Korean J Ophthalmol.
2011 Apr;25(2):146-150. 10.3341/kjo.2011.25.2.146.
A Case of Optic Nerve Atrophy with Severe Disc Cupping after Methanol Poisoning
- Affiliations
-
- 1Department of Ophthalmology, Hanyang University College of Medicine, Seoul, Korea. kbuhm@hanyang.ac.kr
- KMID: 1111880
- DOI: http://doi.org/10.3341/kjo.2011.25.2.146
Abstract
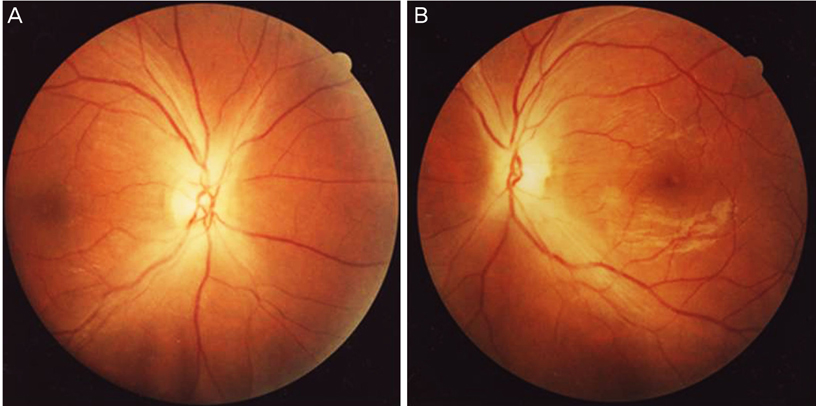
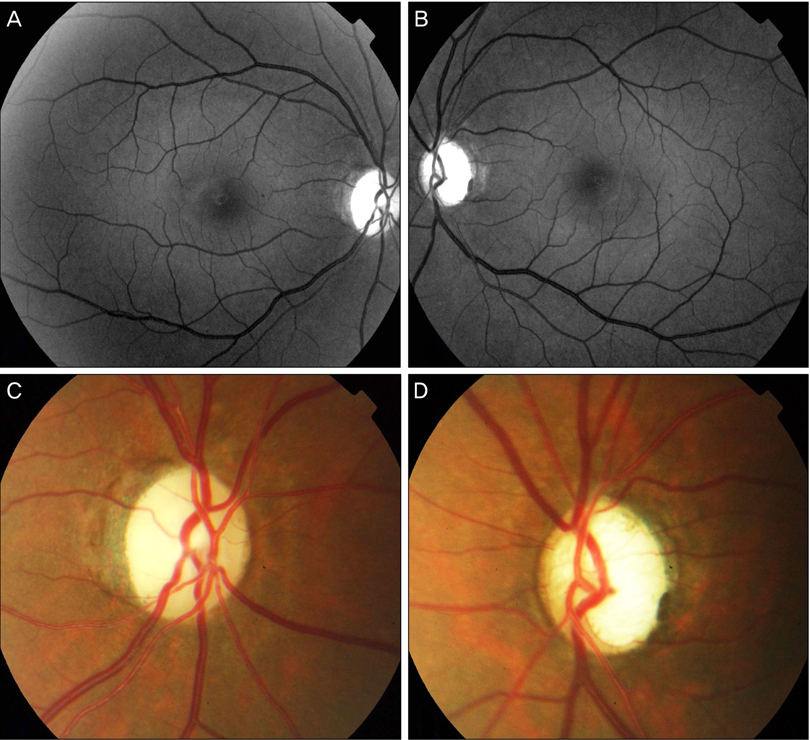
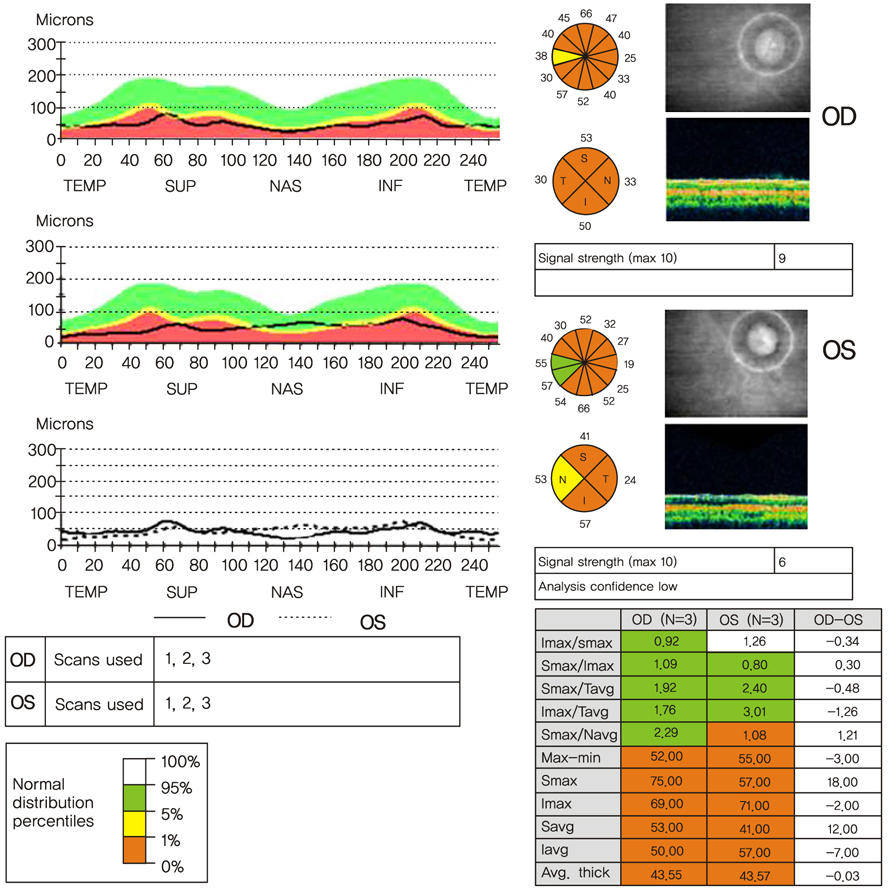
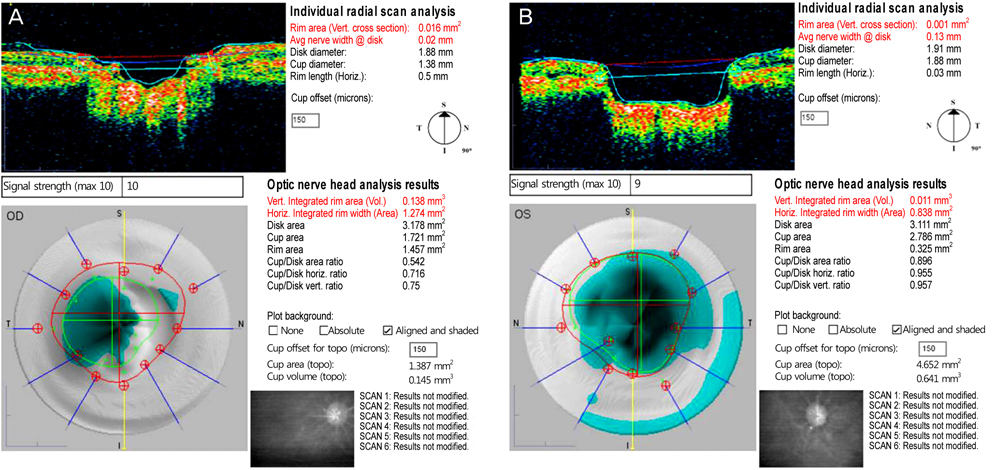
- We report a rare case of optic nerve atrophy with severe disc cupping resulting from methanol poisoning. A 30-year-old man presented to the hospital complaining of decreased visual acuity in both eyes a day after drinking alcohol containing methanol. His initial visual acuity allowed for only visualizing hand motion and not corrected in either eye. Initial intraocular pressure was within normal limits in both eyes. Initial fundus examination showed optic disc swelling in both eyes. Four years later, he visited our hospital for an eye evaluation. Visual acuity in both eyes still only allowed for visualizing hand motion. No nystagmus was observed in either eye during the optokinetic nystagmus test, and no waves were found in a visual evoked potential test. No specific change was noted on brain magnetic resonance imaging. On fundus examination, there was disc pallor in both eyes and disc cupping with a high cup/disc (C/D) ratio above 0.9 in the left eye. C/D ratio of the right eye was 0.5. Methanol poisoning may induce glaucomatous disc cupping in the late stage as well as optic atrophy. One possible mechanism of disc cupping is ganglion cell loss due to acute demyelination of the retrobulbar optic nerve. This report is the first photographic evidence of methanol induced optic disc cupping in Korea.
