Endoscopic Ultrasonography-Guided Ethanol Ablation for Small Pancreatic Neuroendocrine Tumors: Results of a Pilot Study
- Affiliations
-
- 1Division of Gastroenterology, Department of Internal Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. dhpark@amc.seoul.kr
- 2Department of Internal Medicine, Dankook University College of Medicine, Cheonan, Korea.
- KMID: 1801208
- DOI: http://doi.org/10.5946/ce.2015.48.2.158
Abstract
- BACKGROUND/AIMS
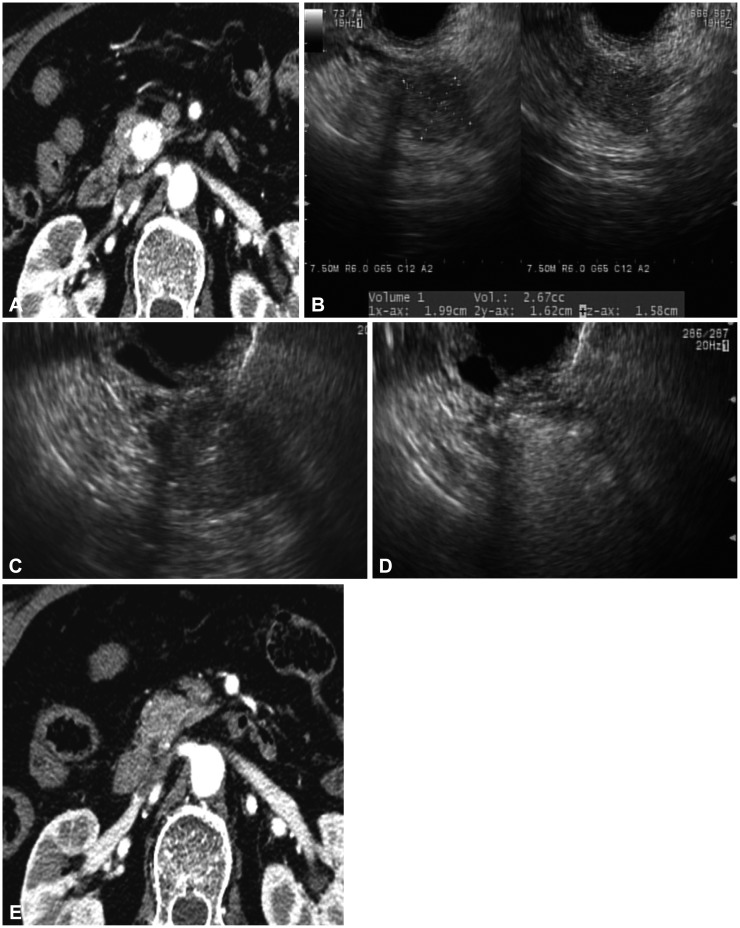
Endoscopic ultrasonography (EUS)-guided ethanol ablation is gaining popularity for the treatment of focal pancreatic lesions. The aim of this study was to evaluate the safety, feasibility, and treatment response after EUS-guided ethanol injection for small pancreatic neuroendocrine tumors (p-NETs).
METHODS
This was a retrospective analysis of a prospectively collected database including 11 consecutive patients with p-NETs who underwent EUS-guided ethanol injection.
RESULTS
EUS-guided ethanol injection was successfully performed in 11 patients with 14 tumors. The final diagnosis was based on histology and clinical signs as follows: 10 non-functioning neuroendocrine tumors and four insulinomas. During follow-up (median, 370 days; range, 152 to 730 days), 10 patients underwent clinical follow-up after treatment, and one patient was excluded because of loss to follow-up. A single treatment session with an injection of 0.5 to 3.8 mL of ethanol resulted in complete responses (CRs) at the 3-month radiologic imaging for seven of 13 tumors (response rate, 53.8%). Multiple treatment sessions performed in three tumors with residual viable enhancing tissue increased the number of tumors with CRs to eight of 13 (response rate, 61.5%). Mild pancreatitis occurred in three of 11 patients.
