Korean J Radiol.
2006 Sep;7(3):173-179. 10.3348/kjr.2006.7.3.173.
CT Analysis of the Anterior Mediastinum in Idiopathic Pulmonary Fibrosis and Nonspecific Interstitial Pneumonia
- Affiliations
-
- 1Department of Radiology and the Institute of Radiation Medicine, Seoul National University College of Medicine, Clinical Research Institute, Seoul National University Hospital, Seoul, Korea. rosaceci@radiol.snu.ac.kr
- 2Department of Radiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul 138-736, Korea.
- KMID: 1114349
- DOI: http://doi.org/10.3348/kjr.2006.7.3.173
Abstract
OBJECTIVE
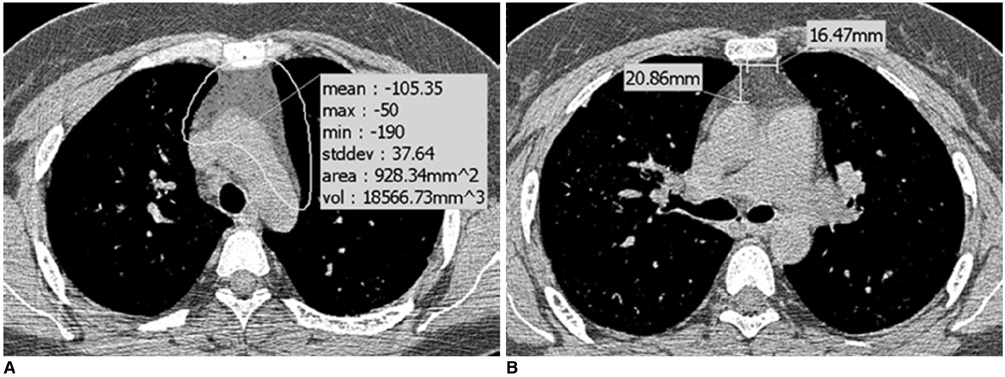
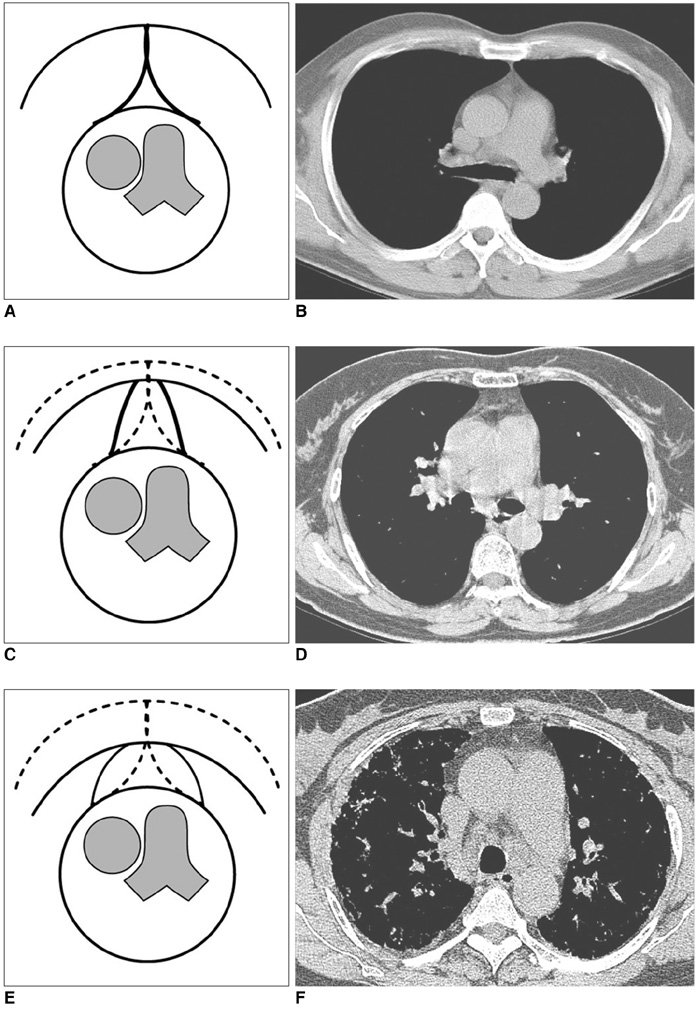
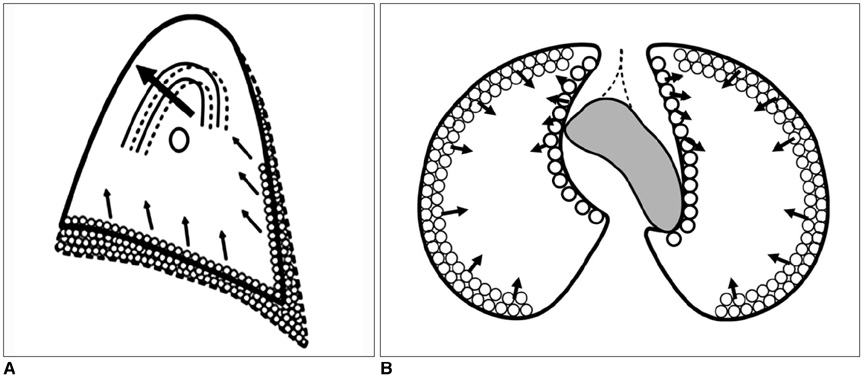
We wanted to determine whether the amount and shape of the anterior mediastinal fat in the patients suffering with usual interstitial pneumonia (UIP) or nonspecific interstitial pneumonia (NSIP) was different from those of the normal control group. MATERIALS AND METHODS: We selected patients who suffered with UIP (n = 26) and NSIP (n = 26) who had undergone CT scans. Twenty-six controls were selected from individuals with normal CT findings and normal pulmonary function tests. All three groups (n = 78) were individually matched for age and gender. The amounts of anterior mediastinal fat, and the retrosternal anteroposterior (AP) and transverse dimensions of the anterior mediastinal fat were compared by one-way analysis of variance and Bonferroni's test. The shapes of the anterior mediastinum were compared using the Chi-square test. Exact logistic regression analysis and polychotomous logistic regression analysis were employed to assess whether the patients with NSIP or UIP had a tendency to show a convex shape of their anterior mediastinal fat. RESULTS: The amount of anterior mediastinal fat was not different among the three groups (p = 0.175). For the UIP patients, the retrosternal AP dimension of the anterior mediastinal fat was shorter (p = 0.037) and the transverse dimension of the anterior mediastinal fat was longer (p = 0.001) than those of the normal control group. For the NSIP patients, only the transverse dimension was significantly longer than those of the normal control group (p < 0.001). The convex shape of the anterior mediastinum was predictive of NSIP (OR = 19.7, CI 3.32-infinity, p < 0.001) and UIP (OR = 24.42, CI 4.06-infinity, p < 0.001). CONCLUSION: For UIP patients, the retrosternal AP and transverse dimensions are different from those of normal individuals, whereas the amounts of anterior mediastinal fat are similar. UIP and NSIP patients have a tendency to have a convex shape of their anterior mediastinal fat.
