Korean J Ophthalmol.
2006 Jun;20(2):87-92. 10.3341/kjo.2006.20.2.87.
Visual Improvement in High Myopic Amblyopic Adult Eyes following Phakic Anterior Chamber Intraocular Lens Implantation
- Affiliations
-
- 1Department of Ophthalmology, Gachon Medical School, Gil Medical Center, Incheon, Korea. khshyn@gilhospital.com
- KMID: 1099041
- DOI: http://doi.org/10.3341/kjo.2006.20.2.87
Abstract
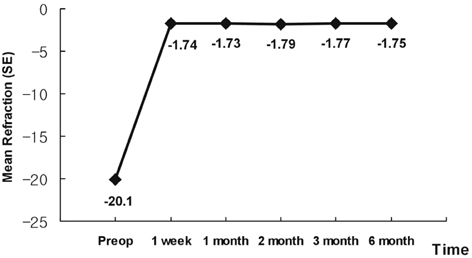
- PURPOSE: To evaluate the efficacy and safety of angle-supported phakic anterior chamber intraocular lenses in amblyopic adult eyes with very high myopia. METHODS: We evaluated 12 eyes in nine patients with very high myopic amblyopia who received angle-supported phakic intraocular lenses (Phakic 6H(R)) and followed them for more than six months. Uncorrected visual acuity (UCVA), best-corrected visual acuity (BCVA), and complications were evaluated. A satisfaction score was rated by patients using a 5-point (1~5) numeric scale. RESULTS: The mean age of patients was 37.3+/-9.4 years, ranging from 29 to 59 years old. The preoperative mean refraction (spherical equivalent, SE) was -20.10+/-5.41 diopters (D). The postoperative mean refraction (SE) was -1.75+/-0.76 D at six months. The postoperative BCVA improved an average 3.92+/-1.24 lines over preoperative values, and mean endothelial cell loss was 8.9% at six months. Development of cataracts, glaucoma, and pupil abnormalities were not demonstrated in any case during the study. The patients were all very satisfied, as the average satisfaction score was 4.3. CONCLUSIONS: This study indicates that angle-supported phakic anterior chamber intraocular lens implantation may be an effective surgical alternative for the correction of amblyopic adult eyes with very high myopia. However, long-term evaluation is necessary to assess possible complications and long-term safety.
Keyword
MeSH Terms
-
Visual Acuity/*physiology
Treatment Outcome
Severity of Illness Index
Retrospective Studies
Refraction, Ocular/*physiology
Myopia/complications/physiopathology/*surgery
Middle Aged
Male
Lens Implantation, Intraocular/*methods
Humans
Follow-Up Studies
Female
Anterior Chamber/*surgery
Amblyopia/complications/physiopathology/*surgery
Adult
Figure
Reference
-
1. Arne JL. Phakic intraocular lens implantation versus clear lens extraction in highly myopic eyes of 30- to 50-year-old patients. J Cataract Refract Surg. 2004. 30:2092–2096.2. Colin J, Robinet A, Cochener B. Retinal detachment after clear lens extraction for high myopia; seven-year follow-up. Ophthalmology. 1999. 106:2281–2284.3. Pineda-Fernandez A, Jaramillo J, Vargas J, et al. Phakic posterior chamber intraocular lens for high myopia. J Cataract Refract Surg. 2004. 30:2277–2283.4. Menezo JL, Peris-Martinez C, Cisneros AL, Martinez-Costa R. Phakic intraocular lenses to correct high myopia: Adatomed, Staar, and Artisan. J Cataract Refract Surg. 2004. 30:33–44.5. Lyle WA, Jin GJ. Laser in situ keratomileusis with the VISX star laser for myopia over 10.0 dipoters. J Cataract Refract Surg. 2001. 27:1812–1822.6. Sher NA, Barak M, Daya S. Excimer laser photorefractive keratectomy in high myopia; a multicenter study. Arch Ophthalmol. 1992. 110:935–943.7. Huber C. Effectiveness of intraocular lens calculation in high ametropia. J Cataract Refract Surg. 1989. 15:667–672.8. Pallikaris IG, Papatzanak ME, Stathi EZ. Laser in situ keratomileusis. Laser Surg Med. 1990. 10:463–468.9. Geggel HS, Talley AR. Delayed onset keratectasia following laser in situ keratomileusis and photorefractive keratectomy. Ophthalmology. 2000. 107:640–652.10. Holladay JT, Dudeja KR, Chang J. Functional vision and corneal changes after laser in situ keratomileusis determined by contrast sensitivity, glare testing, and corneal topography. J Cataract Refract Surg. 1999. 