CONCLUSIONS
EUS-guided ethanol injection appears to be a safe, feasible, and potentially effective method for treating small p-NETs in patients who are poor surgical candidates.
Keyword
MeSH Terms
Figure
Cited by 7 articles
-
Surgical outcomes are hampered after endoscopic ultrasonography-guided ethanol lavage and/or Taxol injection in cystic lesions of the pancreas
Seong-Ryong Kim, Song Cheol Kim, Ki Byung Song, Kwang-Min Park, Dae Wook Hwang, Jae Hoon Lee, Sang Hyun Shin, Bong Jun Kwak, Young-Joo Lee
Ann Hepatobiliary Pancreat Surg. 2021;25(3):342-348. doi: 10.14701/ahbps.2021.25.3.342.Irreversible electroporation for the treatment of pancreatic neuroendocrine tumors
Michail Papamichail, Amir Ali, Michail Pizanias, Praveen Peddu, John Karani, Nigel Heaton
Korean J Hepatobiliary Pancreat Surg. 2016;20(3):116-120. doi: 10.14701/kjhbps.2016.20.3.116.Current Status of Endoscopic Ultrasound Techniques for Pancreatic Neoplasms
Yousuke Nakai, Naminatsu Takahara, Suguru Mizuno, Hirofumi Kogure, Kazuhiko Koike
Clin Endosc. 2019;52(6):527-532. doi: 10.5946/ce.2019.025.Future Perspectives on Endoscopic Ultrasonography-Guided Therapy for Pancreatic Neoplasm
Woo Hyun Paik, Sang Hyub Lee, Sunguk Jang
Clin Endosc. 2018;51(3):229-234. doi: 10.5946/ce.2018.063.Endoscopic Ultrasound-Guided Direct Intervention for Solid Pancreatic Tumors
Jimin Han, Kenneth J. Chang
Clin Endosc. 2017;50(2):126-137. doi: 10.5946/ce.2017.034.Diagnosis of Pancreatic Neuroendocrine Tumors
Dong Wook Lee, Michelle Kang Kim, Ho Gak Kim
Clin Endosc. 2017;50(6):537-545. doi: 10.5946/ce.2017.131.Therapy of Pancreatic Neuroendocrine Tumors: Fine Needle Intervention including Ethanol and Radiofrequency Ablation
Sundeep Lakhtakia
Clin Endosc. 2017;50(6):546-551. doi: 10.5946/ce.2017.167.
Reference
-
1. O'Grady HL, Conlon KC. Pancreatic neuroendocrine tumours. Eur J Surg Oncol. 2008; 34:324–332. PMID: 17967523.2. Modlin IM, Oberg K, Chung DC, et al. Gastroenteropancreatic neuroendocrine tumours. Lancet Oncol. 2008; 9:61–72. PMID: 18177818.
Article3. Cherenfant J, Stocker SJ, Gage MK, et al. Predicting aggressive behavior in nonfunctioning pancreatic neuroendocrine tumors. Surgery. 2013; 154:785–791. PMID: 24074416.
Article4. Oberg K, Eriksson B. Endocrine tumours of the pancreas. Best Pract Res Clin Gastroenterol. 2005; 19:753–781. PMID: 16253899.5. Falconi M, Plockinger U, Kwekkeboom DJ, et al. Well-differentiated pancreatic nonfunctioning tumors/carcinoma. Neuroendocrinology. 2006; 84:196–211. PMID: 17312380.
Article6. Bettini R, Partelli S, Boninsegna L, et al. Tumor size correlates with malignancy in nonfunctioning pancreatic endocrine tumor. Surgery. 2011; 150:75–82. PMID: 21683859.
