Intest Res.
2024 Apr;22(2):186-207. 10.5217/ir.2023.00109.
A survey of current practices in post-polypectomy surveillance in Korea
- Affiliations
-
- 1Department of Internal Medicine, Keimyung University School of Medicine, Daegu, Korea
- 2Division of Gastroenterology, Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 3Department of Internal Medicine, Kyung Hee University Hospital at Gangdong, College of Medicine, Kyung Hee University, Seoul, Korea
- 4Department of Internal Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea
- 5Department of Internal Medicine, Chosun University College of Medicine, Gwangju, Korea
- 6Division of Gastroenterology, Department of Medicine, Soonchunhyang University Seoul Hospital, Soonchunhyang University College of Medicine, Seoul, Korea
- 7Department of Internal Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 8Division of Gastroenterology and Hepatology, Department of Internal Medicine, Institute of Digestive Disease and Nutrition, Korea University College of Medicine, Seoul, Korea
- 9Department of Internal Medicine, Ewha Womans University School of Medicine, Seoul, Korea
- 10Department of Internal Medicine, Chonnam National University Medical School, Gwangju, Korea
- 11Department of Internal Medicine, Pusan National University School of Medicine and Biomedical Research Institute, Pusan National University Hospital, Busan, Korea
- 12Department of Gastroenterology, Kyung Hee University Hospital, Seoul, Korea
- 13Department of Internal Medicine and Liver Research Institute, Seoul National University College of Medicine, Seoul, Korea
- 14Health Screening and Promotion Center, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 15Division of Gastroenterology, Department of Medicine, Soonchunhyang University Cheonan Hospital, Soonchunhyang University College of Medicine, Cheonan, Korea
- 16Department of Internal Medicine, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- 17Department of Gastroenterology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2554662
- DOI: http://doi.org/10.5217/ir.2023.00109
Abstract
- Background/Aims
