Korean J Ophthalmol.
2009 Sep;23(3):228-231. 10.3341/kjo.2009.23.3.228.
Acute Comitant Esotropia in a Child With a Cerebellar Tumor
- Affiliations
-
- 1Department of Ophthalmology, College of Medicine, Catholic University of Daegu, Daegu, Korea. kimsy@cu.ac.kr
- KMID: 1115760
- DOI: http://doi.org/10.3341/kjo.2009.23.3.228
Abstract
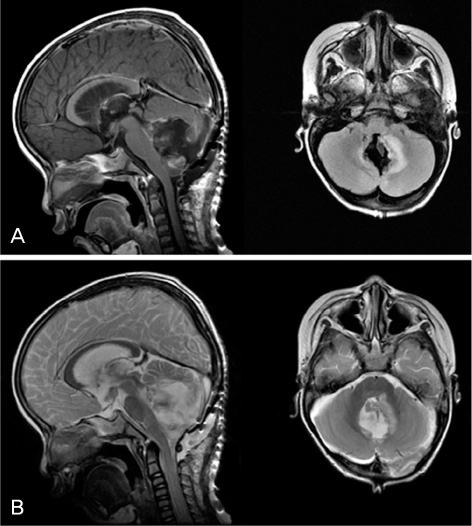
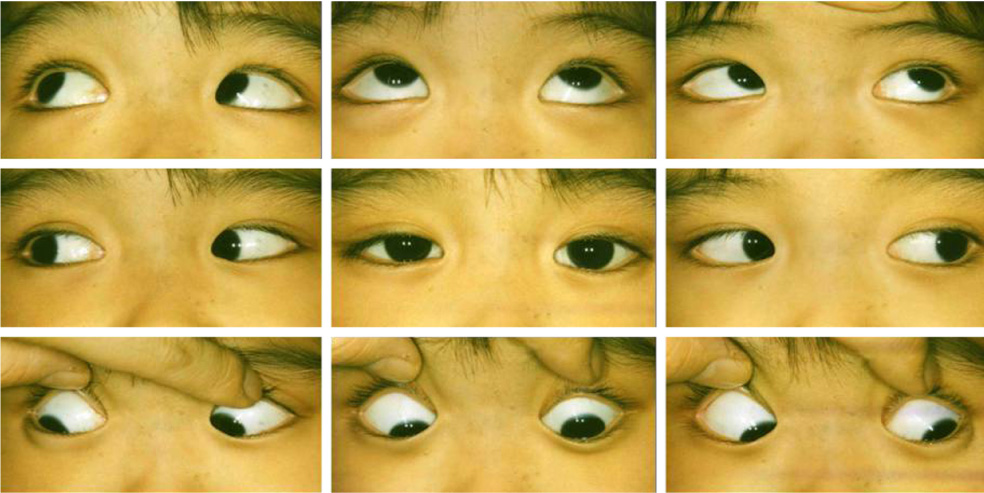
- We report a case of acute comitant esotropia in a child with a cerebellar tumor. A 3-year-old boy was referred for management of a 9 month history of acute acquired comitant esotropia. On first presentation, the patient's angle of esodeviation was 50 prism-diopters (PD) at distance and near fixation without any lateral incomitance. The cycloplegic refraction revealed +0.75 diopters in both eyes. Very mild bilateral papilledema was found on the fundus examination, but the neurological examination did not reveal any other pathological findings. Brain MRI showed a 5 cm mass located in the midline of the cerebellum as well as hydrocephalus. The mass was completely excised and histological examination confirmed the diagnosis of pilocytic astrocytoma. Despite neurosurgery, the patient's strabismus remained unresolved. One year after neurosurgery, both medial rectus muscles were surgically recessed by 6 mm, resulting in esotropia of 8PD at distant and near fixation without restoration of bifoveal fusion at follow-up 2 years after the eye muscle surgery. Therefore, acute onset comitant esotropia in a child can be the first sign of a cerebellar tumor, even without any other neurological signs and symptoms.
