Korean J Radiol.
2011 Apr;12(2):187-195. 10.3348/kjr.2011.12.2.187.
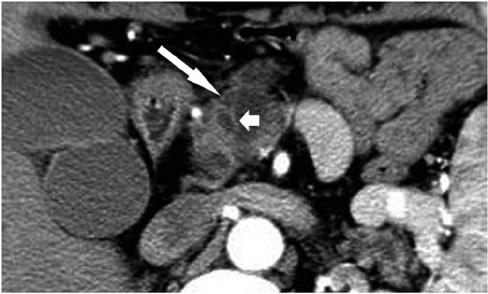
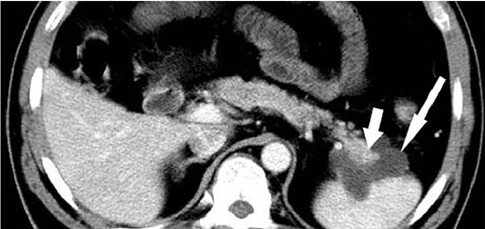
Differentiating Pancreatic Ductal Adenocarcinoma from Pancreatic Serous Cystadenoma, Mucinous Cystadenoma, and a Pseudocyst with Detailed Analysis of Cystic Features on CT Scans: a Preliminary Study
- Affiliations
-
- 1Department of Radiology, Rui Jin Hospital Shanghai Jiao Tong University School of Medicine, No. 197, Rui Jin Er Road, Shanghai 200025, China. keminchen0307@yahoo.com.cn
- 2Department of Pathology, Rui Jin Hospital Shanghai Jiao Tong University School of Medicine, No. 197, Rui Jin Er Road, Shanghai 200025, China.
- KMID: 1088563
- DOI: http://doi.org/10.3348/kjr.2011.12.2.187
Abstract
OBJECTIVE
To determine whether or not detailed cystic feature analysis on CT scans can assist in the differential diagnosis of pancreatic ductal adenocarcinoma (PDAC) from serous cystadenoma (SCN), mucinous cystadenoma (MCN), and a pseudocyst.
MATERIALS AND METHODS
This study received Institutional Review Board approval and informed patient consent was waived. Electronic radiology and pathology databases were searched to identify patients with PDAC (n = 19), SCN (n = 26), MCN (n = 20) and a pseudocyst (n = 23) who underwent pancreatic CT imaging. The number, size, location, and contents of cysts, and the contour of the lesions were reviewed, in addition to the wall thickness, enhancement patterns, and other signs of pancreatic and peripancreatic involvement. Diagnosis was based on lesion resection (n = 82) or on a combination of cytological findings, biochemical markers, and tumor markers (n = 6). Fisher's exact test was used to analyze the results.
RESULTS
A combination of the CT findings including irregular contour, multiple cysts, mural nodes, and localized thickening, had a relatively high sensitivity (74%) and specificity (75%) for differentiating PDAC from SCN, MCN, and pseudocysts (p < 0.05). Other CT findings such as location, greatest dimension, or the presence of calcification were not significantly different.
CONCLUSION
The CT findings for PDAC are non-specific, but perhaps helpful for differentiation. PDAC should be included in the general differential diagnosis of pancreatic cystic neoplasms.
