Clin Orthop Surg.
2012 Mar;4(1):91-97. 10.4055/cios.2012.4.1.91.
Consensus and Different Perspectives on Treatment of Supracondylar Fractures of the Humerus in Children
- Affiliations
-
- 1Department of Orthopaedic Surgery, Sanggye Paik Hospital, Seoul, Korea.
- 2Department of Orthopedic Surgery, Seoul National University Bundang Hospital, Seongnam, Korea. oasis100@empal.com
- 3Department of Orthopedic Surgery, Seoul National University Children's Hospital, Seoul, Korea.
- KMID: 1245404
- DOI: http://doi.org/10.4055/cios.2012.4.1.91
Abstract
- BACKGROUND
Although closed reduction and percutaneous pinning is accepted as the treatment of choice for displaced supracondylar fracture of the humerus, there are some debates on the pinning techniques, period of immobilization, elbow range of motion (ROM) exercise, and perceptions on the restoration of elbow ROM. This study was to investigate the consensus and different perspectives on the treatment of supracondylar fractures of the humerus in children.
METHODS
A questionnaire was designed for this study, which included the choice of pinning technique, methods of elbow motion, and perception on the restoration of elbow ROM. Seventy-six orthopedic surgeons agreed to participate in the study and survey was performed by a direct interview manner in the annual meetings of Korean Pediatric Orthopedic Association and Korean Society for Surgery of the Hand. There were 17 pediatric orthopedic surgeons, 48 hand surgeons, and 11 general orthopedic surgeons.
RESULTS
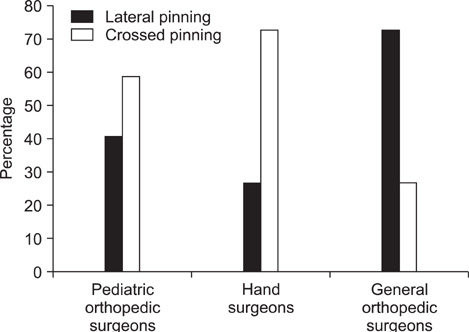
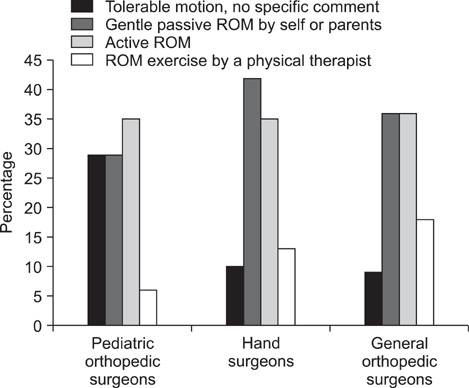
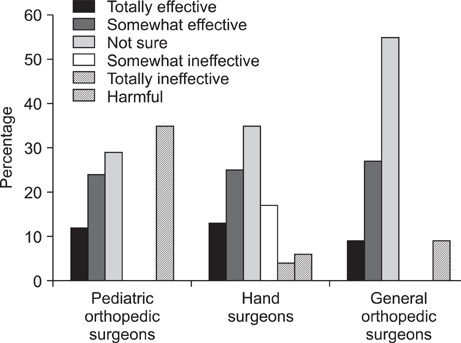
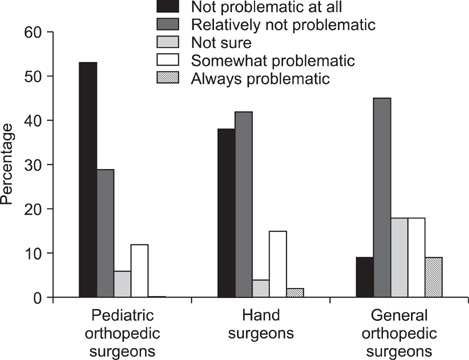
Ninety-six percent of the orthopedic surgeons agreed that closed reduction and percutaneous pinning was the treatment of choice for the displaced supracondylar fracture of the humerus in children. They showed significant difference in the choice of pin entry (lateral vs. crossed pinning, p = 0.017) between the three groups of orthopedic surgeons, but no significant difference was found in the number of pins, all favoring 2 pins over 3 pins. Most of the orthopedic surgeons used a removable splint during the ROM exercise period. Hand surgeons and general orthopedic surgeons tended to be more concerned about elbow stiffness after supracondylar fracture than pediatric orthopedic surgeons, and favored gentle passive ROM exercise as elbow motion. Pediatric orthopedic surgeons most frequently adopted active ROM exercise as the elbow motion method. Pediatric orthopedic surgeons and general orthopedic surgeons acknowledged that the patient's age was the most contributing factor to the restoration of elbow motion, whereas hand surgeons acknowledged the amount of injury to be the most contributing factor.
