Yonsei Med J.
2010 May;51(3):432-437. 10.3349/ymj.2010.51.3.432.
The Urologist's View of Male Overactive Bladder: Discrepancy between Reality and Belief in Practical Setting
- Affiliations
-
- 1Department of Urology, Yonsei University College of Medicine, Seoul, Korea. chung646@yuhs.ac
- 2Department of Urology, The Catholic University of Korea College of Medicine, Seoul, Korea.
- 3Department of Urology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 4Department of Urology, Korea University College of Medicine, Seoul, Korea.
- 5Department of Urology, Keimyung University School of Medicine, Daegu, Korea.
- 6Department of Urology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 7Department of Urology, Chonbuk National University Medical School, Jeonju, Korea.
- KMID: 1074997
- DOI: http://doi.org/10.3349/ymj.2010.51.3.432
Abstract
- PURPOSE
In order to gain insight into the physicians' awareness of and attitude towards management of overactive bladder (OAB) in males, we performed a nationwide survey of the current strategies that urologists use to diagnose and manage OAB in male patients.
MATERIALS AND METHODS
A probability sample was taken from the Korean Urological Association Registry of Physicians, and a random sample of 289 Korean urologists were mailed a structured questionnaire that explored how they manage benign prostatic hyperplasia (BPH).
RESULTS
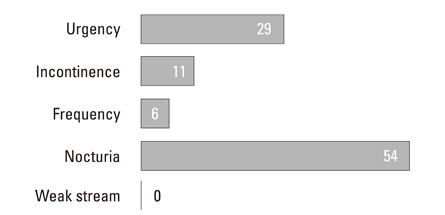
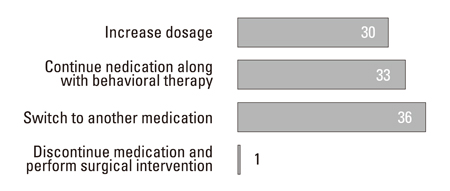
A total of 185 completed questionnaires were returned. The consent rate in the survey was 64.5%. Eighty-one (44%) urologists believed that of all males with lower urinary tract symptoms (LUTS), 20% or more had OAB and 72 (39%) believed that 10-20% had OAB. Half of the urologists surveyed believed that the most bothersome symptom in male OAB patients was nocturia. Seventy-three percent of respondents reported that they prescribed alpha blockers with anticholinergics for first line management, while 19% of urologists prescribed alpha blocker monotherapy but not anticholinergics for OAB patients. Though acute urinary retention (AUR) was considered the anticholinergic adverse event of most concern, the most frequently observed adverse event was dry mouth (95%).
CONCLUSION
The present study provides insights into urologist views of male OAB. There is a discrepancy between the awareness of urologists and actual patterns of diagnosis and treatment of male OAB. This finding indicates the need to develop further practical guidelines based on solid clinical data.
Keyword
MeSH Terms
-
Adrenergic alpha-Antagonists/therapeutic use
Cholinergic Antagonists/therapeutic use
*Health Knowledge, Attitudes, Practice
Humans
Male
Physician's Practice Patterns
Physicians/*psychology
Prostatic Hyperplasia/diagnosis/drug therapy/pathology
Questionnaires
Urinary Bladder Neck Obstruction/diagnosis/drug therapy/pathology
Urinary Bladder, Overactive/*diagnosis/drug therapy/pathology
Urinary Retention/diagnosis/drug therapy/pathology
*Urology
Figure
Cited by 1 articles
Reference
-
1. Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn. 2002. 21:167–178.
Article2. Irwin DE, Milsom I, Hunskaar S, Reilly K, Kopp Z, Herschorn S, et al. Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. Eur Urol. 2006. 50:1306–1314.
Article3. Chapple CR, Roehrborn CG. A shifted paradigm for the further understanding, evaluation, and treatment of lower urinary tract symptoms in men: focus on the bladder. Eur Urol. 2006. 49:651–658.
Article4. Abdel-Aziz KF, Lemack GE. Overactive bladder in the male patient: bladder, outlet, or both? Curr Urol Rep. 2002. 3:445–451.
Article5. de Nunzio C, Franco G, Rocchegiani A, Iori F, Leonardo C, Laurenti C. The evolution of detrusor overactivity after watchful waiting, medical therapy and surgery in patients with bladder outlet obstruction. J Urol. 2003. 169:535–539.
Article6. Goepel M, Hoffmann JA, Piro M, Rübben H, Michel MC. Prevalence and physician awareness of symptoms of urinary bladder dysfunction. Eur Urol. 2002. 41:234–239.
Article7. Milsom I, Abrams P, Cardozo L, Roberts RG, Thüroff J, Wein AJ. How widespread are the symptoms of an overactive bladder and how are they managed? A population-based prevalence study. BJU Int. 2001. 87:760–766.8. Djavan B, Nickel JC, de la Rosette J, Abrams P. The urologist view of BPH progression: results of an international survey. Eur Urol. 2002. 41:490–496.
Article9. Moorthy P, Lapitan MC, Quek PL, Lim PH. Prevalence of overactive bladder in Asian men: an epidemiological survey. BJU Int. 2004. 93:528–531.10. Knutson T, Edlund C, Fall M, Dahlstrand C. BPH with coexisting overactive bladder dysfunction--an everyday urological dilemma. Neurourol Urodyn. 2001. 20:237–247.11. Ameda K, Sullivan MP, Bae RJ, Yalla SV. Urodynamic characterization of nonobstructive voiding dysfunction in symptomatic elderly men. J Urol. 1999. 162:142–146.
Article12. Johansson C, Hellström L, Ekelund P, Milsom I. Urinary incontinence: a minor risk factor for hip fractures in elderly women. Maturitas. 1996. 25:21–28.
Article13. Eckhardt MD, van Venrooij GE, van Melick HH, Boon TA. Prevalence and bothersomeness of lower urinary tract symptoms in benign prostatic hyperplasia and their impact on well-being. J Urol. 2001. 166:563–568.
Article14. Choo MS, Ku JH, Park CH, Lee YS, Lee KS, Lee JG, et al. Prevalence of nocturia in a Korean population aged 40 to 89 years. Neurourol Urodyn. 2008. 27:60–64.
Article15. Abrams P, Kaplan S, De Koning Gans HJ, Millard R. Safety and tolerability of tolterodine for the treatment of overactive bladder in men with bladder outlet obstruction. J Urol. 2006. 175:999–1004.
Article16. Kaplan SA, Walmsley K, Te AE. Tolterodine extended release attenuates lower urinary tract symptoms in men with benign prostatic hyperplasia. J Urol. 2005. 174:2273–2275.
Article17. Barry MJ, Cockett AT, Holtgrewe HL, McConnell JD, Sihelnik SA, Winfield HN. Relationship of symptoms of prostatism to commonly used physiological and anatomical measures of the severity of benign prostatic hyperplasia. J Urol. 1993. 150:351–358.
Article18. Bowling A. Mode of questionnaire administration can have serious effects on data quality. J Public Health (Oxf). 2005. 27:281–291.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Erratum to "The Urologist's View of Male Overactive Bladder: Discrepancy between Reality and Belief in Practical Setting" by Lee SH, et al. (Yonsei Med J 2010;51:432-437)
- Overactive Bladder
- The Analysis of Persistent Overactive Bladder Syndrome after Sling Surgery in Female Stress Urinary Incontinence
- Overactive Bladder
- New Frontiers in the Treatment of Overactive Bladder