J Surg Ultrasound.
2023 May;10(1):14-23. 10.46268/jsu.2023.10.1.14.
Ultrasound (US)-Guided Ablation of Thyroid Nodules
- Affiliations
-
- 1Department of Surgery, Joau Clinic, Suwon, Korea
- KMID: 2552569
- DOI: http://doi.org/10.46268/jsu.2023.10.1.14
Abstract
- The conventional treatment of symptomatic benign thyroid nodules is surgical excision under general anesthesia. Ultrasound-guided ablation of thyroid nodules has emerged as an alternative to surgery for symptomatic benign thyroid nodules. The procedure can be performed on an outpatient basis and has a low complication rate. Cystic thyroid nodules can be effectively managed with percutaneous ethanol injections and solid thyroid nodules can be treated using thermal ablation, such as radiofrequency ablation (RFA), laser ablation (LA), high intensity focus ultrasound (HIFU), and microwave ablation. Ethanol injections use a chemical reaction and thermal ablation uses heat injury to cause the cells to break down and the nodule to shrink. In recent years, RFA is available for achieving local control of recurrences of papillary thyroid carcinoma in patients who are poor candidates for general anesthesia. RFA and LA are the most commonly used techniques. HIFU and microwave ablation are newer techniques and should be considered experimental due to insufficient evidence regarding their utility.
Keyword
Figure
Reference
-
1. Durante C, Costante G, Lucisano G, Bruno R, Meringolo D, Paciaroni A, et al. 2015; The natural history of benign thyroid nodules. JAMA. 313:926–35. DOI: 10.1001/jama.2015.0956. PMID: 25734734.
Article2. Papini E, Gugliemi R, Pacella CM. 2016; Laser, radiofrequency, and ethanol ablation for the management of thyroid nodules. Curr Opin Endocrinol Diabetes Obes. 23:400–6. DOI: 10.1097/MED.0000000000000282. PMID: 27504993.
Article3. Esnault O, Franc B, Monteil JP, Chapelon JY. 2004; High-intensity focused ultrasound for localized thyroid-tissue ablation: preliminary experimental animal study. Thyroid. 14:1072–6. DOI: 10.1089/thy.2004.14.1072. PMID: 15650361.
Article4. Hahn SY, Shin JH, Na DG, Ha EJ, Ahn HS, Lim HK, et al. 2019; Ethanol ablation of the thyroid nodules: 2018 consensus statement by the Korean Society of Thyroid Radiology. Korean J Radiol. 20:609–20. DOI: 10.3348/kjr.2018.0696. PMID: 30887743. PMCID: PMC6424836.
Article5. Guglielmi R, Pacella CM, Bianchini A, Bizzarri G, Rinaldi R, Graziano FM, et al. 2004; Percutaneous ethanol injection treatment in benign thyroid lesions: role and efficacy. Thyroid. 14:125–31. DOI: 10.1089/105072504322880364. PMID: 15068627.
Article6. Tarantino L, Francica G, Sordelli I, Sperlongano P, Parme-ggiani D, Ripa C, et al. 2008; Percutaneous ethanol injection of hyperfunctioning thyroid nodules: long-term follow-up in 125 patients. AJR Am J Roentgenol. 190:800–8. DOI: 10.2214/AJR.07.2668. PMID: 18287455.
Article7. Strajina V, Dy BM, McKenzie TJ, Al-Hilli Z, Lee RA, Ryder M, et al. 2019; Treatment of lateral neck papillary thyroid carcinoma recurrence after selective lateral neck dissection. Surgery. 165:31–6. DOI: 10.1016/j.surg.2018.04.063. PMID: 30314726.
Article8. Lewis BD, Hay ID, Charboneau JW, McIver B, Reading CC, Goellner JR. 2002; Percutaneous ethanol injection for treatment of cervical lymph node metastases in patients with papillary thyroid carcinoma. AJR Am J Roentgenol. 178:699–704. DOI: 10.2214/ajr.178.3.1780699. PMID: 11856701.
Article9. Heilo A, Sigstad E, Fagerlid KH, Grøholt KK, Berner A, Håskjold OI, et al. 2011; Efficacy of ultrasound-guided percutaneous ethanol injection treatment in patients with a limited number of metastatic cervical lymph nodes from papillary thyroid carcinoma. J Clin Endocrinol Metab. 96:2750–5. DOI: 10.1210/jc.2010-2952. PMID: 21715533.
