Korean J Lab Med.
2009 Apr;29(2):127-134. 10.3343/kjlm.2009.29.2.127.
Species-Specific Differences in Rhodamine 6G Accumulation of Candida Isolates Detected by Flow Cytometric Analysis
- Affiliations
-
- 1Department of Laboratory Medicine, Chonnam National University Medical School, Gwangju, Korea. shinjh@chonnam.ac.kr
- KMID: 854970
- DOI: http://doi.org/10.3343/kjlm.2009.29.2.127
Abstract
- BACKGROUND
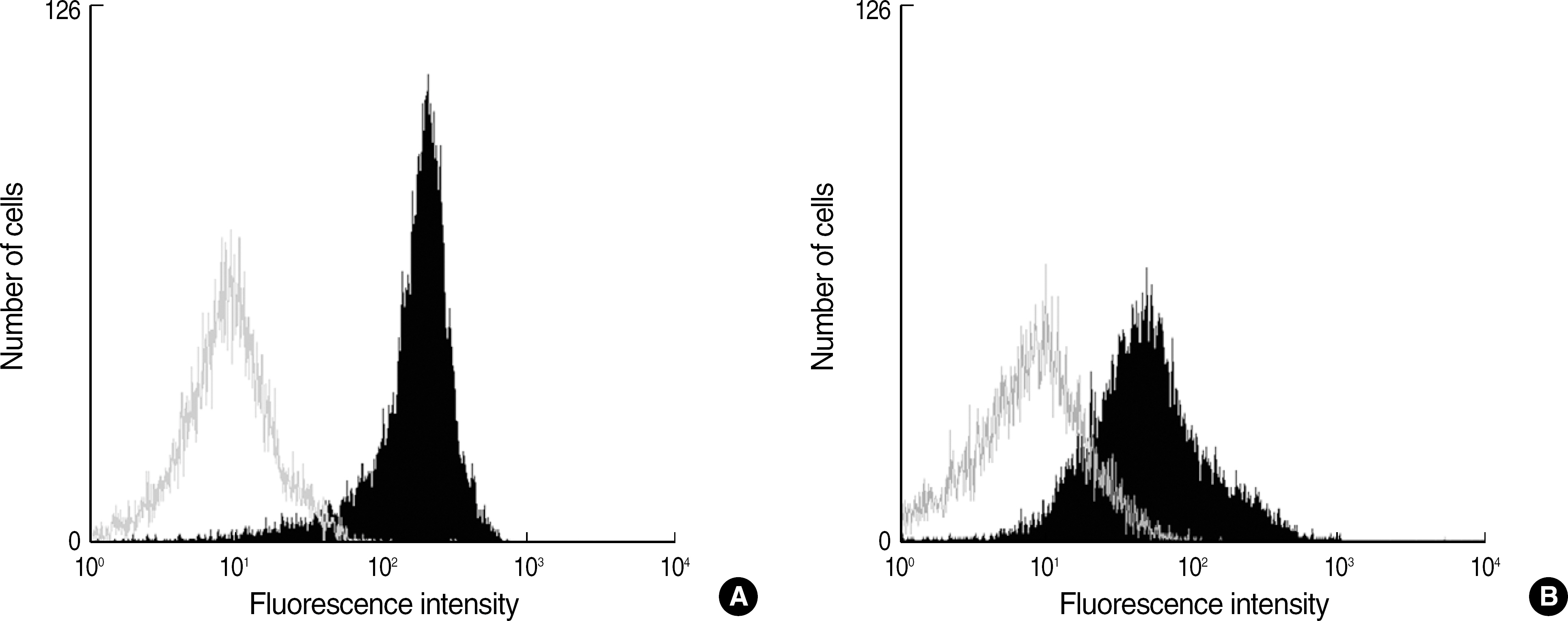
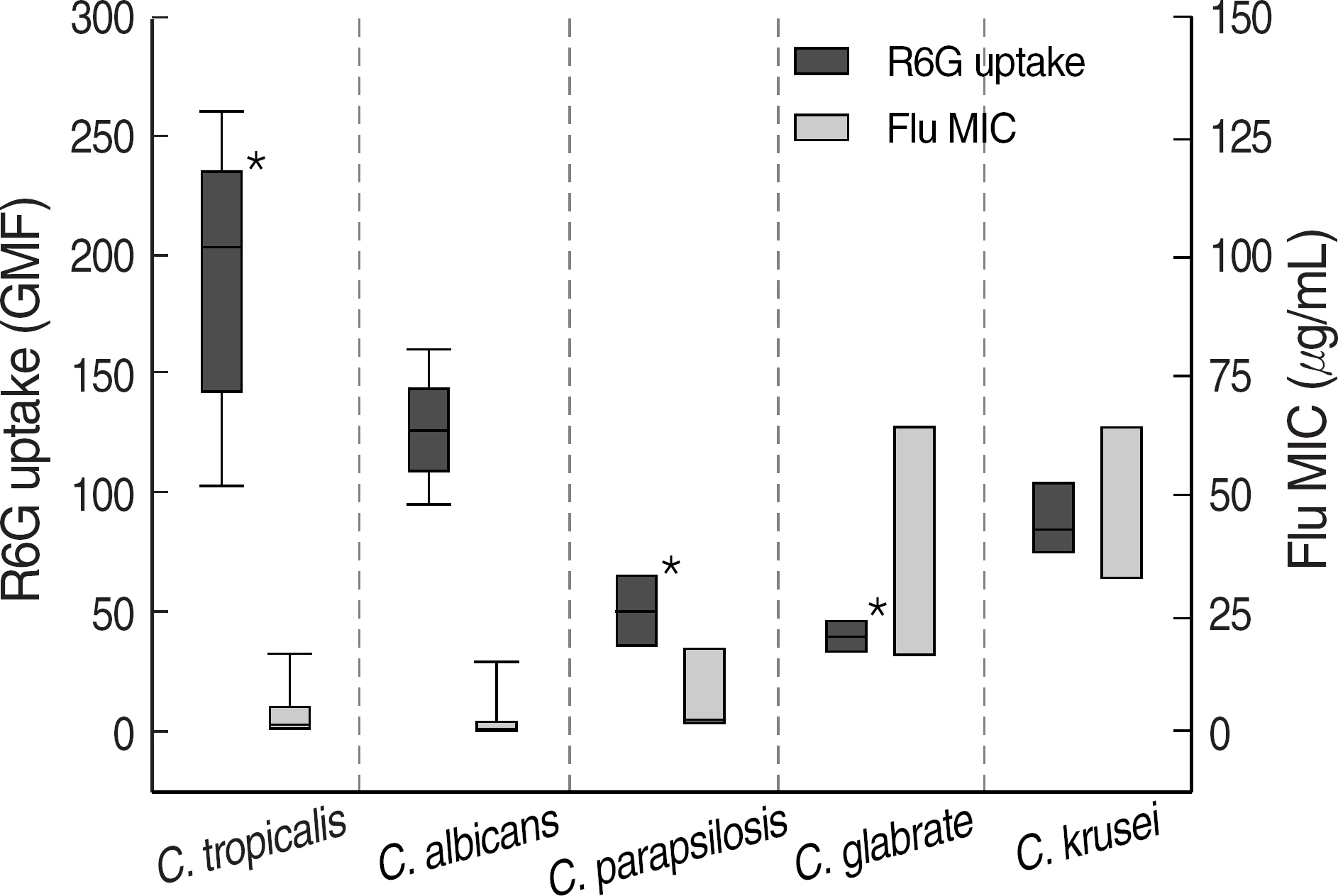
Fluorescent dye Rhodamine 6G (R6G) is a substrate of multidrug resistance pumps and its accumulation is reduced in some azole-resistant Candida isolates with the upregulation of multidrug efflux transporter genes. Despite reports on species-specific differences in azole susceptibility in various Candida species, only a few studies have been reported on the R6G accumulation among clinical isolates of Candida species. In this study, we compared R6G accumulation between six different Candida species. METHODS: The intracellular accumulation of R6G and minimal inhibitory concentrations (MICs) of three triazole agents were investigated in 48 strains of six Candida species (14 C. albicans, 9 C. tropicalis, 8 C. glabrata, 8 C. krusei, 7 C. parapsilosis, and 2 C. haemulonii). R6G accumulation was measured by using flow cytometry and the geometric mean of the fluorescence intensity (GMF) was used to compare the accumulation between the Candida isolates. RESULTS: The GMF values for the C. tropicalis, C. albicans, C. krusei, C. parapsilosis, and C. glabrata isolates were 167.3+/-18.5, 126.9+/-6.6, 88.5+/-18.5, 50.8+/-7.0, and 38.1+/-3.9, respectively. C. glabrata had a significantly lower mean GMF than all the other Candida species (P<0.05). While some Candida strains with trailing growth phenomenon and increased fluconazole MIC did not have a reduced GMF, three Candida strains with increased MICs to all three triazole agents had a reduced GMF. CONCLUSIONS: This study found species-specific differences in R6G accumulation in Candida. In addition, the intracellular R6G accumulation can be used to investigate the drug efflux mechanism in azole-resistant Candida strains.
