Korean J Ophthalmol.
2006 Mar;20(1):13-17. 10.3341/kjo.2006.20.1.13.
Anterior Elevation Maps as the Screening Test for the Ablation Power of Previous Myopic Refractive Surgery
- Affiliations
-
- 1Department of Ophthalmology, Inha University College of Medicine, Incheon, Korea. jhoh9707@hanmail.net
- KMID: 1099067
- DOI: http://doi.org/10.3341/kjo.2006.20.1.13
Abstract
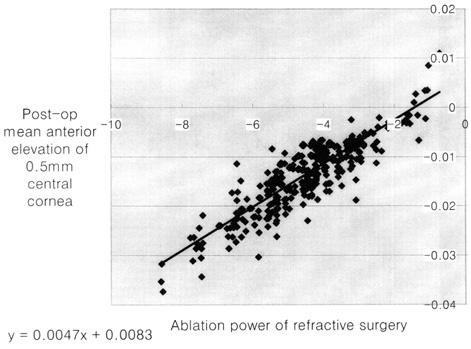
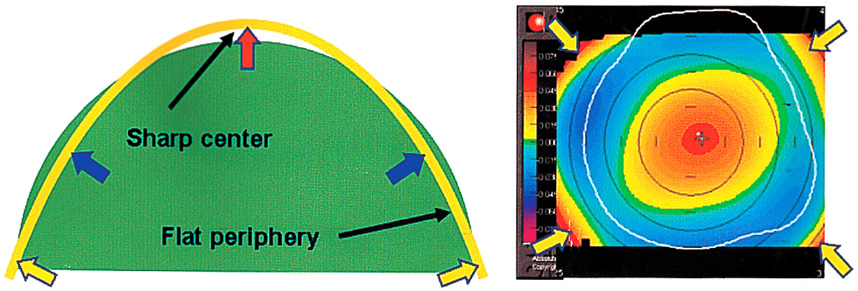
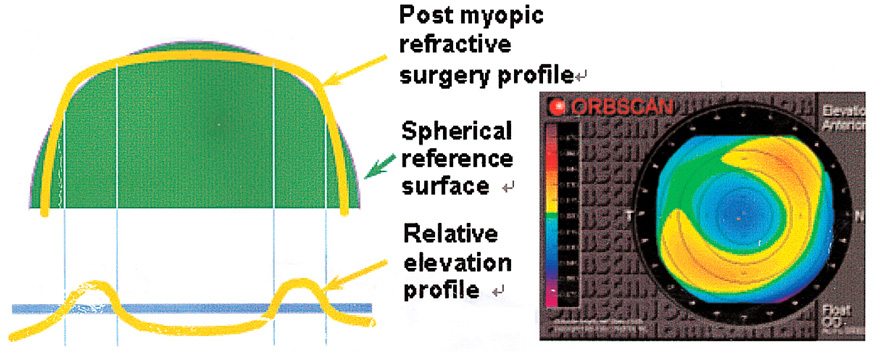
- PURPOSE: We classified the Orbscan anterior elevation maps in normal eyes (under myopic, emmetropic and hyperopic conditions) and in those after myopic refractive surgery. We did this classification to demonstrate how Orbscan anterior elevation maps are useful in screening for the existence and extent of previous myopic refractive surgery. Such a classification can help clinicians interpret preoperative and postoperative topographies. METHODS: We measured for visual acuity and refractive power in 4800 eyes. After a slit-lamp examination, a corneal topography exam was performed with an Orbscan corneal topography system. The eyes were divided into two groups, with Group I representing those who had not had refractive surgery (4438 eyes). Group II included those who had undergone previous refractive surgery to correct myopia (362 eyes). RESULTS: In Group I, the central island type (43.0%) was the most common, followed by the temporal ridge (25.8%), the with-the-rule regular ridge (16.7%), the against-the-rule regular ridge (6.6%), the nasal ridge (4.0%), and the saddle type (2.1%). In Group II, the depressed lake type (69.9%) was most common, followed by the de-centered ablation type (21.3%). The trend line of the postoperative central anterior surface elevation (E) and the ablation power of refractive surgery were calculated. Ablation power of refractive surgery=0.0047 E+0.0083 CONCLUSIONS: This study demonstrates that it is possible to use Orbscan anterior elevation maps to screen for the extent of previous refractory surgery used in the correction of myopia. This study may also be useful in understanding the shapes of Orbscan anterior elevation maps before and after myopic refractive surgery as well as in determining the degree of ablated myopic refractive power and decentration.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Screening of the Previous Photorefractive Surgery Using the Minimum Distance Between the Anterior Best Fit Sphere and the Center of the Anterior Corneal Surface
Lee Hoo Kim, Jae Hwan Lee, Jung Hyub Oh
J Korean Ophthalmol Soc. 2008;49(1):27-33. doi: 10.3341/jkos.2008.49.1.27.