Article10. Sung JY, Baek JH, Kim KS, Lee D, Yoo H, Kim JK, et al. 2013; Single-session treatment of benign cystic thyroid nodules with ethanol versus radiofrequency ablation: a prospective rando-mized study. Radiology. 269:293–300. DOI: 10.1148/radiol.13122134. PMID: 23616630.
Article11. Baek JH, Ha EJ, Choi YJ, Sung JY, Kim JK, Shong YK. 2015; Radiofrequency versus ethanol ablation for treating predominantly cystic thyroid nodules: a randomized clinical trial. Korean J Radiol. 16:1332–40. DOI: 10.3348/kjr.2015.16.6.1332. PMID: 26576124. PMCID: PMC4644756.
Article12. Kim YJ, Baek JH, Ha EJ, Lim HK, Lee JH, Sung JY, et al. 2012; Cystic versus predominantly cystic thyroid nodules: efficacy of ethanol ablation and analysis of related factors. Eur Radiol. 22:1573–8. DOI: 10.1007/s00330-012-2406-5. PMID: 22437920.
Article13. Park HS, Yim Y, Baek JH, Choi YJ, Shong YK, Lee JH. 2019; Ethanol ablation as a treatment strategy for benign cystic thyroid nodules: a comparison of the ethanol retention and aspiration techniques. Ultrasonography. 38:166–71. DOI: 10.14366/usg.18033. PMID: 30317854. PMCID: PMC6443594.
Article14. Suh CH, Baek JH, Ha EJ, Choi YJ, Lee JH, Kim JK, et al. 2015; Ethanol ablation of predominantly cystic thyroid nodules: evaluation of recurrence rate and factors related to recurrence. Clin Radiol. 70:42–7. DOI: 10.1016/j.crad.2014.09.008. PMID: 25443776.
Article15. Valcavi R, Frasoldati A. 2004; Ultrasound-guided percutaneous ethanol injection therapy in thyroid cystic nodules. Endocr Pract. 10:269–75. DOI: 10.4158/EP.10.3.269. PMID: 15310546.
Article16. Zhu Q, Shen Y, Zhang A, Xu LX. 2013; Numerical study of the influence of water evaporation on radiofrequency ablation. Bio-med Eng Online. 12:127. DOI: 10.1186/1475-925X-12-127. PMID: 24325296. PMCID: PMC3904760.
Article17. Kim JH, Baek JH, Lim HK, Ahn HS, Baek SM, Choi YJ, et al. 2018; 2017 thyroid radiofrequency ablation guideline: Korean Society of Thyroid Radiology. Korean J Radiol. 19:632–55. DOI: 10.3348/kjr.2018.19.4.632. PMID: 29962870. PMCID: PMC6005940.
Article18. Jang SW, Baek JH, Kim JK, Sung JY, Choi H, Lim HK, et al. 2012; How to manage the patients with unsatisfactory results after ethanol ablation for thyroid nodules: role of radiofrequency ablation. Eur J Radiol. 81:905–10. DOI: 10.1016/j.ejrad.2011.02.039. PMID: 21388767.
Article19. Lee JH, Kim YS, Lee D, Choi H, Yoo H, Baek JH. 2010; Radio-frequency ablation (RFA) of benign thyroid nodules in patients with incompletely resolved clinical problems after ethanol ablation (EA). World J Surg. 34:1488–93. DOI: 10.1007/s00268-010-0565-6. PMID: 20376445.
Article20. Cesareo R, Palermo A, Benvenuto D, Cella E, Pasqualini V, Bernardi S, et al. 2019; Efficacy of radiofrequency ablation in autonomous functioning thyroid nodules. A systematic review and meta-analysis. Rev Endocr Metab Disord. 20:37–44. DOI: 10.1007/s11154-019-09487-y. PMID: 30887407.
