J Korean Med Sci.
2024 Jan;39(2):e4. 10.3346/jkms.2024.39.e4.
Risk Factors for Unfavorable Outcomes of Tuberculosis in Korea: Implications for Patient-Centered
- Affiliations
-
- 1Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- 2Department of Microbiology, Brain Korea 21 Project for Graduate School of Medical Science, Yonsei University College of Medicine, Seoul, Korea
- 3Institute for Immunology and Immunological Disease, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2550804
- DOI: http://doi.org/10.3346/jkms.2024.39.e4
Abstract
- Background
The treatment success rate for tuberculosis (TB) has stagnated at 80–81% in South Korea, indicating unsatisfactory outcomes. Enhancing treatment success rate necessitates the development of individualized treatment approaches for each patient. This study aimed to identify the risk factors associated with unfavorable treatment outcomes to facilitate tailored TB care.
Methods
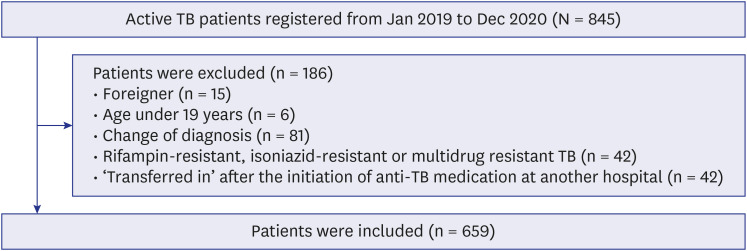
We retrospectively analyzed the data of patients with active TB between January 2019 and December 2020 at a single tertiary referral center. We classified unfavorable treatment outcomes according to the 2021 World Health Organization guidelines as follows: “lost to follow-up” (LTFU), “not evaluated” (NE), “death,” and “treatment failure” (TF). Moreover, we analyzed risk factors for each unfavorable outcome using Cox proportional hazard regression analysis.
Results
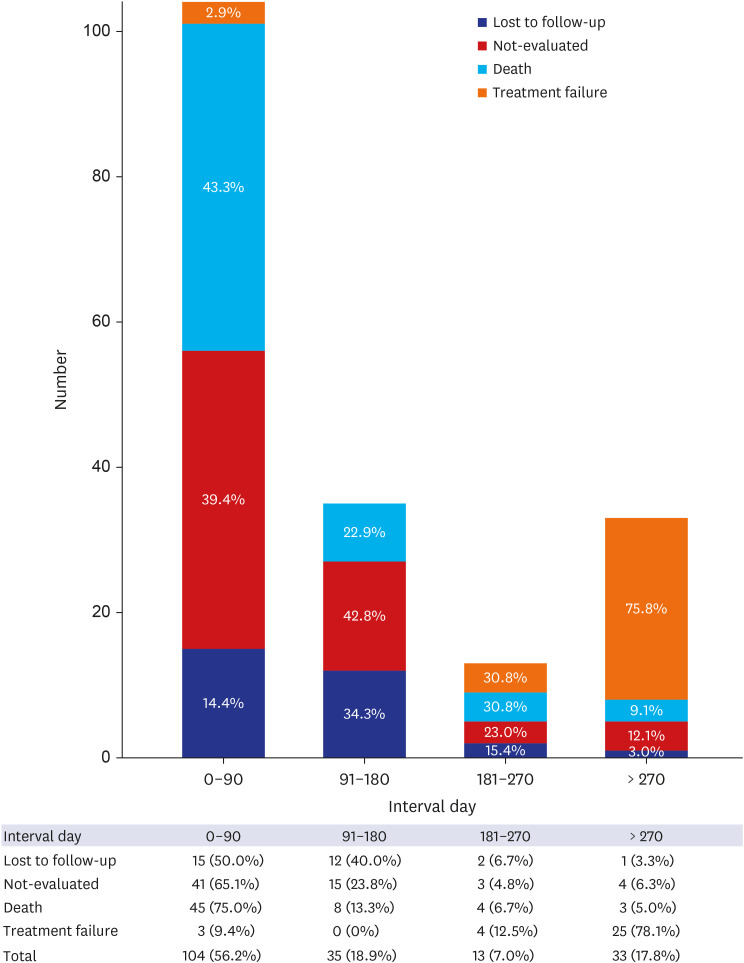
A total of 659 patients (median age 62 years; male 54.3%) were included in the study. The total unfavorable outcomes were 28.1%: 4.6% LTFU, 9.6% NE, 9.1% deaths, and 4.9% TF. Multivariate analysis showed that a culture-confirmed diagnosis of TB was associated with a lower risk of LTFU (adjusted hazard ratio [aHR], 0.25; 95% confidence interval [CI], 0.10–0.63), whereas the occurrence of adverse drug reactions (ADRs) significantly increased the risk of LTFU (aHR, 6.63; 95% CI, 2.63–16.69). Patients living far from the hospital (aHR, 4.47; 95% CI, 2.50–7.97) and those with chronic kidney disease (aHR, 3.21; 95% CI, 1.33–7.75) were at higher risk of being transferred out to other health institutions (NE). Higher mortality was associated with older age (aHR, 1.06; 95% CI, 1.04–1.09) and comorbidities. The ADRs that occurred during TB treatment were a risk factor for TF (aHR, 6.88; 95% CI, 2.24–21.13).
Conclusion
Unfavorable outcomes of patients with TB were substantial at a tertiary referral center, and the risk factors for each unfavorable outcome varied. To improve treatment outcomes, close monitoring and the provision of tailored care for patients with TB are necessary.
