Korean J Ophthalmol.
2011 Dec;25(6):447-450. 10.3341/kjo.2011.25.6.447.
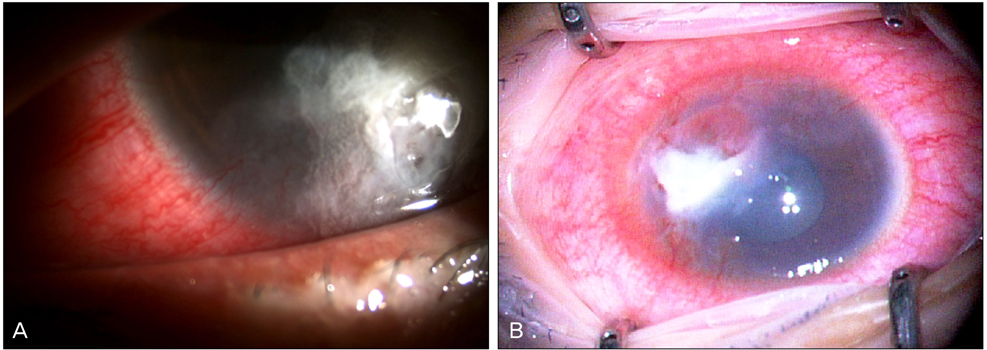
Superimposed Fungal Ulcer after Fibrin Glue Sealant in Infectious Corneal Ulcer
- Affiliations
-
- 1Department of Ophthalmology and Visual Science, Seoul St. Mary's Hospital, The Catholic University of Korea College of Medicine, Seoul, Korea. mskim@catholic.ac.kr
- KMID: 1031194
- DOI: http://doi.org/10.3341/kjo.2011.25.6.447
Abstract
- A healthy 27-year-old woman with a corneal ulcer underwent fibrin gluing with a bandage contact lens twice, due to an impending perforation. The ulcer lesion slowly progressed, unresponsive to topical antibiotics and amphotericin B. We removed the gluing patch and performed a corneal or scraping or biopsy with multiple amniotic membrane grafts to seal the thinned or perforated cornea. Three days after the surgery, the corneal cultures grew Fusarium, as well as Enterococcus faecalis. Three weeks after surgery, the outermost layer of amniotic membranes, serving as a temporary patch, was removed. The anterior chamber was clear without cells. The signs of infection clinically and symptomatically cleared up four weeks later. Two months after surgery, the lesion became enhanced by amniotic membranes. The use of fibrin glue in infectious keratitis should be avoided, because it not only masks the underlying lesion, but it also interferes with drug penetration into the underlying lesion.
MeSH Terms
Figure
Reference
-
1. Refojo MF, Dohlman CH, Ahmad B, et al. Evaluation of adhesives for corneal surgery. Arch Ophthalmol. 1968. 80:645–656.2. Webster RG Jr, Slansky HH, Refojo MF, et al. The use of adhesive for the closure of corneal perforations. Report of two cases. Arch Ophthalmol. 1968. 80:705–709.3. Lagoutte FM, Gauthier L, Comte PR. A fibrin sealant for perforated and preperforated corneal ulcers. Br J Ophthalmol. 1989. 73:757–761.4. Duchesne B, Tahi H, Galand A. Use of human fibrin glue and amniotic membrane transplant in corneal perforation. Cornea. 2001. 20:230–232.5. Sumich PM, Cook SD, Tole DM. Fibrin tissue-filler glue for persistent epithelial defects. Clin Experiment Ophthalmol. 2003. 31:267–269.6. Watts MT, Collin R. The use of fibrin glue in mucous membrane grafting of the fornix. Ophthalmic Surg. 1992. 23:689–690.7. Grewing R, Mester U. Fibrin sealant in the management of complicated hypotony after trabeculectomy. Ophthalmic Surg Lasers. 1997. 28:124–127.8. Kaufman HE, Insler MS, Ibrahim-Elzembely HA, Kaufman SC. Human fibrin tissue adhesive for sutureless lamellar keratoplasty and scleral patch adhesion: a pilot study. Ophthalmology. 2003. 110:2168–2172.9. Vote BJ, Elder MJ. Cyanoacrylate glue for corneal perforations: a description of a surgical technique and a review of the literature. Clin Experiment Ophthalmol. 2000. 28:437–442.10. Markowitz GD, Orlin SE, Frayer WC, et al. Corneal endothelial polymerization of histoacryl adhesive: a report of a new intraocular complication. Ophthalmic Surg. 1995. 