Ann Pediatr Endocrinol Metab.
2024 Apr;29(2):90-94. 10.6065/apem.2346054.027.
Effectiveness of the triptorelin stimulation test compared with the classic gonadotropin-releasing hormone stimulation test in diagnosing central precocious puberty in girls
- Affiliations
-
- 1Department of Pediatrics, Korea University Ansan Hospital, Ansan, Korea
- 2Department of Pediatrics, Korea University Anam Hospital, Seoul, Korea
- 3Department of Pediatrics, Korea University Guro Hospital, Seoul, Korea
- KMID: 2554679
- DOI: http://doi.org/10.6065/apem.2346054.027
Abstract
- Purpose
The gonadotropin-releasing hormone (GnRH) stimulation test is the gold standard for diagnosing central precocious puberty (CPP). Gonadorelin (Relefact) is used for the test but is not always readily available; triptorelin is used as an alternative. The purpose of this study was to evaluate the diagnostic validity of the triptorelin test compared with the GnRH test in the diagnosis of CPP in girls.
Methods
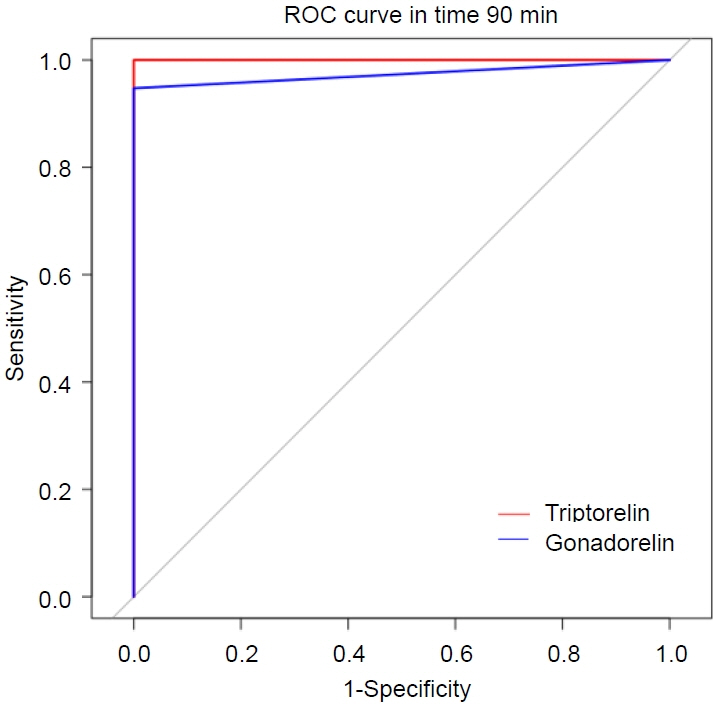
This retrospective study included 100 girls with premature thelarche (PT) who underwent a hypothalamic-pituitary-gonadal axis evaluation. In the overall group, 50 girls were tested with intravenous gonadorelin (Relefact) and 50 girls were tested with subcutaneous triptorelin acetate (Decapeptyl). Luteinizing hormone (LH) and follicle-stimulating hormone levels were measured at baseline and 30, 45, 60, and 90 minutes after gonadorelin injection or 30, 60, 90, and 120 minutes after triptorelin injection.
Results
Clinical characteristics of age, height, weight, body mass index, and bone age were similar between the 2 groups. The highest LH level was reached 60 minutes after stimulation in both groups. Approximately 20% of the gonadorelin group and 24% of the triptorelin group were diagnosed with CPP (P=0.52). Among those diagnosed with CPP, the mean peak LH concentrations were 8.15 mIU/mL and 9.73 mIU/mL in the gonadorelin and triptorelin groups, respectively.
Conclusion
The triptorelin test showed similar trends of LH elevation and diagnostic rate compared with the traditional GnRH test for diagnosing CPP. This suggests that the triptorelin test may be a valid alternative to the GnRH test for differentiating CPP from self-limiting PT. Our study also demonstrated that a triptorelin stimulation test for up to 120 minutes was sufficient to diagnose CPP.
Keyword
Figure
Reference
-
References
1. Berberoğlu M. Precocious puberty and normal variant puberty: definition, etiolog y, diagnosis and current management. J Clin Res Pediatr Endocrinol. 2009; 1:164–74.2. Carel JC, Léger J. Clinical practice. Precocious puberty. N Engl J Med. 2008; 358:2366–77.3. Parent AS, Teilmann G, Juul A, Skakkebaek NE, Toppari J, Bourguignon JP. The timing of normal puberty and the age limits of sexual precocity: variations around the world, secular trends, and changes after migration. Endocr Rev. 2003; 24:668–93.