CONCLUSIONS
More investigation and communication will be needed to reach a consensus in treating pediatric supracondylar fractures of the humerus between the different subspecialties of orthopedic surgeons, which can minimize malpractice and avoid medicolegal issues.
MeSH Terms
-
Age Factors
Attitude of Health Personnel
Bone Nails
Chi-Square Distribution
Child
Consensus
Elbow Joint/physiology
Exercise Therapy/*methods
Fracture Fixation, Internal/*methods
Humans
Humeral Fractures/rehabilitation/*surgery
Orthopedics
Questionnaires
*Range of Motion, Articular
Splints
Statistics, Nonparametric
Time Factors
Figure
Reference
-
1. Beaty JH, Kasser JR, Skaggs DL, Flynn JM, Waters PM. Rockwood and Wilkins' fractures in children. 2007. 7th ed. Philadelphia: Lippincott Williams & Wilkins.2. Farley FA, Patel P, Craig CL, et al. Pediatric supracondylar humerus fractures: treatment by type of orthopedic surgeon. J Child Orthop. 2008. 2(2):91–95.
Article3. Zamzam MM, Bakarman KA. Treatment of displaced supracondylar humeral fractures among children: crossed versus lateral pinning. Injury. 2009. 40(6):625–630.
Article4. Zionts LE, Woodson CJ, Manjra N, Zalavras C. Time of return of elbow motion after percutaneous pinning of pediatric supracondylar humerus fractures. Clin Orthop Relat Res. 2009. 467(8):2007–2010.
Article5. Iobst CA, Spurdle C, King WF, Lopez M. Percutaneous pinning of pediatric supracondylar humerus fractures with the semisterile technique: the Miami experience. J Pediatr Orthop. 2007. 27(1):17–22.
Article6. Ponce BA, Hedequist DJ, Zurakowski D, Atkinson CC, Waters PM. Complications and timing of follow-up after closed reduction and percutaneous pinning of supracondylar humerus fractures: follow-up after percutaneous pinning of supracondylar humerus fractures. J Pediatr Orthop. 2004. 24(6):610–614.
Article7. Flynn JM, Sarwark JF, Waters PM, Bae DS, Lemke LP. The surgical management of pediatric fractures of the upper extremity. Instr Course Lect. 2003. 52:635–645.8. Nacht JL, Ecker ML, Chung SM, Lotke PA, Das M. Supracondylar fractures of the humerus in children treated by closed reduction and percutaneous pinning. Clin Orthop Relat Res. 1983. (177):203–209.
Article9. Brauer CA, Lee BM, Bae DS, Waters PM, Kocher MS. A systematic review of medial and lateral entry pinning versus lateral entry pinning for supracondylar fractures of the humerus. J Pediatr Orthop. 2007. 27(2):181–186.
Article10. Murtezani A, Pustina A, Bytyci C, Hundozi H. Rehabilitation of children after elbow injuries. Niger J Med. 2007. 16(2):138–142.
Article11. Keppler P, Salem K, Schwarting B, Kinzl L. The effectiveness of physiotherapy after operative treatment of supracondylar humeral fractures in children. J Pediatr Orthop. 2005. 25(3):314–316.
Article12. Reitman RD, Waters P, Millis M. Open reduction and internal fixation for supracondylar humerus fractures in children. J Pediatr Orthop. 2001. 21(2):157–161.
Article13. Otsuka NY, Kasser JR. Supracondylar fractures of the humerus in children. J Am Acad Orthop Surg. 1997. 5(1):19–26.
Article14. Lee SS, Mahar AT, Miesen D, Newton PO. Displaced pediatric supracondylar humerus fractures: biomechanical analysis of percutaneous pinning techniques. J Pediatr Orthop. 2002. 22(4):440–443.
Article15. Lee YH, Lee SK, Kim BS, et al. Three lateral divergent or parallel pin fixations for the treatment of displaced supracondylar humerus fractures in children. J Pediatr Orthop. 2008. 28(4):417–422.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Flexion-type Humerus Supracondylar Fractures in Children
- Treatment of Supracondylar Fractures of the Humerus in Children by Open Reduction
- Treatment of Supracondylar Fracture of the Humerus in Children: by Immediate Closed Reduction & Lateral Percutaneous K-Wire Fixation
- Treatment of Displaced Extension type Supracondylar Fractures of the Humerus in Children by Percutaneous Pining or Open Reduction
- A Clinical Study of Supracondylar Fracture of the Humerus in Children