Keyword
MeSH Terms
-
Acute Disease
Astrocytoma/*complications/surgery
Brain/pathology
Cerebellar Neoplasms/*complications/diagnosis/surgery
Child, Preschool
Esotropia/*etiology/pathology/physiopathology/surgery
Humans
Magnetic Resonance Imaging
Male
Neurosurgical Procedures
Oculomotor Muscles/surgery
Refraction, Ocular
Time Factors
Figure
Cited by 1 articles
-
Clinical Characteristics and Outcomes of Smartphone Overusers with Acute Acquired Comitant Esotropia
Jiho Song, Sa Kang Kim, Mi Young Choi
J Korean Ophthalmol Soc. 2018;59(2):169-175. doi: 10.3341/jkos.2018.59.2.169.
Reference
-
1. von Noorden GK, Campos EC. Binocular vision and ocular motility: Theory and management of strabismus. 2002. 6th ed. St Louis: C.V. Mosby Company;338.2. Watson AP, Fielder AR. Sudden-onset squint. Dev Med Child Neurol. 1987. 29:207–211.3. Anderson WD, Lubow M. Astrocytoma of the corpus callosum presenting with acute comitant esotropia. Am J Ophthalmol. 1970. 69:594–598.4. Bixenman WW, Laguna JF. Acquired esotropia as initial manifestation of Arnold-Chiari malformation. J Pediatr Ophthalmol Strabismus. 1987. 24:83–86.5. Williams AS, Hoyt CS. Acute comitant esotropia in children with brain tumors. Arch Ophthalmol. 1989. 107:376–378.6. Astle WF, Miller SJ. Acute comitant esotropia: a sign of intracranial disease. Can J Ophthalmol. 1994. 29:151–154.7. Simon JW, Waldman JB, Couture KC. Cerebellar astrocytoma manifesting as isolated, comitant esotropia in childhood. Am J Ophthalmol. 1996. 121:584–586.8. Lewis AR, Kline LB, Sharpe JA. Acquired esotropia due to Arnold-Chiari I malformation. J Neuroophthlmol. 1996. 16:49–54.9. Liu GT, Hertle RW, Quinn GE, Schaffer DB. Comitant esodeviation resulting from neurologic insult in children. J AAPOS. 1997. 1:143–146.10. Lennerstrand G. Central motor control in concomitant strabismus. Graefes Arch Clin Exp Ophthalmol. 1988. 226:172–174.11. Hoyt CS, Good WV. Acute comitant esotropia: when is it a sign of serious neurologic disease? Br J Ophthalmol. 1995. 79:498–501.12. Jampolsky A. Ocular divergence mechanisms. Trans Am Ophthalmol Soc. 1970. 68:730–822.13. Flynn JT. Problems in strabismus management. Trans New Orleans Acad Ophthalmol. 1986. 34:449–460.14. Kirkham TH, Bird AC, Sanders MD. Divergence paralysis with raised intracranial pressure. An electro-oculographic study. Br J Ophthalmol. 1972. 56:776–782.15. Bixenman WW, von Noorden GK. Benign recurrentVI nerve palsy in childhood. J Pediatr Ophthalmol Strabismus. 1981. 18:29–34.16. Dikici K, Cicik E, Akman C, et al. Cerebellar astrocytoma presenting with acute esotropia in a 5 year-old girl. Int Ophthalmol. 2001. 23:167–170.17. Zweifach PH. Childhood esotropia with delayed appearance of cerebellar tumor. Neuroophthalmology. 1981. 1:291–293.18. Musazadeh M, Hartmann K, Simon F. Late onset esotropia as first symptom of a cerebellar tumor. Strabismus. 2004. 12:119–123.19. Lyons CJ, Tiffin PA, Oystreck D. Acute acquired comitant esotropia: a prospective study. Eye. 1999. 13:617–620.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Acute Acquired Comitant Esotropia Associated with Chiari I Malformation
- Two Cases of Acute Acquired Comitant Esotropia after Occlusion Therapy
- Two Cases of Acute Acquired Comitant Esotropia
- Clinical Aspect of Acute Comitant Esotropia
- Clinical Characteristics and Outcomes of Smartphone Overusers with Acute Acquired Comitant Esotropia