Keyword
MeSH Terms
-
Adenocarcinoma/pathology/*radiography
Adolescent
Adult
Aged
Cystadenocarcinoma, Serous/pathology/*radiography
Cystadenoma, Mucinous/pathology/*radiography
Diagnosis, Differential
Female
Humans
Immunohistochemistry
Male
Middle Aged
Pancreatic Neoplasms/pathology/*radiography
Retrospective Studies
Sensitivity and Specificity
*Tomography, X-Ray Computed
Tumor Markers, Biological/analysis
Figure
Reference
-
1. Brugge WR, Lauwers GY, Sahani D, Fernandez-del Castillo C, Warshaw AL. Cystic neoplasms of the pancreas. N Engl J Med. 2004. 351:1218–1226.2. Kalb B, Sarmiento JM, Kooby DA, Adsay NV, Martin DR. MR imaging of cystic lesions of the pancreas. Radiographics. 2009. 29:1749–1765.3. Lee LY, Hsu HL, Chen HM, Hsueh C. Ductal adenocarcinoma of the pancreas with huge cystic degeneration: a lesion to be distinguished from pseudocyst and mucinous cystadenocarcinoma. Int J Surg Pathol. 2003. 11:235–239.4. Dennis JW, Aranha GV, Greenlee HB, Hoffman JP, Prinz RA. Carcinoma masquerading as a pancreatic pseudocyst on ultrasound. Am Surg. 1984. 50:334–339.5. Ji Y, Lou WH, Jin DY, Kuang TT, Zeng MS, Tan YS, et al. A series of 64 cases of pancreatic cystic neoplasia from an institutional study of China. World J Gastroenterol. 2006. 12:7380–7387.6. Kosmahl M, Pauser U, Anlauf M, Kloppel G. Pancreatic ductal adenocarcinomas with cystic features: neither rare nor uniform. Mod Pathol. 2005. 18:1157–1164.7. Sahani DV, Kadavigere R, Saokar A, Fernandez-del Castillo C, Brugge WR, Hahn PF. Cystic pancreatic lesions: a simple imaging-based classification system for guiding management. Radiographics. 2005. 25:1471–1484.8. Yoon SE, Byun JH, Kim KA, Kim HJ, Lee SS, Jang SJ, et al. Pancreatic ductal adenocarcinoma with intratumoral cystic lesions on MRI: correlation with histopathological findings. Br J Radiol. 2010. 83:318–326.9. Compagno J, Oertel JE. Mucinous cystic neoplasms of the pancreas with overt and latent malignancy (cystadenocarcinoma and cystadenoma). A clinicopathologic study of 41 cases. Am J Clin Pathol. 1978. 69:573–580.10. Buetow PC, Rao P, Thompson LD. From the Archives of the AFIP. Mucinous cystic neoplasms of the pancreas: radiologic-pathologic correlation. Radiographics. 1998. 18:433–449.11. Mathieu D, Guigui B, Valette PJ, Dao TH, Bruneton JN, Bruel JM, et al. Pancreatic cystic neoplasms. Radiol Clin North Am. 1989. 27:163–176.12. Cohen-Scali F, Vilgrain V, Brancatelli G, Hammel P, Vullierme MP, Sauvanet A, et al. Discrimination of unilocular macrocystic serous cystadenoma from pancreatic pseudocyst and mucinous cystadenoma with CT: initial observations. Radiology. 2003. 228:727–733.13. Choi BS, Kim TK, Kim AY, Kim KW, Park SW, Kim PN, et al. Differential diagnosis of benign and malignant intraductal papillary mucinous tumors of the pancreas: MR cholangiopancreatography and MR angiography. Korean J Radiol. 2003. 4:157–162.14. Kosmahl M, Pauser U, Peters K, Sipos B, Luttges J, Kremer B, et al. Cystic neoplasms of the pancreas and tumor-like lesions with cystic features: a review of 418 cases and a classification proposal. Virchows Arch. 2004. 445:168–178.15. Martin DR, Semelka RC. MR imaging of pancreatic masses. Magn Reson Imaging Clin N Am. 2000. 8:787–812.16. Sahani DV, Kadavigere R, Blake M, Fernandez-Del Castillo C, Lauwers GY, Hahn PF. Intraductal papillary mucinous neoplasm of pancreas: multi-detector row CT with 2D curved reformations--correlation with MRCP. Radiology. 2006. 238:560–569.17. Kimura W, Sata N, Nakayama H, Muto T, Matsuhashi N, Sugano K, et al. Pancreatic carcinoma accompanied by pseudocyst: report of two cases. J Gastroenterol. 1994. 29:786–791.18. Itai Y, Moss AA, Ohtomo K. Computed tomography of cystadenoma and cystadenocarcinoma of the pancreas. Radiology. 1982. 145:419–425.19. Sheehan MK, Beck K, Pickleman J, Aranha GV. Spectrum of cystic neoplasms of the pancreas and their surgical management. Arch Surg. 2003. 138:657–660. discussion 660-662.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Pancreatic Serous Cystadenoma Associated with Papillary Thyroid Cancer
- A Case of Serous Cystadenoma of the Pancreas Communicating with the Pancreatic Duct
- Pancreatic Mucinous Cystadenoma Misdiagnosed as Pancreatic Pseudocyst and Managed by Internal Drainage
- Pancreatic serous cystadenoma mimicking pseudocyst
- A Case of Mucinous Cystadenoma of the Pancreas