Article21. Mazzeo S, Cervelli R, Elisei R, Tarantini G, Cappelli C, Molinaro E, et al. 2018; mRECIST criteria to assess recurrent thyroid carcinoma treatment response after radiofrequency ablation: a prospective study. J Endocrinol Invest. 41:1389–99. DOI: 10.1007/s40618-018-0886-0. PMID: 29687416.22. Chung SR, Suh CH, Baek JH, Park HS, Choi YJ, Lee JH. 2017; Safety of radiofrequency ablation of benign thyroid nodules and recurrent thyroid cancers: a systematic review and meta-analy-sis. Int J Hyperthermia. 33:920–30. DOI: 10.1080/02656736.2017.1337936. PMID: 28565997.
Article23. Chung SR, Baek JH, Choi YJ, Lee JH. 2019; Longer-term outcomes of radiofrequency ablation for locally recurrent papillary thyroid cancer. Eur Radiol. 29:4897–903. DOI: 10.1007/s00330-019-06063-5. PMID: 30805701.
Article24. Na DG, Lee JH, Jung SL, Kim JH, Sung JY, Shin JH, et al. 2012; Radiofrequency ablation of benign thyroid nodules and recurrent thyroid cancers: consensus statement and recommen-dations. Korean J Radiol. 13:117–25. DOI: 10.3348/kjr.2012.13.2.117. PMID: 22438678. PMCID: PMC3303894.
Article25. Zhang M, Luo Y, Zhang Y, Tang J. 2016; Efficacy and safety of ultrasound-guided radiofrequency ablation for treating low-risk papillary thyroid microcarcinoma: a prospective study. Thyroid. 26:1581–7. DOI: 10.1089/thy.2015.0471. PMID: 27445090.
Article26. Jeong SY, Baek JH, Choi YJ, Chung SR, Sung TY, Kim WG, et al. 2018; Radiofrequency ablation of primary thyroid carcinoma: efficacy according to the types of thyroid carcinoma. Int J Hyperthermia. 34:611–6. DOI: 10.1080/02656736.2018.1427288. PMID: 29322881.
Article27. Ding M, Tang X, Cui D, Chi J, Shi Y, Wang T, et al. 2019; Clinical outcomes of ultrasound-guided radiofrequency ablation for the treatment of primary papillary thyroid microcarcinoma. Clin Radiol. 74:712–7. DOI: 10.1016/j.crad.2019.05.012. PMID: 31253420.
Article28. Yan L, Luo Y, Zhang Y, Zhu Y, Xiao J, Lan Y, et al. 2020; The clinical application of core-needle biopsy after radiofrequency ablation for low-risk papillary thyroid microcarcinoma: a large cohort of 202 patients study. J Cancer. 11:5257–63. DOI: 10.7150/jca.42673. PMID: 32742471. PMCID: PMC7391195.
Article29. Jung SL, Baek JH, Lee JH, Shong YK, Sung JY, Kim KS, et al. 2018; Efficacy and safety of radiofrequency ablation for benign thyroid nodules: a prospective multicenter study. Korean J Radiol. 19:167–74. DOI: 10.3348/kjr.2018.19.1.167. PMID: 29354014. PMCID: PMC5768499.
Article30. Park HS, Baek JH, Park AW, Chung SR, Choi YJ, Lee JH. 2017; Thyroid radiofrequency ablation: updates on innovative devices and techniques. Korean J Radiol. 18:615–23. DOI: 10.3348/kjr.2017.18.4.615. PMID: 28670156. PMCID: PMC5447637.
