Korean J Ophthalmol.
2011 Dec;25(6):455-458. 10.3341/kjo.2011.25.6.455.
Optic Disc Pit with Peripapillary Retinoschisis Presenting as a Localized Retinal Nerve Fiber Layer Defect
- Affiliations
-
- 1Department of Ophthalmology, Hanyang University College of Medicine, Seoul, Korea. KBUhm@hanyang.ac.kr
- KMID: 1031196
- DOI: http://doi.org/10.3341/kjo.2011.25.6.455
Abstract
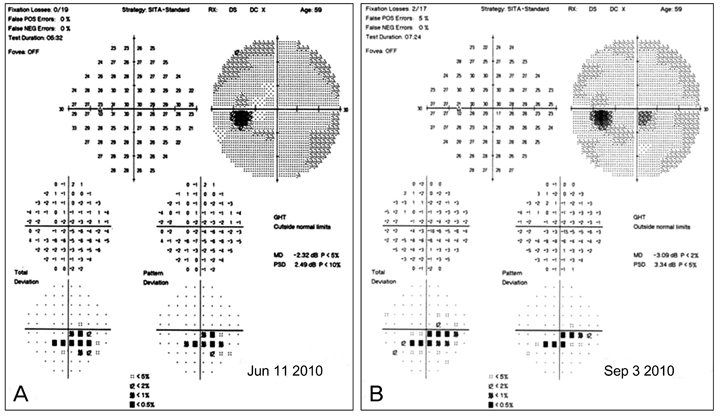
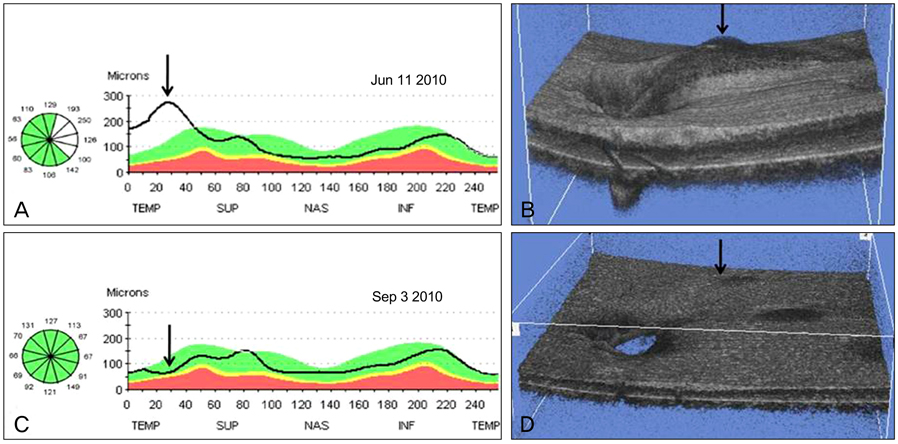
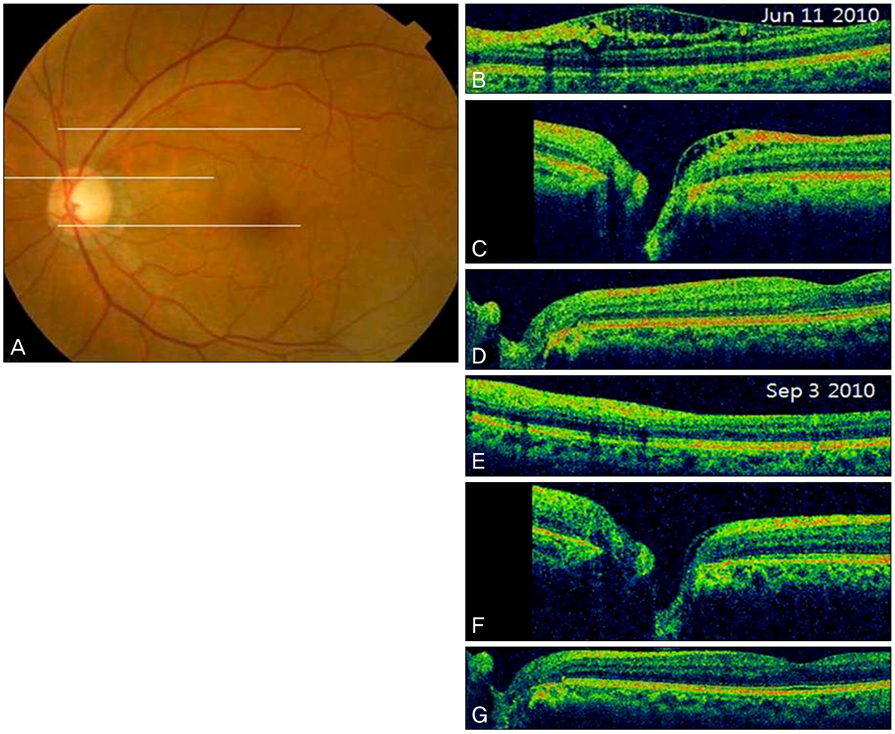
- A 59-year-old woman was referred to our clinic for a glaucoma evaluation. The visual acuity and intraocular pressure were normal in both eyes. However, red-free fundus photography in the left eye showed a superotemporal wedge-shaped retinal nerve fiber layer defect, and visual field testing showed a corresponding partial arcuate scotoma. In an optical coherence tomography examination, the macula was flat, but an arcuate-shaped peripapillary retinoschisis was found. Further, the retinoschisis seemed to be connected with a superotemporal optic pit shown in a disc photograph. After 3 months of a topical prostaglandin analogue medication, the intraocular pressure in the retinoschisis eye was lowered from 14 to 10 mmHg and the peripapillary retinoschisis was almost resolved. We report a rare case of an optic disc pit with peripapillary retinoschisis presenting as a localized retinal nerve fiber layer defect.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Peripapillary Retinoschisis in Non-Glaucomatous Eyes
Sun Young Jin, Mi Ryoung Song, Min Kyung Kim, Young Hoon Hwang
J Korean Ophthalmol Soc. 2015;56(1):80-85. doi: 10.3341/jkos.2015.56.1.80.
Reference
-