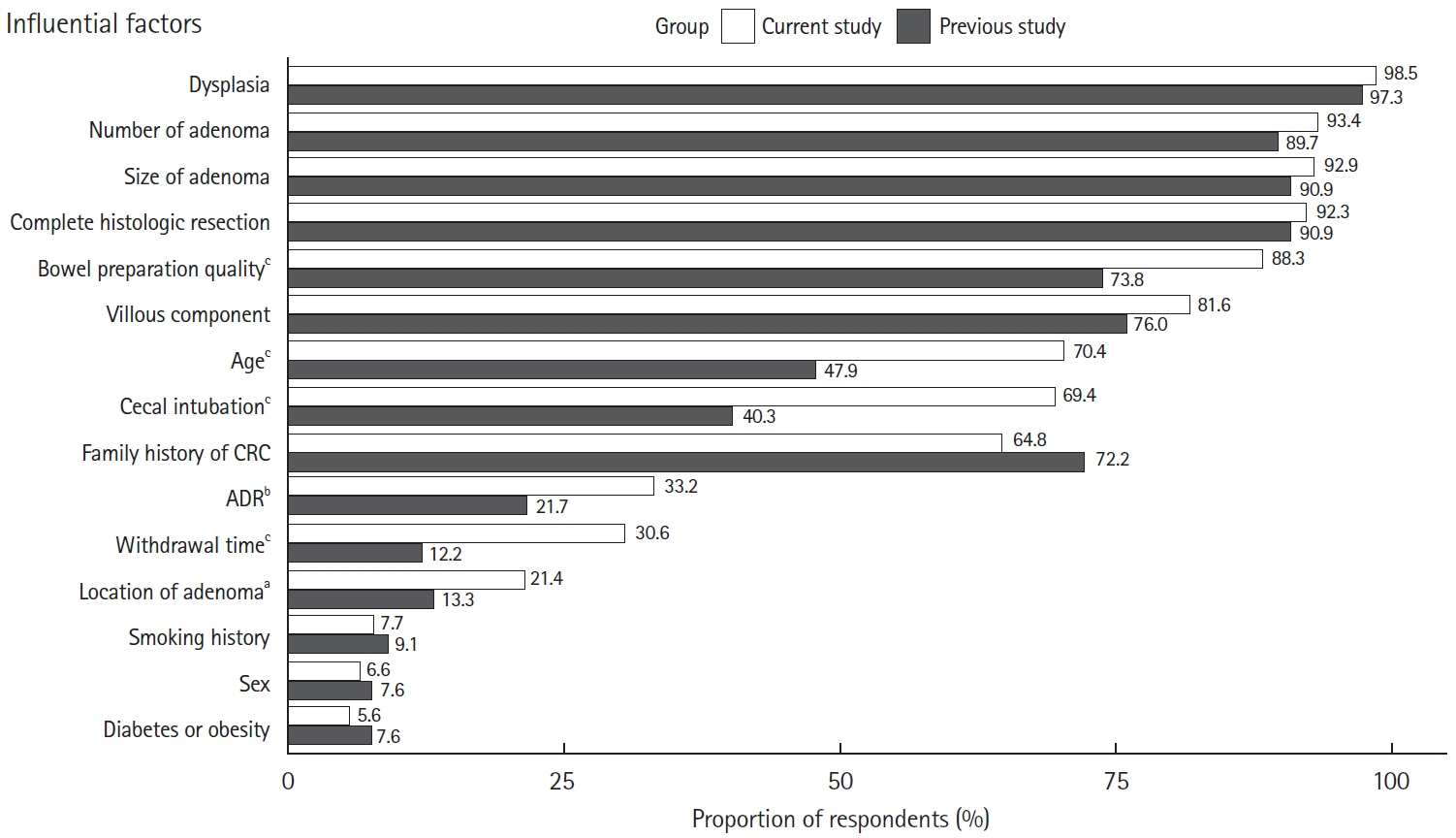
We investigated the clinical practice patterns of post-polypectomy colonoscopic surveillance among Korean endoscopists.
Methods
In a web-based survey conducted between September and November 2021, participants were asked about their preferred surveillance intervals and the patient age at which surveillance was discontinued. Adherence to the recent guidelines of the U.S. Multi-Society Task Force on Colorectal Cancer (USMSTF) was also analyzed.
Results
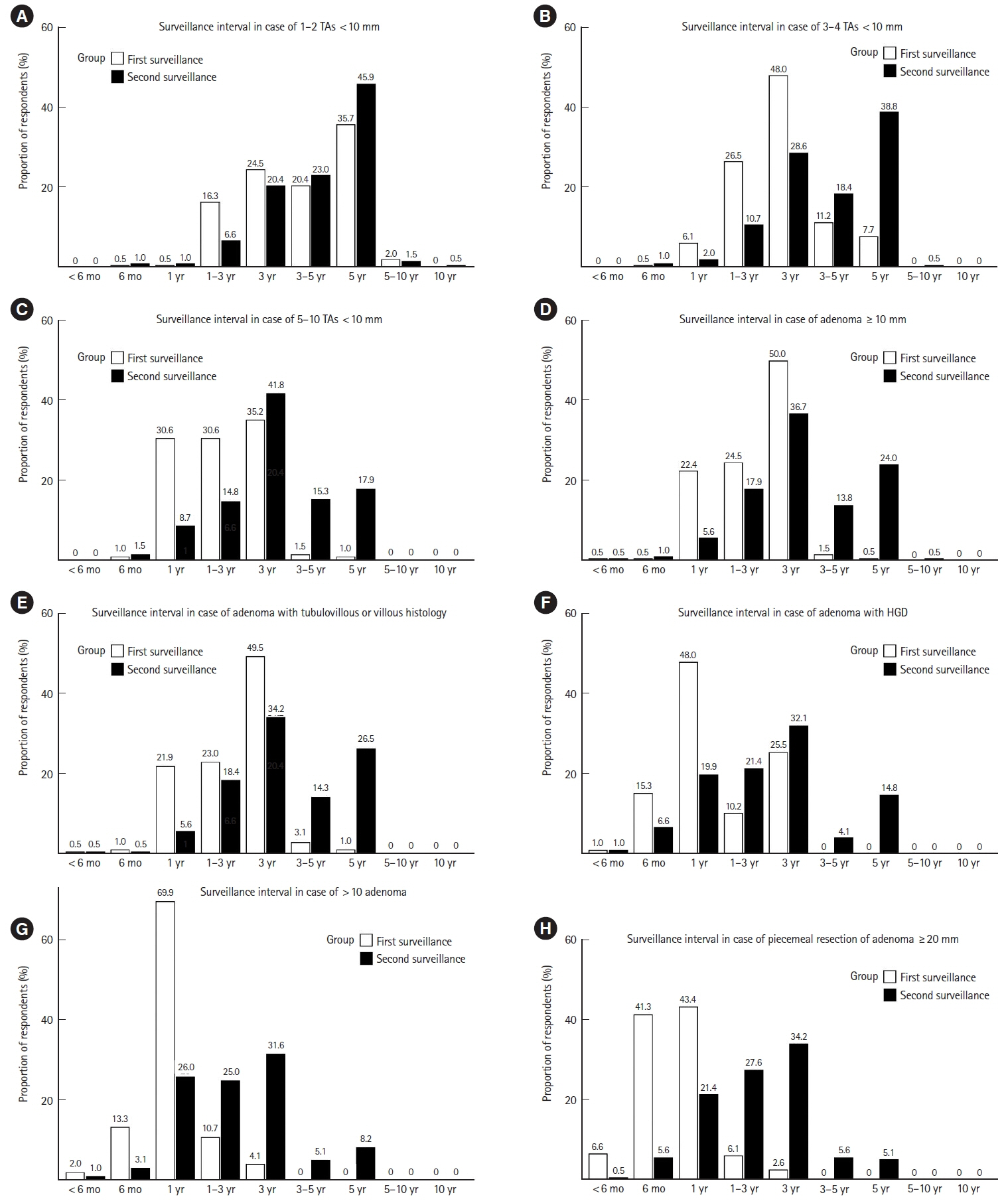
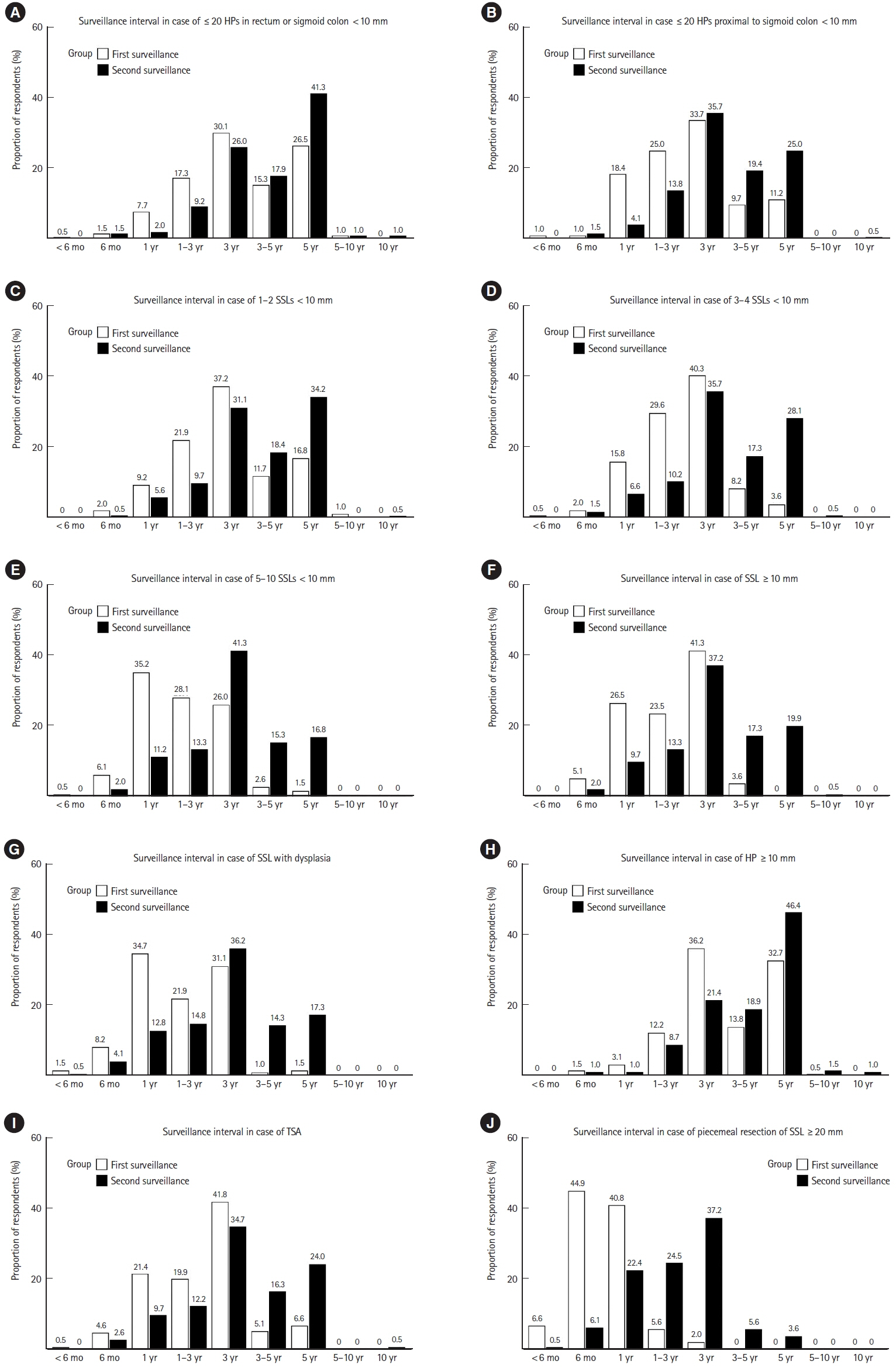
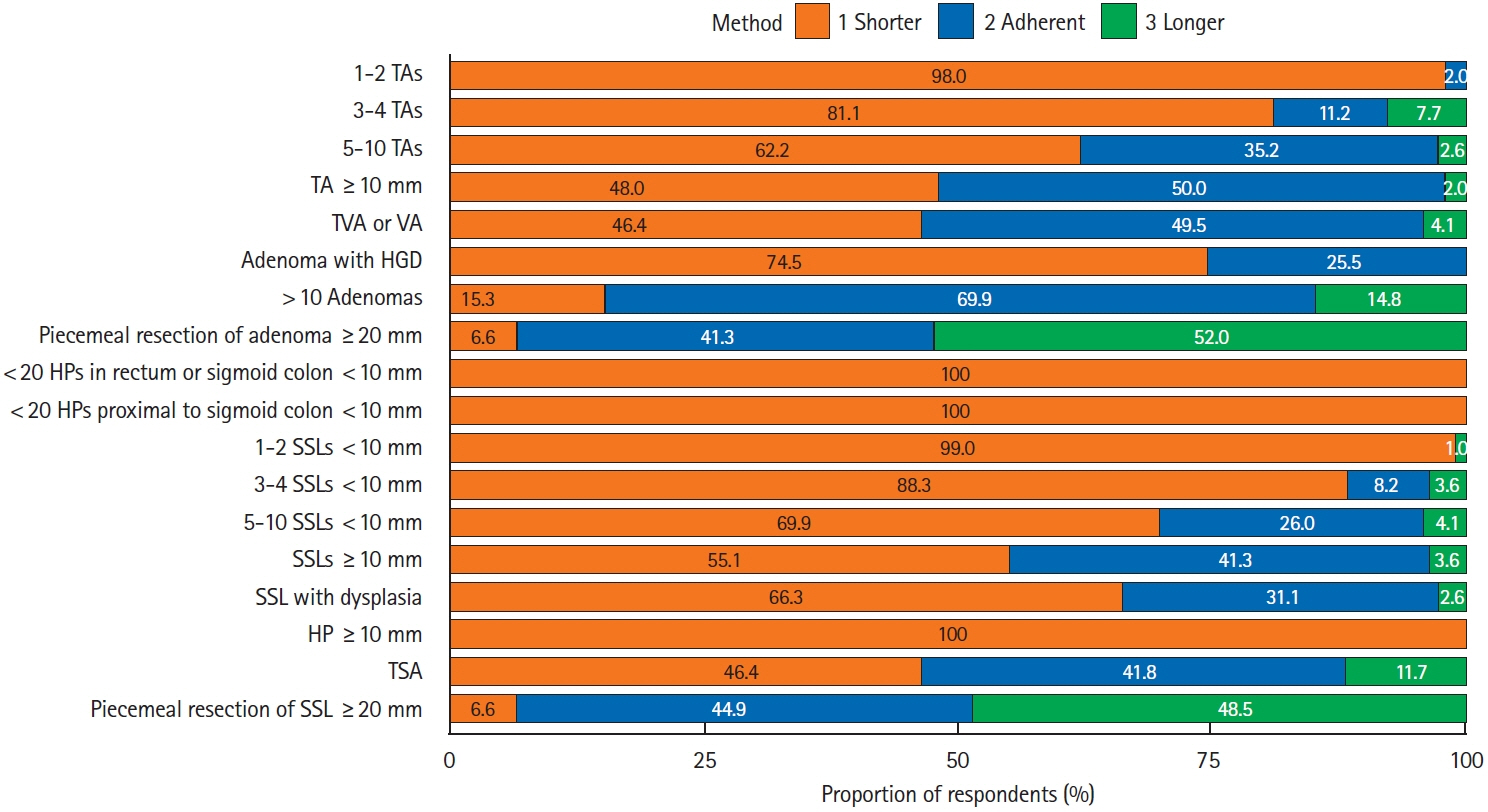
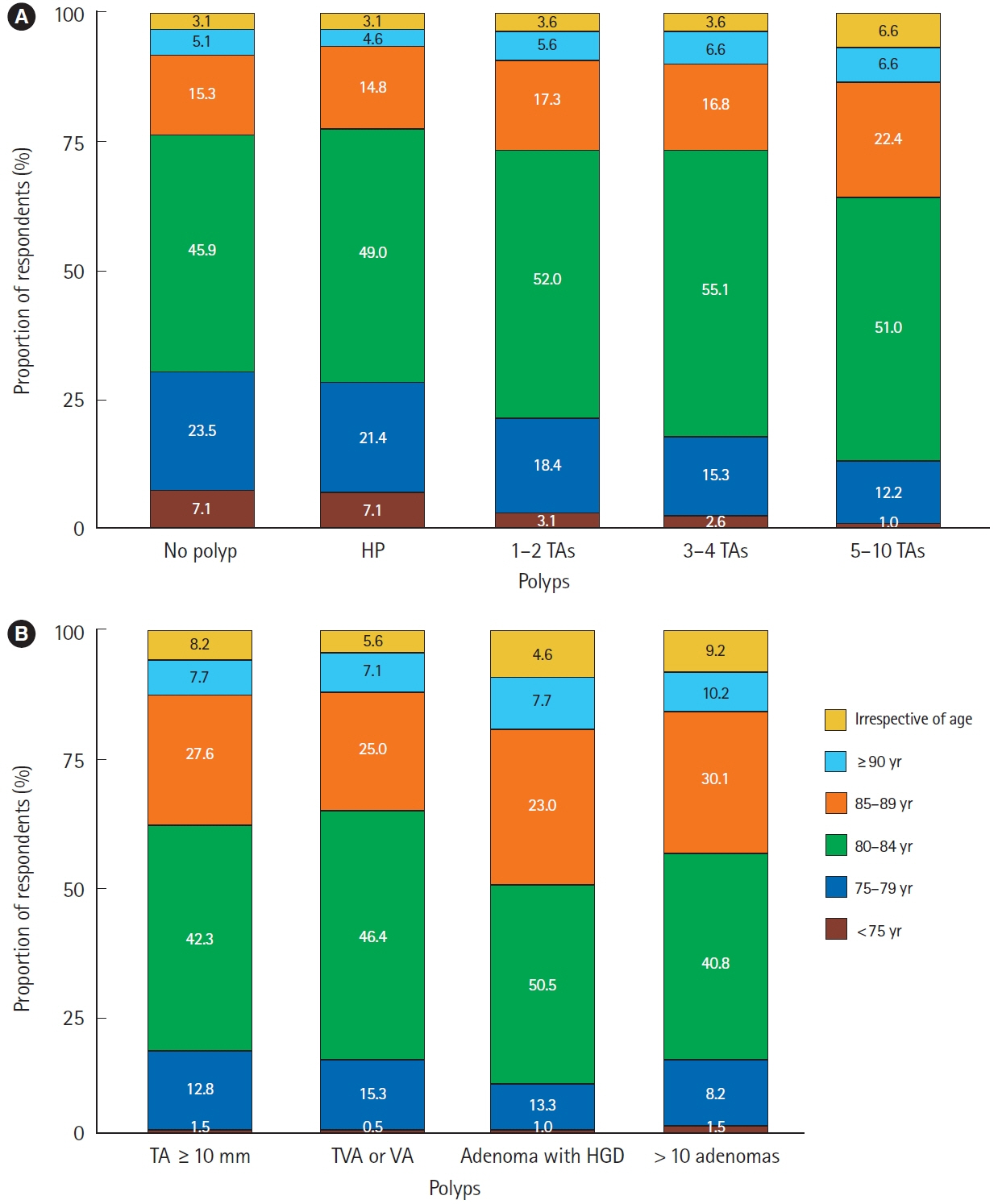
