J Cerebrovasc Endovasc Neurosurg.
2024 Mar;26(1):37-45. 10.7461/jcen.2023.E2023.06.005.
Microsurgical treatment of distal middle cerebral artery aneurysm: A single-center review
- Affiliations
-
- 1Department of Neurosurgery, Busan Paik Hospital, Inje University, School of Medicine, Busan, Korea
- 2Department of Endocrinology, Haundae Paik Hospital, Inje University, School of Medicine, Busan, Korea
- 3Department of Neurosurgery, Busan St. Mary’s Hospital, Busan, Korea
- KMID: 2554044
- DOI: http://doi.org/10.7461/jcen.2023.E2023.06.005
Abstract
Objective
To review the characteristics of distal middle cerebral artery (MCA) aneurysm treated by microsurgery, the detailed surgical options, and the clinical result.
Methods
We retrospectively reviewed cerebral aneurysm in the M2 and M3 segments of the MCA surgically treated between January 2015 and December 2022. The demographic data, aneurysm-related findings, type of surgical approach, surgical technique, and clinical outcomes of the enrolled patients were analyzed.
Results
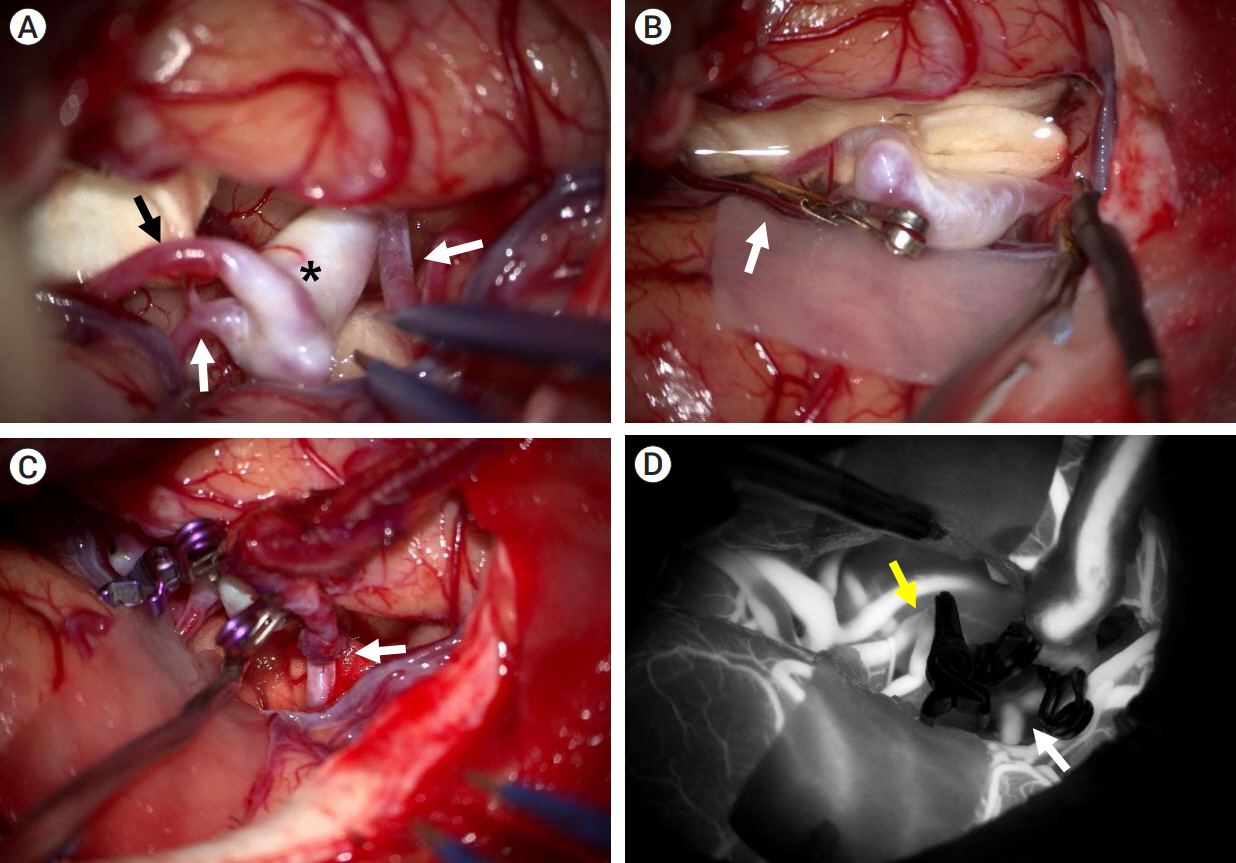
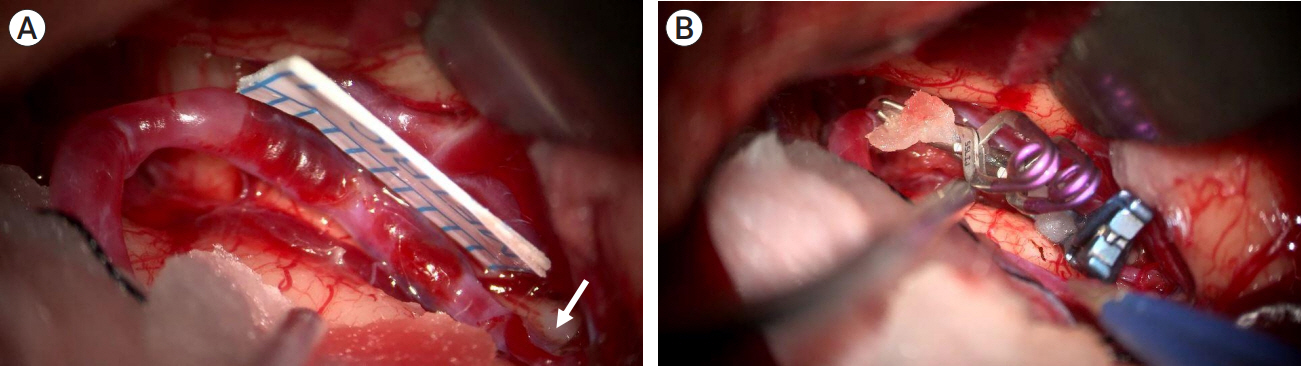
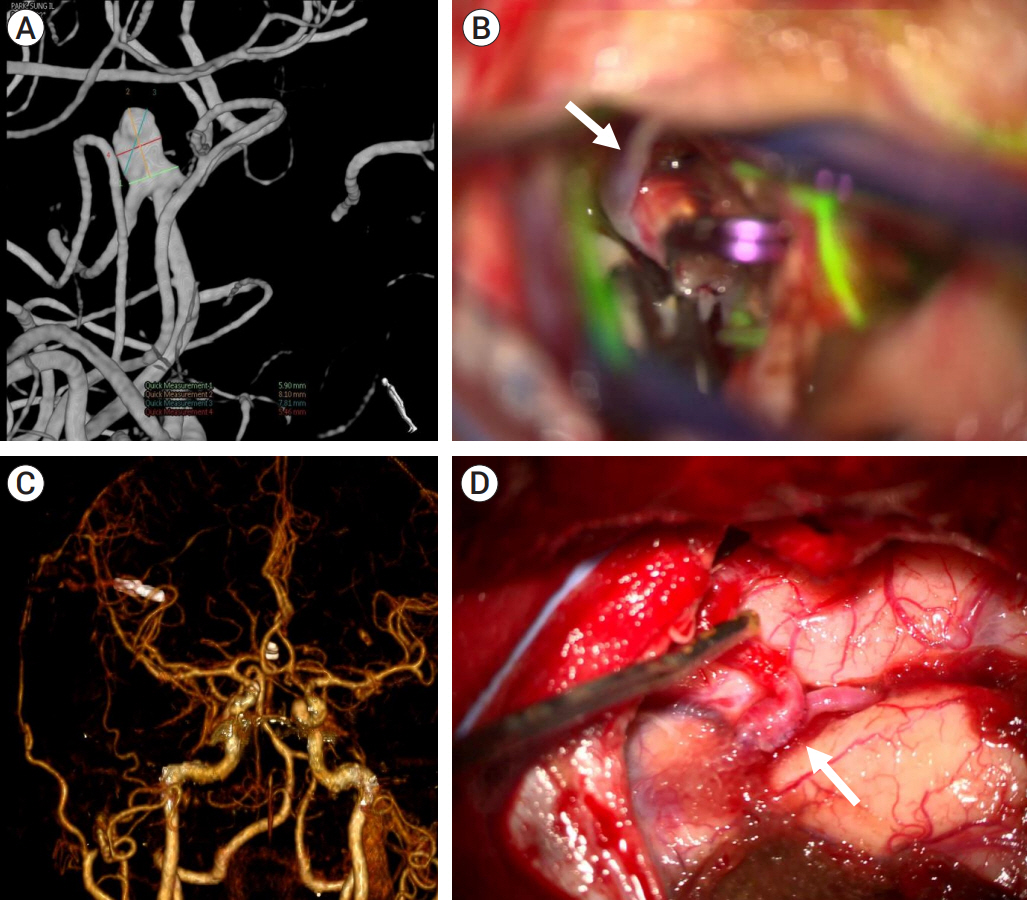
Sixteen distal MCA aneurysms were treated with microneurosurgery (incidence, 1.0%; female, 12; mean age, 58.1 years; ruptured, three). Twelve aneurysms were in the M2 segment (insular segment), two aneurysms at the M2–M3 junction, and two aneurysms in the M3 segment (opercular segment). Twelve aneurysms were saccular (average size, 4.9 mm; multiplicity, 50%; average aneurysms, 3.0; partially thrombosed, 1; sidewall aneurysm, 2). Three aneurysms were fusiform, of which two were ruptured. Of the ruptured aneurysms, one was a ruptured dissecting aneurysm. The trans-sylvian and trans-sulcal approaches were used in fourteen and two patients, respectively. Neck clipping, wrap clipping, and surgical trapping were performed in twelve, one, and one patient, respectively. Proximal occlusion was performed in one patient. Bypass technique was required in two patients (neck clipping and proximal occlusion). The modified Rankin Score was 6 in the two patients with ruptured aneurysms. The remaining patients did not show further neurological deterioration after microneurosurgery.
Conclusions
Distal MCA aneurysms had a high incidence of being diagnosed with multiple other aneurysms and were relatively non-saccular.
Figure
Reference
-
1. Acerbi F, Prada F, Vetrano IG, Falco J, Faragò G, Ferroli P, et al. Indocyanine green and contrast-enhanced ultrasound videoangiography: A synergistic approach for real-time verification of distal revascularization and aneurysm occlusion in a complex distal middle cerebral artery aneurysm. World Neurosurgery. 2019; May. 125:277–84.
Article2. Baldoncini M, Wahjoepramono EJ, Wahjoepramono POP, Campero A, Justa A, Spetzler R, et al. Wrapping technique in fusiform aneurysms. Neurol Sci Neurosurg. 2020; 2(1):111.