Reference
-
1. Destrempes F, Brunette I, Meunier J, et al. Topography-based screening for previous laser in situ keratomileusis to correct myopia. J Cataract Refract Surg. 2002. 28:1644–1650.2. Bogan SJ, Waring GO 3rd, Ibrahim O, et al. Classification of normal corneal topography based on computer-assisted videokeratography. Arch Ophthalmol. 1990. 108:945–949.3. Naufal SC, Hess JS, Friedlander MH, Granet NS. Rasterstereography-based classification of normal corneas. J Cataract Refract Surg. 1997. 23:222–230.4. Dingeldein SA, Klyce SD, Wilson SE. Quantitative descriptors of corneal shape derived from computer-assisted analysis of photokeratographs. Refract Corneal Surg. 1989. 5:372–378.5. Hersh PS. A standardized classification of corneal topography after laser refractive surgery. J Refract Surg. 1997. 13:571–578.6. Abbas UL, Hersh PS. Early corneal topography patterns after excimer laser photorefractive keratectomy for myopia. J Refract Surg. 1999. 15:124–131.7. Hersh PS, Scher KS, Irani R. Corneal topography of photo-refractive keratectomy versus laser in situ keratomileusis. Summit PRK-LASIK Study Group. Ophthalmology. 1998. 105:612–619.8. Mootha VV, Dawson D, Kumar A, et al. Slitlamp, specular, and light microscopic findings of human donor corneas after laser-assisted in situ keratomileusis. Arch Ophthalmol. 2004. 122:686–692.9. Ousley PJ, Terry MA. Objective screening methods for prior refractive surgery in donor tissue. Cornea. 2002. 21:181–188.10. Hjortdal JO, Moller-Pedersen T, Ivarsen A, Ehlers N. Corneal power, thickness, and stiffness: results of a prospective randomized controlled trial of PRK and LASIK for myopia. J Cataract Refract Surg. 2005. 31:21–29.11. Priglinger SG, Neubauer AS, May CA, et al. Optical coherence tomography for the detection of laser in situ keratomileusis in donor corneas. Cornea. 2003. 22:46–50.12. Wolf AH, Neubauer AS, Priglinger SG, et al. Detection of laser in situ keratomileusis in a postmortem eye using optical coherence tomography. J Cataract Refract Surg. 2004. 30:491–495.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Classification of Anterior and Posterior Elevation and Axial Curvature Maps of Cornea using the Orbscan in Myopic Eyes
- Screening of the Previous Photorefractive Surgery Using the Minimum Distance Between the Anterior Best Fit Sphere and the Center of the Anterior Corneal Surface
- Comparison of Changes in Manifest Refraction and Orbscan Power Maps after Photorefractive Keratectomy and Laser in Situ Keratomileusis
- Agreement of Actual Corneal Power and Corneal Power Using Topography in Cataract Patients Undergone Refractive Surgery
- Intraocular Lens Power Calculation Using Shammas-PL Formula after Laser In-situ Keratomileusis