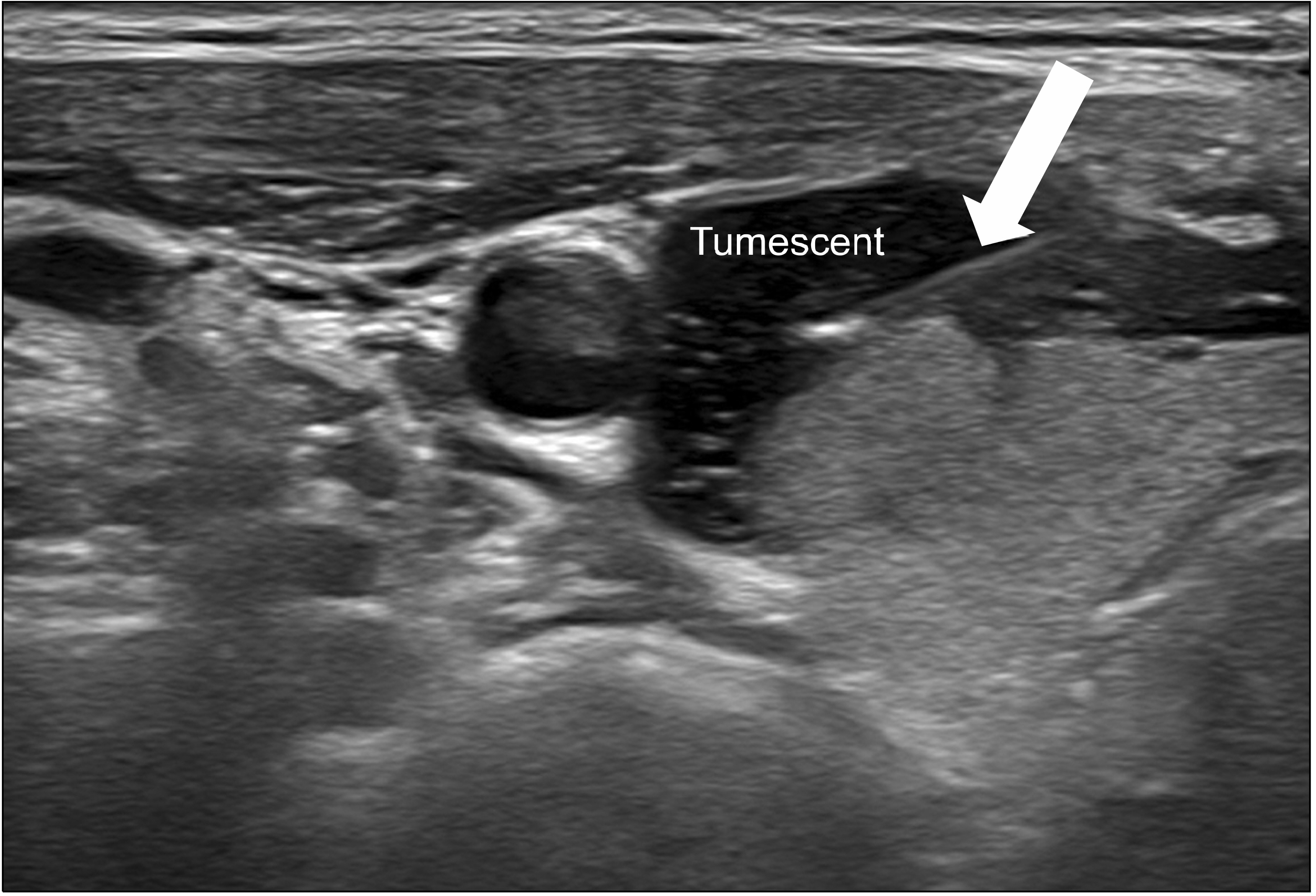
Article31. Eom TI, Kim BS. 2019; Safety and technical efficacy of tumescent anesthesia in radiofrequency ablation for thyroid nodules close to the surrounding structure. J Surg Ultrasound. 6:20–6. DOI: 10.46268/jsu.2019.6.1.20.
Article32. Lee HS, Lee BJ, Kim SW, Cha YW, Choi YS, Park YH, et al. 2009; Patterns of post-thyroidectomy hemorrhage. Clin Exp Otorhi-nolaryngol. 2:72–7. DOI: 10.3342/ceo.2009.2.2.72. PMID: 19565031. PMCID: PMC2702735.
Article33. Ha EJ, Baek JH, Lee JH. 2014; Moving-shot versus fixed electrode techniques for radiofrequency ablation: comparison in an ex-vivo bovine liver tissue model. Korean J Radiol. 15:836–43. DOI: 10.3348/kjr.2014.15.6.836. PMID: 25469097. PMCID: PMC4248641.
Article34. Shindo ML, Wu JC, Park EE. 2005; Surgical anatomy of the recurrent laryngeal nerve revisited. Otolaryngol Head Neck Surg. 133:514–9. DOI: 10.1016/j.otohns.2005.07.010. PMID: 16213921.
