Korean J Ophthalmol.
2007 Sep;21(3):151-154. 10.3341/kjo.2007.21.3.151.
Dark-room Prone-position Test for Intermittent Angle Closure
- Affiliations
-
- 1Department of Ophthalmology, Seoul National University Bundang Hospital, Seongnam, Korea.
- 2Department of Ophthalmology, Seoul National University College of Medicine, Seoul, Korea. kihopark@snu.ac.kr
- 3Glaucoma Service, Dr. Hong's Clinic, Seoul, Korea.
- KMID: 1099030
- DOI: http://doi.org/10.3341/kjo.2007.21.3.151
Abstract
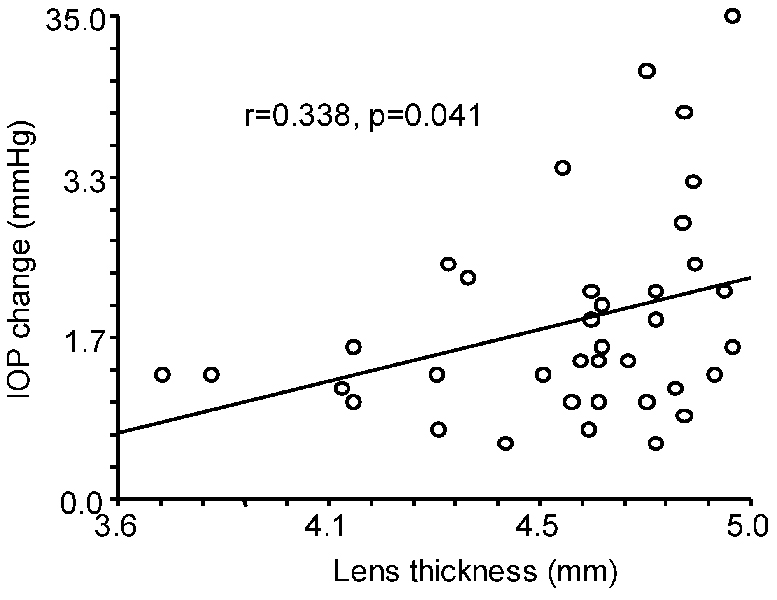
- PURPOSE: To determine the efficacy and safety of the dark-room prone-position test (DRPT) for intermittent angle closure (IAC) and to investigate the correlation between A-scan ultrasound biometric measurements and the results of DRPT. METHODS: Medical records were reviewed of 37 eyes in 24 patients who were diagnosed with IAC and received DRPT. The increase of intraocular pressure (IOP) induced by DRPT and the results from A-scan ultrasound biometric measurements were obtained. An increase in IOP of at least 8 mmHg from baseline was considered a positive result for DRPT. Associations between the increase of IOP induced by DRPT and the parameters of A-scan biometry were tested by linear regression analysis. RESULTS: The DRPT results were positive in 28 eyes of 19 patients. After DRPT, the IOP returned to near-baseline levels within 2 hours in all patients; some patients were treated with anti-glaucoma eye drops. Lens thickness was significantly correlated with the amount of IOP elevation induced by DRPT (r=0.338, p=0.041). CONCLUSIONS: DRPT is a safe and effective test in patients with IAC. DRPT can be used effectively to make a concrete diagnosis of IAC. Lens thickness appears to be associated with a positive response to DRPT.
MeSH Terms
Figure
Reference
-
1. Ritch R, Lowe RF. Ritch R, Shields MB, Krupin T, editors. Angle-closure glaucoma: clinical types. The glaucomas. 1996. 2nd ed. Missouri: Mosby;821–823.2. Berger BB. Foveal photocoagulation from laser iridotomy. Ophthalmology. 1984. 91:1029–1033.3. Bongard B, Pederson JE. Retinal burns from experimental laser iridotomy. Ophthalmic Surg. 1985. 16:42–44.4. Zabel RW, MacDonald IM, Mintsioulis G. Corneal endothelial decompensation after argon laser iridotomy. Can J Ophthalmol. 1991. 26:367–373.5. Small KM, Maslin KF. Malignant glaucoma following laser iridotomy. Aust N Z J Ophthalmol. 1995. 23:339–341.6. Hyams SW, Friedman Z, Neumann E. Elevated intraocular pressure in the prone position. A new provocative test for angle-closure glaucoma. Am J Ophthalmol. 1968. 66:661–672.7. Harris LS, Galin MA. Prone provocative testing for narrow angle glaucoma. Arch Ophthalmol. 1972. 87:493–496.8. Wilensky JT, Kaufman PL, Frohlichstein D, et al. Follow-up of angle-closure glaucoma suspects. Am J Ophthalmol. 1993. 115:338–346.9. Hong C, Park KH, Hyung SM, et al. Evaluation of pupillary block component in angle-closure glaucoma. Jpn J Ophthalmol. 1996. 40:239–243.10. Kondo T, Miyazawa D, Unigame K, Kurimoto Y. Ultrasound biomicroscopic findings in humans with shallow anterior chamber and increased intraocular pressure after the prone provocation test. Am J Ophthalmol. 1997. 124:632–640.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Dark Room Prone-position Test in Primary Angle-Closure Glaucoma
- Argon Laser Peripheral Iridoplasty in Angle-Closure Glaucoma
- The Supine and Prone Position for Computed Tomographic Myelography(CTM) of the Lumbar Spine: Change of Gantry Angle
- The changes of endotracheal tube cuff pressure by the position changes from supine to prone and the flexion and extension of head
- Sedation for magnetic resonance imaging in the prone position - A report of four cases -