In total, 196 endoscopists completed the survey. The most preferred first surveillance intervals were: a 5-year interval after the removal of 1–2 tubular adenomas < 10 mm; a 3-year interval after the removal of 3–10 tubular adenomas < 10 mm, adenomas ≥ 10 mm, tubulovillous or villous adenomas, ≤ 20 hyperplastic polyps < 10 mm, 1–4 sessile serrated lesions (SSLs) < 10 mm, hyperplastic polyps or SSLs ≥ 10 mm, and traditional serrated adenomas; and a 1-year interval after the removal of adenomas with highgrade dysplasia, >10 adenomas, 5–10 SSLs, and SSLs with dysplasia. In piecemeal resections of large polyps ( > 20 mm), surveillance colonoscopy was mostly preferred after 1 year for adenomas and 6 months for SSLs. The mean USMSTF guideline adherence rate was 30.7%. The largest proportion of respondents (40.8%–55.1%) discontinued the surveillance at the patient age of 80–84 years.
Conclusions
A significant discrepancy was observed between the preferred post-polypectomy surveillance intervals and recent international guidelines. Individualized measures are required to increase adherence to the guidelines.
Keyword
Figure
Reference
-
1. Jung KW, Won YJ, Kang MJ, Kong HJ, Im JS, Seo HG. Prediction of cancer incidence and mortality in Korea, 2022. Cancer Res Treat. 2022; 54:345–351.
Article2. Khil H, Kim SM, Hong S, et al. Time trends of colorectal cancer incidence and associated lifestyle factors in South Korea. Sci Rep. 2021; 11:2413.