1. Kranenburg EW. Crater-like holes in the optic disc and central serous retinopathy. Arch Ophthalmol. 1960. 64:912–924.2. Brown GC, Shields JA, Goldberg RE. Congenital pits of the optic nerve head. II. Clinical studies in humans. Ophthalmology. 1980. 87:51–65.3. Krivoy D, Gentile R, Liebmann JM, et al. Imaging congenital optic disc pits and associated maculopathy using optical coherence tomography. Arch Ophthalmol. 1996. 114:165–170.4. Sobol WM, Blodi CF, Folk JC, Weingeist TA. Long-term visual outcome in patients with optic nerve pit and serous retinal detachment of the macula. Ophthalmology. 1990. 97:1539–1542.5. Ryan SJ. Retina. 2006. 2:4th ed. Philadelphia: Mosby Elsevier;1883.6. Brodsky MC. Congenital optic disk anomalies. Surv Ophthalmol. 1994. 39:89–112.7. Lincoff H, Lopez R, Kreissig I, et al. Retinoschisis associated with optic nerve pits. Arch Ophthalmol. 1988. 106:61–67.8. Lincoff H, Schiff W, Krivoy D, Ritch R. Optic coherence tomography of optic disk pit maculopathy. Am J Ophthalmol. 1996. 122:264–266.9. Radius RL, Maumenee AE, Green WR. Pit-like changes of the optic nerve head in open-angle glaucoma. Br J Ophthalmol. 1978. 62:389–393.10. Javitt JC, Spaeth GL, Katz LJ, et al. Acquired pits of the optic nerve. Increased prevalence in patients with low-tension glaucoma. Ophthalmology. 1990. 97:1038–1043.11. Nduaguba C, Ugurlu S, Caprioli J. Acquired pits of the optic nerve in glaucoma: prevalence and associated visual field loss. Acta Ophthalmol Scand. 1998. 76:273–277.12. Ugurlu S, Weitzman M, Nduaguba C, Caprioli J. Acquired pit of the optic nerve: a risk factor for progression of glaucoma. Am J Ophthalmol. 1998. 125:457–464.13. Healey PR, Mitchell P. The prevalence of optic disc pits and their relationship to glaucoma. J Glaucoma. 2008. 17:11–14.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Retinal Herniation through Peripapillary Pit Resulting in Retinal Nerve Fiber Layer Defect
- A Comparison of Retinal Thickness Changes According to Initial Optic Disc Edema in Optic Neuritis Patients
- A Case of Optic Disc Pit
- Reproducibility of Retinal Nerve Fiber Layer Thickness Evaluation by Nerve Fiber Analyzer
- Two Cases of Topless Optic Disc Syndrome