26:256–258.11. Hirst LW, De Juan E Jr. Sodium hyaluronate and tissue adhesive in treating corneal perforations. Ophthalmology. 1982. 89:1250–1253.12. Hyndiuk RA, Hull DS, Kinyoun JL. Free tissue patch and cyanoacrylate in corneal perforations. Ophthalmic Surg. 1974. 5:50–55.13. Leahey AB, Gottsch JD, Stark WJ. Clinical experience with N-butyl cyanoacrylate (Nexacryl) tissue adhesive. Ophthalmology. 1993. 100:173–180.14. Weiss JL, Williams P, Lindstrom RL, Doughman DJ. The use of tissue adhesive in corneal perforations. Ophthalmology. 1983. 90:610–615.15. Hirst LW, Smiddy WE, Stark WJ. Corneal perforations. Changing methods of treatment, 1960-1980. Ophthalmology. 1982. 89:630–635.16. Fogle JA, Kenyon KR, Foster CS. Tissue adhesive arrests stromal melting in the human cornea. Am J Ophthalmol. 1980. 89:795–802.17. Cavanaugh TB, Gottsch JD. Infectious keratitis and cyanoacrylate adhesive. Am J Ophthalmol. 1991. 111:466–472.18. Naruse S, Mori K, Kinoshita S. A new technique for removing the inner wall of Schlemm's canal using cyanoacrylate. Acta Ophthalmol Scand. 2003. 81:151–154.19. Sharma A, Kaur R, Kumar S, et al. Fibrin glue versus N-butyl-2-cyanoacrylate in corneal perforations. Ophthalmology. 2003. 110:291–298.20. Cho BJ. A case of corneal ulcer caused by combined infection of stenotrophomonas maltophilia and aspergillus fumigatus. J Korean Ophthalmol Soc. 2000. 41:1242–1246.21. You IC, Lee SH, Park YG, Yoon KC. Clinical aspect and prognosis of stenotrophomonas (xanthomonas) maltophilia keratitis. J Korean Ophthalmol Soc. 2007. 48:889–897.22. Chan SM, Boisjoly H. Advances in the use of adhesives in ophthalmology. Curr Opin Ophthalmol. 2004. 15:305–310.23. Cheng H, Fraidakis M, Blomback B, et al. Characterization of a fibrin glue-GDNF slow-release preparation. Cell Transplant. 1998. 7:53–61.24. Van Quill KR, Dioguardi PK, Tong CT, et al. Subconjunctival carboplatin in fibrin sealant in the treatment of transgenic murine retinoblastoma. Ophthalmology. 2005. 112:1151–1158.25. Marone P, Monzillo V, Segu C, Antoniazzi E. Antibiotic-impregnated fibrin glue in ocular surgery: in vitro antibacterial activity. Ophthalmologica. 1999. 213:12–15.26. Anitua E, Andia I, Ardanza B, et al. Autologous platelets as a source of proteins for healing and tissue regeneration. Thromb Haemost. 2004. 91:4–15.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Moxifloxacin Mixed Augmented Amniotic Membrane Transplantation for Perforating Infectious Keratitis
- A Clinical Study on Infectious Corneal Ulcer
- Human Amniotic Membrane Transplantation for Treatment of Fungal Ulcer
- Comparison of Hemostatic Effect of Endoscopic Injection with Fibrin Glue (FG) and Hypertonic Saline - epinephrine (HSE) for Peptic Ulcer Bleeding: A prospective randomized trial
- The Plasmin Activity in Tear Film and Chronic Corneal Ulcer