Article3. Cha JM, Kwak MS, Kim HS, et al. Real-world national colonoscopy volume in Korea: a nationwide population-based study over 12 years. Gut Liver. 2020; 14:338–346.
Article4. Cross AJ, Robbins EC, Pack K, et al. Long-term colorectal cancer incidence after adenoma removal and the effects of surveillance on incidence: a multicentre, retrospective, cohort study. Gut. 2020; 69:1645–1658.
Article5. Robbins EC, Wooldrage K, Cross AJ. Is surveillance colonoscopy necessary for all patients with bowel polyps? BMJ. 2020; m1706.
Article6. Pinsky PF, Schoen RE. Contribution of surveillance colonoscopy to colorectal cancer prevention. Clin Gastroenterol Hepatol. 2020; 18:2937–2944.
Article7. Hong SN, Yang DH, Kim YH, et al. Korean guidelines for postpolypectomy colonoscopic surveillance. Intest Res. 2012; 10:89–109.
Article8. Gupta S, Lieberman D, Anderson JC, et al. Recommendations for follow-up after colonoscopy and polypectomy: a consensus update by the US Multi-Society Task Force on Colorectal Cancer. Gastrointest Endosc. 2020; 91:463–485.
Article9. Hassan C, Antonelli G, Dumonceau JM, et al. Post-polypectomy colonoscopy surveillance: European Society of Gastrointestinal Endoscopy (ESGE) Guideline: update 2020. Endoscopy. 2020; 52:687–700.
Article10. Kim SE, Hong SP, Kim HS, et al. A Korean national survey for colorectal cancer screening and polyp diagnosis methods using web-based survey. Korean J Gastroenterol. 2012; 60:26–35.
Article11. Hong SN, Yang DH, Kim YH, et al. Surveillance and management. a survey for post-polypectomy surveillance. Intest Res. 2011; 9:118–128.12. Shin SJ, Lee SH, Park DI, et al. A Korean national survey for treatment modality in colon polypectomy. Intest Res. 2011; 9:196–205.
Article13. Oh CK, Aniwan S, Piyachaturawat P, et al. Adherence to surveillance guidelines after the removal of colorectal polyps: a multinational, multicenter, prospective survey. Gut Liver. 2021; 15:878–886.
Article14. Hong S, Suh M, Choi KS, et al. Guideline adherence to colonoscopic surveillance intervals after polypectomy in Korea: results from a nationwide survey. Gut Liver. 2018; 12:426–432.
Article15. Kim SY, Kwak MS, Yoon SM, et al. Korean guidelines for postpolypectomy colonoscopic surveillance: 2022 revised edition. Clin Endosc. 2022; 55:703–725.
Article16. Lam YF, Seto WK, Tong T, et al. Rates of metachronous adenoma after curative resection for left-sided or right-sided colon cancer. Intest Res. 2018; 16:619–627.
Article17. Lee JK, Jensen CD, Levin TR, et al. Long-term risk of colorectal cancer and related death after adenoma removal in a large, community-based population. Gastroenterology. 2020; 158:884–894.
Article18. Laiyemo AO, Murphy G, Sansbury LB, et al. Hyperplastic polyps and the risk of adenoma recurrence in the polyp prevention trial. Clin Gastroenterol Hepatol. 2009; 7:192–197.
Article19. Rutter MD, East J, Rees CJ, et al. British Society of Gastroenterology/ Association of Coloproctology of Great Britain and Ireland/ Public Health England post-polypectomy and post-colorectal cancer resection surveillance guidelines. Gut. 2020; 69:201–223.
Article20. Atkin W, Wooldrage K, Brenner A, et al. Adenoma surveillance and colorectal cancer incidence: a retrospective, multicentre, cohort study. Lancet Oncol. 2017; 18:823–834.
Article21. Atkin W, Brenner A, Martin J, et al. The clinical effectiveness of different surveillance strategies to prevent colorectal cancer in people with intermediate-grade colorectal adenomas: a retrospective cohort analysis, and psychological and economic evaluations. Health Technol Assess. 2017; 21:1–536.