Article7. Oh HC, Seo DW, Song TJ, et al. Endoscopic ultrasonography-guided ethanol lavage with paclitaxel injection treats patients with pancreatic cysts. Gastroenterology. 2011; 140:172–179. PMID: 20950614.
Article8. Larssen TB, Rosendahl K, Horn A, Jensen DK, Rørvik J. Single-session alcohol sclerotherapy in symptomatic benign hepatic cysts performed with a time of exposure to alcohol of 10 min: initial results. Eur Radiol. 2003; 13:2627–2632. PMID: 12955449.9. Aslanian H, Salem RR, Marginean C, Robert M, Lee JH, Topazian M. EUS-guided ethanol injection of normal porcine pancreas: a pilot study. Gastrointest Endosc. 2005; 62:723–727. PMID: 16246687.
Article10. Deprez PH, Claessens A, Borbath I, Gigot JF, Maiter D. Successful endoscopic ultrasound-guided ethanol ablation of a sporadic insulinoma. Acta Gastroenterol Belg. 2008; 71:333–337. PMID: 19198582.11. Jürgensen C, Schuppan D, Neser F, Ernstberger J, Junghans U, StÖlzel U. EUS-guided alcohol ablation of an insulinoma. Gastrointest Endosc. 2006; 63:1059–1062. PMID: 16733126.
Article12. Levy MJ, Thompson GB, Topazian MD, Callstrom MR, Grant CS, Vella A. US-guided ethanol ablation of insulinomas: a new treatment option. Gastrointest Endosc. 2012; 75:200–206. PMID: 22078104.
Article13. Vleggaar FP, Bij de, Valk GD, Leguit RJ, Siersema PD. Endoscopic ultrasound-guided ethanol ablation of a symptomatic sporadic insulinoma. Endoscopy. 2011; 43(Suppl 2 UCTN):E328–E329. PMID: 22020710.
Article14. Zhang WY, Li ZS, Jin ZD. Endoscopic ultrasound-guided ethanol ablation therapy for tumors. World J Gastroenterol. 2013; 19:3397–3403. PMID: 23801831.
Article15. Gelczer RK, Charboneau JW, Hussain S, Brown DL. Complications of percutaneous ethanol ablation. J Ultrasound Med. 1998; 17:531–533. PMID: 9697961.
Article16. Matthes K, Mino-Kenudson M, Sahani DV, Holalkere N, Brugge WR. Concentration-dependent ablation of pancreatic tissue by EUS-guided ethanol injection. Gastrointest Endosc. 2007; 65:272–277. PMID: 17258986.
Article17. Lencioni R, Crocetti L, Cioni D, et al. Single-session percutaneous ethanol ablation of early-stage hepatocellular carcinoma with a multipronged injection needle: results of a pilot clinical study. J Vasc Interv Radiol. 2010; 21:1533–1538. PMID: 20817558.
Article18. Kitano M, Sakamoto H, Kudo M. Endoscopic ultrasound: contrast enhancement. Gastrointest Endosc Clin N Am. 2012; 22:349–358. PMID: 22632956.
Article19. Giday SA, Magno P, Gabrielson KL, et al. The utility of contrast-enhanced endoscopic ultrasound in monitoring ethanol-induced pancreatic tissue ablation: a pilot study in a porcine model. Endoscopy. 2007; 39:525–529. PMID: 17554648.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Therapy of Pancreatic Neuroendocrine Tumors: Fine Needle Intervention including Ethanol and Radiofrequency Ablation
- Endoscopic Ultrasonography-Guided Ethanol Ablation for Small Pancreatic Neuroendocrine Tumors: Results of a Pilot Study
- Endoscopic Ultrasonography-Guided Ethanol Injection for a Pancreatic Neuroendocrine Tumor with Multiple Endocrine Neoplasia Type 1
- Future Perspectives on Endoscopic Ultrasonography-Guided Therapy for Pancreatic Neoplasm
- Endoscopic Ultrasound-Guided Treatment of Pancreatic Cystic and Solid Masses