Keyword
MeSH Terms
Figure
Reference
-
1. Proto AV. Conventional chest radiographs: anatomic understanding of newer observations. Radiology. 1992. 183:593–603.2. McLoud TC, Isler RJ, Novelline RA, Putman CE, Simeone J, Stark P. The apical cap. AJR Am J Roentgenol. 1981. 137:299–306.3. Im JG, Webb WR, Han MC, Park JH. Apical opacity associated with pulmonary tuberculosis: high-resolution CT findings. Radiology. 1991. 178:727–731.4. Fisher ER, Godwin JD. Extrapleural fat collections: pseudotumors and other confusing manifestations. AJR Am J Roentgenol. 1993. 161:47–52.5. Toei H, Furuse M, Shinozaki T, Sohara Y. Computed tomography analysis of the anterior mediastinal fat after upper lobectomy. Invest Radiol. 1997. 32:174–179.6. This joint statement of the American Thoracic Society (ATS), and the European Respiratory Society (ERS) was adopted by the ATS board of directors, June 2001 and by the ERS Executive Committee, June 2001. American Thoracic Society/European Respiratory Society International Multidisciplinary Consensus Classification of the Idiopathic Interstitial Pneumonias. Am J Respir Crit Care Med. 2002. 165:277–304.7. Yoshizumi T, Nakamura T, Yamane M, Islam AH, Menju M, Yamasaki K, et al. Abdominal fat: standardized technique for measurement at CT. Radiology. 1999. 211:283–286.8. Teates CD. Steroid-induced mediastinal lipomatosis. Radiology. 1970. 96:501–502.9. Koerner HJ, Sun DI. Mediastinal lipomatosis secondary to steroid therapy. Am J Roentgenol Radium Ther Nucl Med. 1966. 98:461–464.10. Felson B. Pulmonary agenesis and related anomalies. Semin Roentgenol. 1972. 7:17–30.11. Ang JG, Proto AV. CT demonstration of congenital pulmonary venolobar syndrome. J Comput Assist Tomogr. 1984. 8:753–757.12. Johkoh T, Müller NL, Cartier Y, Kavanagh PV, Hartman TE, Akira M, et al. Idiopathic interstitial pneumonias: diagnostic accuracy of thin-section CT in 129 patients. Radiology. 1999. 211:555–560.13. MacDonald SL, Rubens MB, Hansell DM, Copley SJ, Desai SR, du Bois RM, et al. Nonspecific interstitial pneumonia and usual interstitial pneumonia: comparative appearances at and diagnostic accuracy of thin-section CT. Radiology. 2001. 221:600–605.14. Hartman TE, Swensen SJ, Hansell DM, Colby TV, Myers JL, Tazelaar HD, et al. Nonspecific interstitial pneumonia: variable appearance at high-resolution chest CT. Radiology. 2000. 217:701–705.15. Daniil ZD, Gilchrist FC, Nicholson AG, Hansell DM, Harris J, Colby TV, et al. A histologic pattern of nonspecific interstitial pneumonia is associated with a better prognosis than usual interstitial pneumonia in patients with cryptogenic fibrosing alveolitis. Am J Respir Crit Care Med. 1999. 160:899–905.16. Flaherty KR, Travis WD, Colby TV, Toews GB, Kazerooni EA, Gross BH, et al. Histologic variability in usual and nonspecific interstitial pneumonias. Am J Respir Crit Care Med. 2001. 164:1722–1727.17. Travis WD, Matsui K, Moss J, Ferrans VJ. Idiopathic nonspecific interstitial pneumonia: prognostic significance of cellular and fibrosing patterns: survival comparison with usual interstitial pneumonia and desquamative interstitial pneumonia. Am J Surg Pathol. 2000. 24:19–33.18. Jeong YJ, Lee KS, Müller NL, Chung MP, Chung MJ, Han J, et al. Usual interstitial pneumonia and non-specific interstitial pneumonia: serial thin-section CT findings correlated with pulmonary function. Korean J Radiol. 2005. 6:143–152.19. Best AC, Lynch AM, Bozic CM, Miller D, Grunwald GK, Lynch DA. Quantitative CT indexes in idiopathic pulmonary fibrosis: relationship with physiologic impairment. Radiology. 2003. 228:407–414.20. Müller NL, Staples CA, Miller RR, Vedal S, Thurlbeck WM, Ostrow DN. Disease activity in idiopathic pulmonary fibrosis: CT and pathologic correlation. Radiology. 1987. 165:731–734.21. Müller NL, Miller RR, Webb WR, Evans KG, Ostrow DN. Fibrosing alveolitis: CT-pathologic correlation. Radiology. 1986. 160:585–588.22. Remy-Jardin M, Giraud F, Remy J, Copin MC, Gosselin B, Duhamel A. Importance of ground-glass attenuation in chronic diffuse infiltrative lung disease: pathologic-CT correlation. Radiology. 1993. 189:693–698.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Idiopathic Interstitial Pneumonias: Radiologic Findings
- Idiopathic Pulmonary Fibrosis and Nonspecific Interstitial Pneumonia
- Clinical Year in Review of Interstitial Lung Diseases: Focused on Idiopathic Interstitial Pneumonia
- A Case of Nonspecific Interstitial Pneumonia with Clinical Course of Rapid Aggravation
- Radiologic Approach to the Idiopathic Interstitial Pneumonias