Keyword
MeSH Terms
-
Adult
Diagnosis, Differential
Evoked Potentials, Visual
Fluorescein Angiography
Fundus Oculi
Humans
Magnetic Resonance Imaging
Male
Methanol/*poisoning
Optic Atrophy/*chemically induced/pathology/physiopathology
Optic Disk/drug effects/*pathology
Papilledema/*chemically induced/pathology/physiopathology
Severity of Illness Index
Solvents/poisoning
Tomography, Optical Coherence
Visual Acuity
Figure
Cited by 1 articles
-
Letter to the Editor: A Case of Optic Nerve Atrophy with Severe Disc Cupping after Methanol Poisoning
Hossein Sanaei-Zadeh, Nasim Zamani
Korean J Ophthalmol. 2011;25(6):463-463. doi: 10.3341/kjo.2011.25.6.463.
Reference
-
1. Jacobsen D, McMartin KE. Methanol and ethylene glycol poisonings. Mechanism of toxicity, clinical course, diagnosis and treatment. Med Toxicol. 1986. 1:309–334.2. Benton CD Jr, Calhoun EP Jr. The ocular effects of methyl alcohol poisoning: report of a catastrophe involving 320 persons. Am J Ophthalmol. 1953. 36:1677–1685.3. Becker CE. Methanol poisoning. J Emerg Med. 1983. 1:51–58.4. Fink WH. The ocular pathology of methyl alcohol poisoning. Trans Am Ophthalmol Soc. 1942. 40:439–498.5. Baumbach GL, Cancilla PA, Martin-Amat G, et al. Methyl alcohol poisoning. IV. Alterations of the morphological findings of the retina and optic nerve. Arch Ophthalmol. 1977. 95:1859–1865.6. Roe O. The ganglion cells of the retina in cases of methanol poisoning in human beings and experimental animals. Acta Ophthalmol (Copenh). 1948. 26:169–182.7. Sharma M, Volpe NJ, Dreyer EB. Methanol-induced optic nerve cupping. Arch Ophthalmol. 1999. 117:286.8. Stelmach MZ, O'Day J. Partly reversible visual failure with methanol toxicity. Aust N Z J Ophthalmol. 1992. 20:57–64.9. Lindenberg R, Walsh FB, Sacks JG. Neuropathology of vision: an atlas. 1973. Philadelphia: Lea and Febiger;118.10. Sharpe JA, Hostovsky M, Bilbao JM, Rewcastle NB. Methanol optic neuropathy: a histopathological study. Neurology. 1982. 32:1093–1100.11. Bang JS, Yang HS, Rho SS, Chang YH. A case of toxic amblyopia caused by methanol intoxication. J Korean Ophthalmol Soc. 2007. 48:1731–1735.12. Kong SM, Hwang BK, Lee HK. 2 Cases of toxic amblyopia caused by acute methanol poisoning. J Korean Ophthalmol Soc. 1982. 23:259–263.13. Hayreh MS, Hayreh SS, Baumbach GL, et al. Methyl alcohol poisoning III. Ocular toxicity. Arch Ophthalmol. 1977. 95:1851–1858.14. Rang HP, Dale MM, Ritter JM. Pharmacology. 1999. 4th ed. Edinburgh: Churchill Livingstone;628–629.15. Liesivuori J, Savolainen H. Methanol and formic acid toxicity: biochemical mechanisms. Pharmacol Toxicol. 1991. 69:157–163.16. Medeiros FA, Susanna R Jr. Retinal nerve fiber layer loss after traumatic optic neuropathy detected by scanning laser polarimetry. Arch Ophthalmol. 2001. 119:920–921.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Optic Atrophy following Methanol Poisoning
- Letter to the Editor: A Case of Optic Nerve Atrophy with Severe Disc Cupping after Methanol Poisoning
- On the Ratio to the Physiologic Cupping and Optic Disc. and Optic Disc
- Neurological Complications Resulting from Non-Oral Occupational Methanol Poisoning
- Reversal of Optic Disc Cupping in Adults with Advanced Glaucoma