Korean J Radiol.
2010 Dec;11(6):603-611. 10.3348/kjr.2010.11.6.603.
Endovascular Treatment of Traumatic Pseudoaneurysm Presenting as Intractable Epistaxis
- Affiliations
-
- 1Department of Neurosurgery, West China Hospital, Sichuan University, Chengdu, Sichuan 610041, People's Republic of China. zcwazq@sina.com
- KMID: 1119222
- DOI: http://doi.org/10.3348/kjr.2010.11.6.603
Abstract
OBJECTIVE
To investigate the clinical efficacy of individual endovascular management for the treatment of different traumatic pseudoaneurysms presenting as intractable epistaxis.
MATERIALS AND METHODS
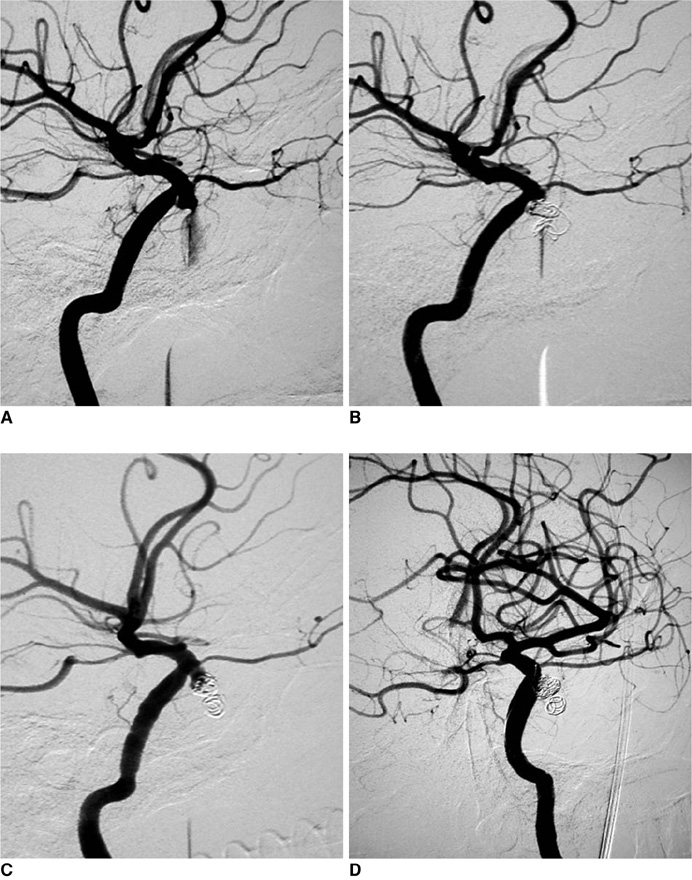
For 14 consecutive patients with traumatic pseudoaneurysm presenting as refractory epistaxes, 15 endovascular procedures were performed. Digital subtraction angiography revealed that the pseudoaneurysms originated from the internal maxillary artery in eight patients; and all were treated with occlusion of the feeding artery. In six cases, they originated from the internal carotid artery (ICA); out of which, two were managed with detachable balloons, two with covered stents, one by means of cavity embolization, and the remaining one with parent artery occlusion. All of these cases were followed up clinically from six to 18 months, with a mean follow up time of ten months; moreover, three cases were also followed with angiography.
RESULTS
Complete cessation of bleeding was achieved in all the 15 instances (100%) immediately after the endovascular therapies. Of the six patients who suffered from ICA pseudoaneurysms, one presented with a permanent stroke and one had an episode of rebleeding requiring intervention.
CONCLUSION
In patients presenting with a history of craniocerebral trauma, traumatic pseudoaneurysm must be considered as a differential diagnosis. Individual endovascular treatment is a relatively safe, plausible, and reliable means of managing traumatic pseudoaneurysms.