Article4. Mills JL, Stolley PD, Davies J, Moshang T Jr. Premature thelarche. Natural history and etiologic investigation. Am J Dis Child. 1981; 135:743–5.5. Pasternak Y, Friger M, Loewenthal N, Haim A, Hershkovitz E. The utility of basal serum LH in prediction of central precocious puberty in girls. Eur J Endocrinol. 2012; 166:295–9.
Article6. Calcaterra V, De Filippo G, Albertini R, Rendina D, Messini B, Monti CM, et al. Effectiveness of basal LH in monitoring central precocious puberty treatment in girls. J Pediatr Endocrinol Metab. 2021; 34:45–50.
Article7. Fujita LGA, Palhares H, da Silva AP, Tomé JM, Borges MF. Clinical and laboratory parameters of gonadotropin-releasing hormone analog treatment effectiveness in children with precocious puberty. Clinics (Sao Paulo). 2019; 74:e1205.
Article8. Eugster EA. Treatment of central precocious puberty. J Endocr Soc. 2019; 3:965–72.
Article9. Poomthavorn P, Khlairit P, Mahachoklertwattana P. Subcutaneous gonadotropin-releasing hormone agonist (triptorelin) test for diagnosing precocious puberty. Horm Res. 2009; 72:114–9.
Article10. Bhatia S, Neely EK, Wilson DM. Serum luteinizing hormone rises within minutes after depot leuprolide injection: implications for monitoring therapy. Pediatrics. 2002; 109:E30.
Article11. Tanner JM, Whitehouse RH. Clinical longitudinal standards for height, weight, height velocity, weight velocity, and stages of puberty. Arch Dis Child. 1976; 51:170–9.
Article12. Kim JH, Yun S, Hwang SS, Shim JO, Chae HW, Lee YJ, et al. The 2017 Korean National Growth Charts for children and adolescents: development, improvement, and prospects. Korean J Pediatr. 2018; 61:135–49.
Article13. Aksglaede L, Sørensen K, Petersen JH, Skakkebaek NE, Juul A. Recent decline in age at breast development: the Copenhagen Puberty Study. Pediatrics. 2009; 123:e932–9.
Article14. Menon PS. Precocious puberty, GnRH stimulation test and monitoring GnRH analog therapy. Indian J Pediatr. 2015; 82:980–2.
Article15. Lahlou N, Carel JC, Chaussain JL, Roger M. Pharmacokinetics and pharmacodynamics of GnRH agonists: clinical implications in pediatrics. J Pediatr Endocrinol Metab. 2000; 13 Suppl 1:723–37.
Article16. Carel JC, Eugster EA, Rogol A, Ghizzoni L, Palmert MR, Antoniazzi F, et al. Consensus statement on the use of gonadotropin-releasing hormone analogs in children. Pediatrics. 2009; 123:e752–62.
Article17. Garner C. Uses of GnRH agonists. J Obstet Gynecol Neonatal Nurs. 1994; 23:563–70.
Article18. Freire AV, Escobar ME, Gryngarten MG, Arcari AJ, Ballerini MG, Bergadá I, et al. High diagnostic accuracy of subcutaneous Triptorelin test compared with GnRH test for diagnosing central precocious puberty in girls. Clin Endocrinol (Oxf ). 2013; 78:398–404.
Article19. Strich D, Kvatinsky N, Hirsch HJ, Gillis D. Triptorelin depot stimulation test for central precocious puberty. J Pediatr Endocrinol Metab. 2013; 26:631–4.
Article20. Vukovic R, Milenkovic T, Soldatovic I, Pekic S, Mitrovic K, Todorovic S. Triptorelin stimulated luteinizing hormone concentrations for diagnosing central precocious puberty: study of diagnostic accuracy. Endocrine. 2022; 75:934–41.
Article21. Houk CP, Kunselman AR, Lee PA. The diagnostic value of a brief GnRH analogue stimulation test in girls with central precocious puberty: a single 30-minute post-stimulation LH sample is adequate. J Pediatr Endocrinol Metab. 2008; 21:1113–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Usefulness of Pelvic Ultrasound in Diagnosis of Precocious Puberty
- Factors to Predict Positive Results of Gonadotropin Releasing Hormone Stimulation Test in Girls with Suspected Precocious Puberty
- Sterile Abscess Formation Associated with Two Different Forms of Gonadotropin-Releasing Hormone Agonist in Central Precocious Puberty
- Diagnosis and Treatment of Central Precocious Puberty
- Indication of Gonadotropin-Releasing Hormone Agonist: Precocious Puberty or Advanced Puberty?