Article35. Cho SJ, Baek JH, Chung SR, Choi YJ, Lee JH. 2020; Long-term results of thermal ablation of benign thyroid nodules: a systematic review and meta-analysis. Endocrinol Metab (Seoul). 35:339–50. DOI: 10.3803/EnM.2020.35.2.339. PMID: 32615718. PMCID: PMC7386110.
Article36. Kim HJ, Cho SJ, Baek JH, Suh CH. 2021; Efficacy and safety of thermal ablation for autonomously functioning thyroid nodules: a systematic review and meta-analysis. Eur Radiol. 31:605–15. DOI: 10.1007/s00330-020-07166-0. PMID: 32816198.
Article37. Ha EJ, Baek JH, Lee JH. 2011; The efficacy and complications of radiofrequency ablation of thyroid nodules. Curr Opin Endocrinol Diabetes Obes. 18:310–4. DOI: 10.1097/MED.0b013e32834a9168. PMID: 21841482.
Article38. Sim JS, Baek JH. 2019; Long-term outcomes following thermal ablation of benign thyroid nodules as an alternative to surgery: the importance of controlling regrowth. Endocrinol Metab (Seoul). 34:117–23. DOI: 10.3803/EnM.2019.34.2.117. PMID: 31257739. PMCID: PMC6599899.
Article39. Sung JY, Kim YS, Choi H, Lee JH, Baek JH. 2011; Optimum first-line treatment technique for benign cystic thyroid nodules: ethanol ablation or radiofrequency ablation? AJR Am J Roentgenol. 196:W210–4. DOI: 10.2214/AJR.10.5172. PMID: 21257865.
Article40. He L, Zhao W, Xia Z, Su A, Li Z, Zhu J. 2021; Comparative efficacy of different ultrasound-guided ablation for the treatment of benign thyroid nodules: systematic review and network meta-analysis of randomized controlled trials. PLoS One. 16:e0243864. DOI: 10.1371/journal.pone.0243864. PMID: 33471820. PMCID: PMC7816973.
Article41. Matthewson K, Coleridge-Smith P, O'Sullivan JP, Northfield TC, Bown SG. 1987; Biological effects of intrahepatic neody-mium:yttrium-aluminum-garnet laser photocoagulation in rats. Gastroenterology. 93:550–7. DOI: 10.1016/0016-5085(87)90918-8. PMID: 3609664.
Article42. Papini E, Rago T, Gambelunghe G, Valcavi R, Bizzarri G, Vitti P, et al. 2014; Long-term efficacy of ultrasound-guided laser ablation for benign solid thyroid nodules. Results of a three-year multicenter prospective randomized trial. J Clin Endocrinol Metab. 99:3653–9. DOI: 10.1210/jc.2014-1826. PMID: 25050903.
Article43. Pacella CM, Mauri G, Achille G, Barbaro D, Bizzarri G, De Feo P, et al. 2015; Outcomes and risk factors for complications of laser ablation for thyroid nodules: a multicenter study on 1531 patients. J Clin Endocrinol Metab. 100:3903–10. DOI: 10.1210/jc.2015-1964. PMID: 26274342.
Article44. Pacella CM, Mauri G, Cesareo R, Paqualini V, Cianni R, De Feo P, et al. 2017; A comparison of laser with radiofrequency ablation for the treatment of benign thyroid nodules: a propensity score matching analysis. Int J Hyperthermia. 33:911–9. DOI: 10.1080/02656736.2017.1332395. PMID: 28605944.
Article45. Ha EJ, Baek JH, Kim KW, Pyo J, Lee JH, Baek SH, et al. 2015; Comparative efficacy of radiofrequency and laser ablation for the treatment of benign thyroid nodules: systematic review including traditional pooling and bayesian network meta-analy-sis. J Clin Endocrinol Metab. 100:1903–11. DOI: 10.1210/jc.2014-4077. PMID: 25695887.
Article46. Cesareo R, Pacella CM, Pasqualini V, Campagna G, Iozzino M, Gallo A, et al. 2020; Laser ablation versus radiofrequency ablation for benign non-functioning thyroid nodules: six-month results of a randomized, parallel, open-label, trial (LARA Trial). Thyroid. 30:847–56. DOI: 10.1089/thy.2019.0660. PMID: 32056501.