Article22. Morelli MS, Glowinski EA, Juluri R, Johnson CS, Imperiale TF. Yield of the second surveillance colonoscopy based on the results of the index and first surveillance colonoscopies. Endoscopy. 2013; 45:821–826.
Article23. Imperiale TF, Juluri R, Sherer EA, Glowinski EA, Johnson CS, Morelli MS. A risk index for advanced neoplasia on the second surveillance colonoscopy in patients with previous adenomatous polyps. Gastrointest Endosc. 2014; 80:471–478.
Article24. Dubé C, Yakubu M, McCurdy BR, et al. Risk of advanced adenoma, colorectal cancer, and colorectal cancer mortality in people with low-risk adenomas at baseline colonoscopy: a systematic review and meta-analysis. Am J Gastroenterol. 2017; 112:1790–1801.
Article25. de Jonge V, Sint Nicolaas J, van Leerdam ME, Kuipers EJ, Veldhuyzen van Zanten SJ. Systematic literature review and pooled analyses of risk factors for finding adenomas at surveillance colonoscopy. Endoscopy. 2011; 43:560–572.
Article26. Johnson DA, Barkun AN, Cohen LB, et al. Optimizing adequacy of bowel cleansing for colonoscopy: recommendations from the US multi-society task force on colorectal cancer. Gastroenterology. 2014; 147:903–924.
Article27. May FP, Shaukat A. State of the science on quality indicators for colonoscopy and how to achieve them. Am J Gastroenterol. 2020; 115:1183–1190.
Article28. Cross AJ, Robbins EC, Saunders BP, Duffy SW, Wooldrage K. Higher adenoma detection rates at screening associated with lower long-term colorectal cancer incidence and mortality. Clin Gastroenterol Hepatol. 2022; 20:e148–e167.
Article29. Jung Y, Joo YE, Kim HG, et al. Relationship between the endoscopic withdrawal time and adenoma/polyp detection rate in individual colonic segments: a KASID multicenter study. Gastrointest Endosc. 2019; 89:523–530.
Article30. Shaukat A, Rector TS, Church TR, et al. Longer withdrawal time is associated with a reduced incidence of interval cancer after screening colonoscopy. Gastroenterology. 2015; 149:952–957.
Article31. Maratt JK, Calderwood AH. Colorectal cancer screening and surveillance colonoscopy in older adults. Curr Treat Options Gastroenterol. 2019; 17:292–302.
Article32. Săftoiu A, Hassan C, Areia M, et al. Role of gastrointestinal endoscopy in the screening of digestive tract cancers in Europe: European Society of Gastrointestinal Endoscopy (ESGE) Position Statement. Endoscopy. 2020; 52:293–304.
Article33. US Preventive Services Task Force, Davidson KW, Barry MJ, et al. Screening for colorectal cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2021; 325:1965–1977.34. Patel SG, May FP, Anderson JC, et al. Updates on age to start and stop colorectal cancer screening: recommendations from the U.S. Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2022; 162:285–299.
Article35. Tran AH, Man Ngor EW, Wu BU. Surveillance colonoscopy in elderly patients: a retrospective cohort study. JAMA Intern Med. 2014; 174:1675–1682.36. Rege S, Coburn E, Robertson DJ, Calderwood AH. Practice patterns and predictors of stopping colonoscopy in older adults with colorectal polyps. Clin Gastroenterol Hepatol. 2022; 20:e1050. –e1060.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Strategy for post-polypectomy colonoscopy surveillance: focus on the revised Korean guidelines
- A Survey on the Interval of Post-polypectomy Surveillance Colonoscopy
- Post-polypectomy surveillance: the present and the future
- Optimal Colonoscopy Surveillance Interval after Polypectomy
- Summary and comparison of recently updated post-polypectomy surveillance guidelines