Keyword
MeSH Terms
-
Adolescent
Adult
Aneurysm, False/radiography/*therapy
Angiography, Digital Subtraction
Angioplasty, Balloon
Carotid Artery Injuries/radiography/*therapy
Carotid Artery, Internal
Diagnosis, Differential
Embolization, Therapeutic
Endovascular Procedures/*methods
Epistaxis/radiography/*therapy
Female
Humans
Male
Maxillary Artery/*injuries
Middle Aged
Retrospective Studies
Stents
Tomography, X-Ray Computed
Treatment Outcome
Figure
Reference
-
1. Tan LK, Calhoun KH. Epistaxis. Med Clin North Am. 1999. 83:43–56.2. Viducich RA, Blanda MP, Gerson LW. Posterior epistaxis: clinical features and acute complications. Ann Emerg Med. 1995. 25:592–596.3. Sokoloff J, Wickbom I, McDonald D, Brahme F, Goergen TC, Goldberer LE. Therapeutic percutaneous embolization in intractable epistaxis. Radiology. 1974. 111:285–287.4. Quintana F, Diez C, Gutierrez A, Diez ML, Austin O, Vazquez A. Traumatic aneurysm of the basilar artery. AJNR Am J Neuroradiol. 1996. 17:283–285.5. Karamoskos P, Dohrmann PJ. Traumatic internal carotid artery aneurysm and massive epistaxis. Aust N Z J Surg. 1989. 59:745–747.6. Auyeung KM, Lui WM, Chow LC, Chan FL. Massive epistaxis related to petrous carotid artery pseudoaneurysm after radiation therapy: emergency treatment with covered stent in two cases. AJNR Am J Neuroradiol. 2003. 24:1449–1452.7. Nishioka H, Ohno S, Ikeda Y, Ohashi T, Haraoka J. Delayed massive epistaxis following endonasal transsphenoidal surgery. Acta Neurochir (Wien). 2007. 149:523–526.8. Chen D, Concus AP, Halbach VV, Cheung SW. Epistaxis originating from traumatic pseudoaneurysm of the internal carotid artery: diagnosis and endovascular therapy. Laryngoscope. 1998. 108:326–331.9. Feiz-Erfan I, Horn EM, Theodore N, Zabramski JM, Klopfenstein JD, Lekovic GP, et al. Incidence and pattern of direct blunt neurovascular injury associated with trauma to the skull base. J Neurosurg. 2007. 107:364–369.10. Lasjaunias P, Marsot-Dupuch K, Doyon D. The radio-anatomical basis of arterial embolisation for epistaxis. J Neuroradiol. 1979. 6:45–53.11. Cockroft KM, Carew JF, Trost D, Fraser RA. Delayed epistaxis resulting from external carotid artery injury requiring embolization: a rare complication of transsphenoidal surgery: case report. Neurosurgery. 2000. 47:236–239.12. Nishioka H, Haraoka J, Ikeda Y. Risk factors of cerebrospinal fluid rhinorrhea following transsphenoidal surgery. Acta Neurochir (Wien). 2005. 147:1163–1166.13. Fontela PS, Tampieri D, Atkinson JD, Daniel SJ, Teitelbaum J, Shemie SD. Posttraumatic pseudoaneurysm of the intracavernous internal carotid artery presenting with massive epistaxis. Pediatr Crit Care Med. 2006. 7:260–262.14. Renn WH, Rhoton AL Jr. Microsurgical anatomy of the sellar region. J Neurosurg. 1975. 43:288–298.15. Song HH, Won YD, Kim YJ, Kim BS. The endovascular management of saccular posterior inferior cerebellar artery aneurysms. Korean J Radiol. 2008. 9:396–400.16. Bavinzski G, Killer M, Knosp E, Ferraz-Leite H, Gruber A, Richling B. False aneurysms of the intracavernous carotid artery--report of 7 cases. Acta Neurochir (Wien). 1997. 139:37–43.17. Eckert B, Thie A, Carvajal M, Groden C, Zeumer H. Predicting hemodynamic ischemia by transcranial Doppler monitoring during therapeutic balloon occlusion of the internal carotid artery. AJNR Am J Neuroradiol. 1998. 19:577–582.18. Goleas J, Mikhael MA, Paige ML, Wolff AP. Intracavernous carotid artery aneurysm presenting as recurrent epistaxis. Ann Otol Rhinol Laryngol. 1991. 100:577–579.19. Quintana F, Diez C, Gutierrez A, Diez ML, Austin O, Vazquez A. Traumatic aneurysm of the basilar artery. AJNR Am J Neuroradiol. 1996. 17:283–285.20. Karamoskos P, Dohrmann PJ. Traumatic internal carotid artery aneurysm and massive epistaxis. Aust N Z J Surg. 1989. 59:745–747.21. Lempert TE, Halbach VV, Higashida RT, Dowd CF, Urwin RW, Balousek PA, et al. Endovascular treatment of pseudoaneurysms with electrolytically detachable coils. AJNR Am J Neuroradiol. 1998. 19:907–911.22. Struffert T, Buhk JH, Buchfelder M, Rohde V, Doerfler A, Knauth M. Coil migration after endovascular coil occlusion of internal carotid artery pseudoaneurysms within the sphenoid sinus. Minim Invasive Neurosurg. 2009. 52:89–92.23. Celil G, Engin D, Orhan G, Barbaros C, Hakan K, Adil E. Intractable epistaxis related to cavernous carotid artery pseudoaneurysm: treatment of a case with covered stent. Auris Nasus Larynx. 2004. 31:275–278.24. Choi SY, Won JY, Lee do Y, Choi D, Shim WH, Lee KH. Percutaneous transabdominal approach for the treatment of endoleaks after endovascular repair of infrarenal abdominal aortic aneurysm. Korean J Radiol. 2010. 11:107–114.25. Li MH, Li YD, Gao BL, Fang C, Luo QY, Cheng YS, et al. A new covered stent designed for intracranial vasculature: application in the management of pseudoaneurysms of the cranial internal carotid artery. AJNR Am J Neuroradiol. 2007. 28:1579–1585.26. Ruiz-Juretschke F, Castro E, Mateo Sierra O, Iza B, Manuel Garbizu J, Fortea F. Massive epistaxis resulting from an intracavernous internal carotid artery traumatic pseudoaneurysm: complete resolution with overlapping uncovered stents. Acta Neurochir (Wien). 2009. 151:1681–1684.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Traumatic Pseudoaneurysm of the External and Internal Carotid Artery Presenting as Epistaxis: Case Report
- Internal Carotid Artery Pseudoaneurysm in a Patient Presenting With Recurrent Epistaxis: A Case Report and Literature Review
- Technical Pitfalls in the Endovascular Treatment of Traumatic Pseudoaneurysm of the Internal Carotid Artery: Case Report
- Endovascualr Treatment for Traumatic Giant Pseudoaneurysm of Internal Carotid Artery
- Comprehensive understanding of vascular anatomy for endovascular treatment of intractable oronasal bleeding