Article47. Ben Hamou A, Ghanassia E, Espiard S, Abi Rached H, Jannin A, Correas JM, et al. 2019; Safety and efficacy of thermal ablation (radiofrequency and laser): should we treat all types of thyroid nodules? Int J Hyperthermia. 36:666–76. DOI: 10.1080/02656736.2019.1627432. PMID: 31317800.48. Mauri G, Cova L, Monaco CG, Sconfienza LM, Corbetta S, Benedini S, et al. 2017; Benign thyroid nodules treatment using percutaneous laser ablation (PLA) and radiofrequency ablation (RFA). Int J Hyperthermia. 33:295–9. DOI: 10.1080/02656736.2016.1244707. PMID: 27701923.
Article49. Lang BH, Wu ALH. 2018; The efficacy and safety of high-intensity focused ultrasound ablation of benign thyroid nodules. Ultrasonography. 37:89–97. DOI: 10.14366/usg.17057. PMID: 29207852. PMCID: PMC5885474.
Article50. Pałyga I, Pałyga R, Młynarczyk J, Kopczyński J, Góźdź S, Kowalska A. 2020; The current state and future perspectives of high intensity focused ultrasound (HIFU) ablation for benign thyroid nodules. Gland Surg. 9(Suppl 2):S95–104. DOI: 10.21037/gs.2019.10.16. PMID: 32175250. PMCID: PMC7044088.
Article51. Trimboli P, Bini F, Marinozzi F, Baek JH, Giovanella L. 2018; High-intensity focused ultrasound (HIFU) therapy for benign thyroid nodules without anesthesia or sedation. Endocrine. 61:210–5. DOI: 10.1007/s12020-018-1560-1. PMID: 29453658.
Article52. Lang BH, Wu ALH. 2017; High intensity focused ultrasound (HIFU) ablation of benign thyroid nodules - a systematic review. J Ther Ultrasound. 5:11. DOI: 10.1186/s40349-017-0091-1. PMID: 28523127. PMCID: PMC5434558.
Article53. Glassberg MB, Ghosh S, Clymer JW, Qadeer RA, Ferko NC, Sadeghirad B, et al. 2019; Microwave ablation compared with radiofrequency ablation for treatment of hepatocellular carcinoma and liver metastases: a systematic review and meta-analysis. Onco Targets Ther. 12:6407–38. DOI: 10.2147/OTT.S204340. PMID: 31496742. PMCID: PMC6698169.54. Liu YJ, Qian LX, Liu D, Zhao JF. 2017; Ultrasound-guided microwave ablation in the treatment of benign thyroid nodules in 435 patients. Exp Biol Med (Maywood). 242:1515–23. DOI: 10.1177/1535370217727477. PMID: 28847173. PMCID: PMC5648295.
Article55. Yue WW, Wang SR, Lu F, Sun LP, Guo LH, Zhang YL, et al. 2017; Radiofrequency ablation vs. microwave ablation for patients with benign thyroid nodules: a propensity score matching study. Endocrine. 55:485–95. DOI: 10.1007/s12020-016-1173-5. PMID: 27905049.
Article56. Guo DM, Chen Z, Zhai YX, Su HH. 2021; Comparison of radiofrequency ablation and microwave ablation for benign thyroid nodules: a systematic review and meta-analysis. Clin Endo-crinol (Oxf). 95:187–96. DOI: 10.1111/cen.14438. PMID: 33556187.
Article57. Shi YF, Zhou P, Zhao YF, Liu WG, Tian SM, Liang YP. 2019; Microwave ablation compared with laser ablation for treating benign thyroid nodules in a propensity-score matching study. Front Endocrinol (Lausanne). 10:874. DOI: 10.3389/fendo.2019.00874. PMID: 31920983. PMCID: PMC6923173.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Non-surgical, Image-guided Management of Benign Thyroid Nodules
- Analyzing the adoption of radiofrequency ablation of thyroid nodules using the diffusion of innovations theory: understanding where we are in the United States?
- Percutaneous Radiofrequency Ablation for Benign Nodules of the Thyroid Gland
- The Effect of Ethanol Ablation for the Treatment of Benign Cystic Thyroid Nodules
- The efficacy and safety of high-intensity focused ultrasound ablation of benign thyroid nodules