, Kjellstrand CM, Mauer SM. The management of life-threatening hyperammonemia: a comparison of several therapeutic modalities. J Pediatr. 1980. 96:142–144.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- CT and MR Imaging in 3 Patients with Hyperammonemia Due to Ornithine Transcarbamylase Deficiency
- A Case of Ornithine Transcarbamylase (OTC) Deficiency
- Acute treatment of hyperammonemia by continuous renal replacement therapy in a newborn patient with ornithine transcarbamylase deficiency
- Lethal Hyperammonemia due to Ornithine Transcarbamylase Deficiency in a Patient with Severe Septic Shock
- A Case of Molecular Diagnosis of Ornithine Transcarbamylase Deficiency