Keyword
MeSH Terms
Figure
Reference
-
1.Banerjee SN., Emori TG., Culver DH., Gaynes RP., Jarvis WR., Horan T, et al. Secular trends in nosocomial primary bloodstream infections in the United States, 1980-1989. National Nosocomial Infections Surveillance System. Am J Med. 1991. 91:S86–9.2.Sanglard D., Odds FC. Resistance of Candida species to antifungal agents: molecular mechanisms and clinical consequences. Lancet Infect Dis. 2002. 2:73–85.3.Sanglard D., Kuchler K., Ischer F., Pagani JL., Monod M., Bille J. Mechanisms of resistance to azole antifungal agents in Candida albicans isolates from AIDS patients involve specific multidrug transporters. Antimicrob Agents Chemother. 1995. 39:2378–86.4.Sanglard D., Ischer F., Calabrese D., Majcherczyk PA., Bille J. The ATP binding cassette transporter gene CgCDR1 from Candida glabrata is involved in the resistance of clinical isolates to azole antifungal agents. Antimicrob Agents Chemother. 1999. 43:2753–65.5.Barchiesi F., Calabrese D., Sanglard D., Falconi Di Francesco L., Caselli F., Giannini Di, et al. Experimental induction of fluconazole resistance in Candida tropicalis ATCC 750. Antimicrob Agents Chemother. 2000. 44:1578–84.6.Maesaki S., Marichal P., Vanden Bossche H., Sanglard D., Kohno S. Rhodamine 6G efflux for the detection of CDR1-overexpressing azole-resistant Candida albicans strains. J Antimicrob Chemother. 1999. 44:27–31.7.Izumikawa K., Kakeya H., Tsai HF., Grimberg B., Bennett JE. Function of Candida glabrata ABC transporter gene, PDH1. Yeast. 2003. 20:249–61.8.Brun S., Berges T., Poupard P., Vauzelle-Moreau C., Renier G., Chabasse D, et al. Mechanisms of azole resistance in petite mutants of Candida glabrata. Antimicrob Agents Chemother. 2004. 