Article3. Baltacioğlu F, Cekirge S, Saatci I, Oztürk H, Arat A, Pamir N, et al. Distal middle cerebral artery aneurysms. Endovascular treatment results with literature review. Interv Neuroradiol. 2002; Dec. 8(4):399–407.4. Calvacante T, Derrey S, Curey S, Langlois O, Fréger P, Gérardin E, et al. Distal middle cerebral artery aneurysm: A proposition of microsurgical management. Neurochirurgie. 2013; Jun. 59(3):121–7.
Article5. Dashti R, Hernesniemi J, Niemelä M, Rinne J, Lehecka M, Shen H, et al. Microneurosurgical management of distal middle cerebral artery aneurysms. Surg Neurol. 2007; Jun. 67(6):553–63.
Article6. Lenkey C, Mitchell RJ. Microsurgical anatomy of the middle cerebral artery. J Neurosurg. 1981; Feb. 54(2):151–69.
Article7. Horiuchi T, Nakagawa F, Miyatake M, Iwashita T, Tanaka Y, Hongo K. Traumatic middle cerebral artery aneurysm: case report and review of the literature. Neurosurg Rev. 2007; Jul. 30(3):263–7. discussion 267.
Article8. Horiuchi T, Tanaka Y, Takasawa H, Murata T, Yako T, Hongo K. Ruptured distal middle cerebral artery aneurysm. J Neurosurg. 2004; Mar. 100(3):384–8.
Article9. Imada Y, Mihara C, Kawamoto H, Kurisu K. Dissection of the sylvian fissure in the trans-sylvian approach based on the morphological classification of the superficial middle cerebral vein. Neurol Med Chir (Tokyo). 2021; Dec. 61(12):731–40.