25:663–669.11. Oshika T, Klyce SD, Applegate RA, et al. Comparison of corneal wavefront aberrations after photorefractive keratectomy and laser in situ keratomileusis. Am J Ophthalmol. 1999. 127:1–7.12. Pesando PM, Ghiringhello MP, Tagliavacche P. Posterior chamber collamer phakic intraocular lens for myopia and hyperopia. J Refract Surg. 1999. 15:415–423.13. Allemann N, Chamon W, Tanaka HM, et al. Myopic angle-supported intraocular lenses: two-year follow-up. Ophthalmology. 2000. 107:1549–1554.14. The Implantable Contact Lens in Treatment of Myopia Study Group. U.S. Food and Drug Administration clinical trial of the Implantable Contact Lens for moderate to high myopia. Ophthalmology. 2003. 110:255–266.15. Smith RJ. A new method of estimating the depth of the anterior chamber. Br J Ophthalmol. 1979. 63:215–220.16. Waring GO 3rd, Lynn MJ, Nizam A, et al. The Perk Study Group. Results of the Prospective Evaluation of Radial Keratotomy (PERK) Study five years after surgery. Ophthalmology. 1991. 98:1164–1176.17. Buratto L, Ferrari M. Indications, techniques, results, limits, and complications of laser in situ keratomileusis. Curr Opin Ophthalmol. 1997. 8:59–66.18. Dutt S, Steinert RF, Raizman MB, Puliafito CA. One-year results of excimer laser photorefractive keratectomy for low to moderate myopia. Arch Ophthalmol. 1994. 112:1427–1436.19. Assetto V, Benedetti S, Pesando P. Collamer intraocular contact lens to correct high myopia. J Cataract Refract Surg. 1996. 22:551–556.20. Perez-Santonja JJ, Iradier MT, Benitez del Castillo JM, et al. Chronic subclinical inflammation in phakic eyes with intraocular lenses to correct myopia. J Cataract Refract Surg. 1996. 22:183–187.21. Alio JL, de la Hoz F, Perez-Santonja JJ, et al. Phakic anterior chamber lenses for the correction of myopia: a 7 year cumulative analysis of complications in 263 cases. Ophthalmology. 1999. 106:458–466.22. Zaldivar R, Davidorff JM, Oscherow S. Posterior chamber phakic intraocular lens for myopia of -8 to -19 diopters. J Refract Surg. 1998. 14:294–305.23. Baikoff G, Arne JL, Bokobza Y, et al. Angle-fixated anterior chamber phakic intraocular lens for myopia of -7 to -19 diopters. J Refract Surg. 1998. 14:282–293.24. Jean LA, Laurence CL. Phakic posterior chamber lenses for high myopia: Functional and anatomical outcomes. J Cataract Refract Surg. 2000. 26:369–374.25. Lackner B, Pieh S, Schmidinger G, et al. Long-term results of implantation of phakic posterior chamber intraocular lenses. J Cataract Refract Surg. 2004. 30:2269–2276.26. Campos E. Amblyopia. Surv Ophthalmol. 1995. 40:23–39.27. Applegate RA, Howland HC. Magnification and visual acuity in refractive surgery. Arch Ophthalmol. 1993. 111:1335–1342.28. El Mallah MK, Chakravarthy U, Hart PM. Amblyopia: is visual loss permanent? Br J Ophthalmol. 2000. 84:952–956.29. Wick B, Wingard M, Cotter S, Scheiman M. Anisometropic amblyopia: is the patient ever too old to treat? Optom Vis Sci. 1992. 69:866–878.30. Simmers AJ, Gray LS. Improvement of visual function in an adult amblyope. Optom Vis Sci. 1999. 76:82–87.31. Sakatani K, Jabbur NS, O'Brien TP. Improvement in best corrected visual acuity in amblyopic adult eyes after laser in situ keratomileusis. J Cataract Refract Surg. 2004. 30:2517–2521.32. Barequet IS, Wygnanski-Jaffe T, Hirsh A. Laser in situ keratomileusis improves visual acuity in some adult eyes with amblyopia. J Refract Surg. 2004. 20:25–28.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Anterior Chamber Phakic Intraocular lens in Patients with high Myopia
- Clinical Results of Anterior Chamber Phakic Intraocular Lens
- Posterior Chamber Intraocular Lens Implantation in High Myopia
- Result of Central Vault Depending on Lens Diameters in Patients with Implantable Collamer Lens Implantation
- Clinical Results of Femtosecond Laser-assisted Cataract Surgery in Eyes with Posterior Chamber Phakic Intraocular Lens