48:1788–96.9.Tsai HF., Krol AA., Sarti KE., Bennett JE. Candida glabrata PDR1, a transcriptional regulator of a pleiotropic drug resistance network, mediates azole resistance in clinical isolates and petite mutants. Antimicrob Agents Chemother. 2006. 50:1384–92.10.Vandeputte P., Larcher G., Berges T., Renier G., Chabasse D., Bouchara JP. Mechanisms of azole resistance in a clinical isolate of Candida tropicalis. Antimicrob Agents Chemother. 2005. 49:4608–15.11.Woo JH., You YK., Chu WS., Park CS. Measurement of staphylococcus aureus phagocytosis by human leukocytes -comparison of flow cytometry with immune microscopy-. Korean J Immunol. 1992. 14:35–40. (우준희, 유용규, 추원석, 박춘식. 백혈구의 포도구균 탐식 측정-유체세포측정법과면역형광현미경측정의비교 -. 대한면역학회지 1992;14: 35-40.).12.Lee W., Kwak Y. Antifungal susceptibility testing of Candida species by flow cytometry. J Korean Med Sci. 1999. 14:21–6.13.Clinical and Laboratory Standards Institute. Reference method for broth dilution antifungal susceptibility testing of yeasts; approved standard-third edition. M27-A2. Wayne, PA: Clinical and Laboratory Standards Institute;2002.14.Yi JY., Shin JH., Lee K., Yong D., Chae MJ., Suh SP, et al. Evaluation of spectrophotometric broth microdilution method to determine the fluconazole MIC of the Candida species. Korean J Lab Med. 2002. 22:253–9. (이지연, 신종희, 이경원, 용동은, 채명종, 서순팔등. Candida 균종의Fluconazole 감수성검사를위한Spectrophotometric Broth Microdilution법의평가. 대한진단검사의학회지 2002;22: 253-9.).15.Sanguinetti M., Posteraro B., Fiori B., Ranno S., Torelli R., Fadda G. Mechanisms of azole resistance in clinical isolates of Candida glabrata collected during a hospital survey of antifungal resistance. Antimicrob Agents Chemother. 2005. 49:668–79.16.Shin JH., Chae MJ., Song JW., Jung SI., Cho D., Kee SJ, et al. Changes in karyotype and azole susceptibility of sequential bloodstream isolates from patients with Candida glabrata candidemia. J Clin Microbiol. 2007. 