Article10. Johnson HR, South JR. Traumatic dissecting aneurysm of the middle cerebral artery. Surg Neurol. 1980; Sep. 14(3):224–6.11. Joo SP, Kim TS, Choi JW, Lee JK, Kim YS, Moon KS, et al. Characteristics and management of ruptured distal middle cerebral artery aneurysms. Acta Neurochir (Wien). 2007; 149(7):661–7.
Article12. Lee SH, Bang JS. Distal middle cerebral artery M4 aneurysm surgery using navigation-CT angiography. J Korean Neurosurg Soc. 2007; Dec. 42(6):478–80.
Article13. Lee SJ, Shim YS, Park KY, Hong CK, Lee JW, Ahn JY. Clinical characteristics and surgical treatment of patients with distal middle cerebral artery aneurysms. Korean J Cerebrovasc Surg. 2008; 10(3):508–12.14. Maekawa H, Hadeishi H. Venous-preserving Sylvian dissection. World Neurosurg. 2015; Dec. 84(6):2043–52.
Article15. Park SH, Yim MB, Lee CY, Kim E, Son EI. Intracranial fusiform aneurysms: It’s pathogenesis, clinical characteristics and managements. J Korean Neurosurg Soc. 2008; Sep. 44(3):116–23.
Article16. Piepgras DG, McGrail KM, Tazelaar HD. Intracranial dissection of the distal middle cerebral artery as an uncommon cause of distal cerebral artery aneurysm. J Neurosurg. 1994; May. 80(5):909–13.
Article17. Rinne J, Hernesniemi J, Niskanen M, Vapalahti M. Analysis of 561 patients with 690 middle cerebral artery aneurysms: Anatomic and clinical features as correlated to management outcome. Neurosurgery. 1996; Jan. 38(1):2–11.
Article18. Rodríguez-Hernández A, Lawton MT. Flash fluorescence with indocyanine green videoangiography to identify the recipient artery for bypass with distal middle cerebral artery aneurysms: Operative technique. Neurosurgery. 2012; Jun. 70(2 Suppl Operative):209–20.19. Seo D, Lee SU, Oh CW, Kwon OK, Ban SP, Kim T, et al. Characteristics and clinical course of fusiform middle cerebral artery aneurysms according to location, size, and configuration. J Korean Neurosurg Soc. 2019; Nov. 62(6):649–60.
Article20. Sotero FD, Rosário M, Fonseca AC, Ferro JM. Neurological complications of infective endocarditis. Curr Neurol Neurosci Rep. 2019; Mar. 19(5):23.
Article21. Sturiale CL, Brinjikji W, Murad MH, Cloft HJ, Kallmes DF, Lanzino G. Endovascular treatment of distal anterior cerebral artery aneurysms: Single-center experience and a systematic review. AJNR Am J Neuroradiol. 2013; Dec. 34(12):2317–20.
Article22. Sung SK, Cho WH, Lee SW, Choi CH. Surgical treatment of distal middle cerebral artery aneurysms. Korean J Cerebrovasc Surg. 2004; 6(1):45–9.23. Tayebi Meybodi A, Huang W, Benet A, Kola O, Lawton MT. Bypass surgery for complex middle cerebral artery aneurysms: An algorithmic approach to revascularization. J Neurosurg. 2017; Sep. 127(3):463–79.
Article24. Tsutsumi K, Horiuchi T, Nagm A, Toba Y, Hongo K. Clinical characteristics of ruptured distal middle cerebral artery aneurysms: Review of the literature. J Clin Neurosci. 2017; Jun. 40:14–7.
Article25. Varma S, Banh L, Smith P. Traumatic aneurysm of the cortical middle cerebral artery. BMJ Case Rep. 2017; Feb. 2017:bcr 2017219301.
Article26. Widmann G, Schullian P, Ortler M, Bale R. Frameless stereotactic targeting devices: Technical features, targeting errors and clinical results. Int J Med Robot. 2012; Mar. 8(1):1–16.
Article27. Wiebers DO, Whisnant JP, Huston J 3rd, Meissner I, Brown RD Jr, Piepgras DG, et al. Unruptured intracranial aneurysms: Natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet. 2003; Jul. 362(9378):103–10.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Coil Embolization for Distal Middle Cerebral Artery Aneurysm
- Middle Cerebral Artery Aneurysm in a Premature Neonate
- Surgical Management of the Distal Anterior Cerebral Artery Aneurysms
- A Surgical Experience of the Distal Posterior Cerebral Artery Aneurysm
- Microsurgical Anatomy of the Middle Cerebral Artery