45:2385–91.17.Sanglard D., Bille J. Current understanding of the modes of action of and resistance mechanisms to conventional and emerging antifungal agents for treatment of Candida infections. Calderone RA, editor. Candida and Candidiasis. Washington: ASM press;2002. p. 349–83.18.Ostrosky-Zeichner L., Rex JH., Pappas PG., Hamill RJ., Larsen RA., Horowitz HW, et al. Antifungal susceptibility survey of 2,000 bloodstream Candida isolates in the United States. Antimicrob Agents Chemother. 2003. 47:3149–54.19.Guinea J., Sanchez-Somolinos M., Cuevas O., Pelaez T., Bouza E. Fluconazole resistance mechanisms in Candida krusei: the contribution of efflux-pumps. Med Mycol. 2006. 44:575–8.20.Yi JY., Shin JH., Lee K., Yong D., Yang SJ., Suh SP, et al. Evaluation of a spectrophotometric broth microdilution method for determining fluconazole susceptibility of Candida albicans: influence of RPMI and RPMI-2% glucose on the selection of endpoint criteria. Korean J Lab Med. 2002. 22:188–95. (이지연, 신종희, 이경원, 용동은, 양성진, 서순팔등. RPMI 배지및RPMI-2% Glucose 배지를이용한 Candida albicans의 fluconazole 감수성검사. 대한진단검사의학회지 2002;22: 188-95.).21.Shin JH., Kee SJ., Shin MG., Kim SH., Shin DH., Lee SK, et al. Biofilm production by isolates of Candida species recovered from nonneutropenic patients: comparison of bloodstream isolates with isolates from other sources. J Clin Microbiol. 2002. 40:1244–8.22.Rodero L., Cuenca-Estrella M., Cordoba S., Cahn P., Davel G., Kaufman S, et al. Transient fungemia caused by an amphotericin B-resistant isolate of Candida haemulonii. J Clin Microbiol. 2002. 40:2266–9.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Antifungal susceptibility testing of Candida species by flow cytometry
- Identification of Candida Species by Analysis of rRNA Spacer Regions
- Identification of Candida Species by Multiplex Polymerase Chain Reaction
- Identification of Candida Species Using CHROMagar Candida in Superficial Cutaneous Candidiasis
- Antifungal Susceptibility Testing with Etest for Candida Species Isolated from Patients with Oral Candidiasis