Figure
Reference
-
1. World Health Organization. Global Tuberculosis Report 2022. Geneva, Switzerland: Word Health Organization;2022.2. United Nations. The Sustainable Development Goals Report 2022. New York, NY, USA: United Nations;2022.3. World Health Organization. Global Strategy and Targets for Tuberculosis Prevention, Care and Control After 2015 WHA65/2012/REC/3. Geneva, Switzerland: World Health Organization;2013.4. World Health Organization. A Patient-Centered Approach to TB Care. WHO/CDS/TB/201813. Geneva, Switzerland: World Health Organization;2018.5. World Health Organization. The End TB Strategy. WHO/HTM/TH/201519. Geneva, Switzerland: World Health Organization;2015.6. Myburgh H, Baloyi D, Loveday M, Meehan SA, Osman M, Wademan D, et al. A scoping review of patient-centred tuberculosis care interventions: gaps and opportunities. PLOS Glob Public Health. 2023; 3(2):e0001357. PMID: 36963071.7. Alipanah N, Jarlsberg L, Miller C, Linh NN, Falzon D, Jaramillo E, et al. Adherence interventions and outcomes of tuberculosis treatment: a systematic review and meta-analysis of trials and observational studies. PLoS Med. 2018; 15(7):e1002595. PMID: 29969463.8. Korea Disease Control and Prevention Agency. Annual Report on the Notified Tuberculosis in Korea, 2022. Osong: Korea Disease Control and Prevention Agency;2022.9. Kim JH, Yim JJ. Achievements in and challenges of tuberculosis control in South Korea. Emerg Infect Dis. 2015; 21(11):1913–1920. PMID: 26485188.10. Kim J, Han J, Kwon Y, Choi H. Treatment outcomes among drug-susceptible patients with tuberculosis in the Republic of Korea, 2019 & 2020. Public Health Wkly Rep. 2023; 16(12):329–353.11. Linh NN, Viney K, Gegia M, Falzon D, Glaziou P, Floyd K, et al. World Health Organization treatment outcome definitions for tuberculosis: 2021 update. Eur Respir J. 2021; 58(2):2100804. PMID: 34413124.12. Lee H, Kim J, Park G, Choi H. Characteristics of notified tuberculosis cases & Republic of Korea, 2022. Public Health Wkly Rep. 2023; 16(28):931–949.13. Yu S, Sohn H, Kim HY, Kim H, Oh KH, Kim HJ, et al. Evaluating the impact of the nationwide public-private mix (PPM) program for tuberculosis under National Health Insurance in South Korea: a difference in differences analysis. PLoS Med. 2021; 18(7):e1003717. PMID: 34260579.14. Kim HJ, Bai GH, Kang MK, Kim SJ, Lee JK, Cho SI, et al. A public-private collaboration model for treatment intervention to improve outcomes in patients with tuberculosis in the private sector. Tuberc Respir Dis. 2009; 66(5):349–357.15. Min J, Kim HW, Koo HK, Ko Y, Oh JY, Kim J, et al. Impact of COVID-19 pandemic on the national PPM tuberculosis control project in Korea: the Korean PPM monitoring database between July 2019 and June 2020. J Korean Med Sci. 2020; 35(43):e388. PMID: 33169559.16. Oh AL, Makmor-Bakry M, Islahudin F, Wong IC. Prevalence and predictive factors of tuberculosis treatment interruption in the Asia region: a systematic review and meta-analysis. BMJ Glob Health. 2023; 8(1):e010592.17. San Lin K. Loss to follow-up (LTFU) during tuberculosis treatment. Bacha U, Rozman U, Turk SŠ, editors. Healthcare Access-Regional Overviews. London, UK: IntechOpen;2019.18. Sanchez-Padilla E, Marquer C, Kalon S, Qayyum S, Hayrapetyan A, Varaine F, et al. Reasons for defaulting from drug-resistant tuberculosis treatment in Armenia: a quantitative and qualitative study. Int J Tuberc Lung Dis. 2014; 18(2):160–167. PMID: 24429307.19. Tekle B, Mariam DH, Ali A. Defaulting from DOTS and its determinants in three districts of Arsi Zone in Ethiopia. Int J Tuberc Lung Dis. 2002; 6(7):573–579. PMID: 12102295.20. Gholami K, Kamali E, Hajiabdolbaghi M, Shalviri G. Evaluation of anti-tuberculosis induced adverse reactions in hospitalized patients. Pharm Pract (Granada). 2006; 4(3):134–138. PMID: 25214900.21. Kim HW, Min J, Shin AY, Koo HK, Lim SY, Park MJ, et al. Reasons why patients with tuberculosis in South Korea stop anti-TB treatment: a cross-sectional study. Int J Tuberc Lung Dis. 2020; 24(10):1016–1023. PMID: 33126933.22. Kim HW, Park S, Min J, Sun J, Shin AY, Ha JH, et al. Hidden loss to follow-up among tuberculosis patients managed by public-private mix institutions in South Korea. Sci Rep. 2022; 12(1):12362. PMID: 35859107.23. Kim AM, Cho S, Kim HJ, Jung H, Jo MW, Lee JY, et al. Primary care patients’ preference for hospitals over clinics in Korea. Int J Environ Res Public Health. 2018; 15(6):1119. PMID: 29848995.24. Karo B, Hauer B, Hollo V, van der Werf MJ, Fiebig L, Haas W. Tuberculosis treatment outcome in the European Union and European Economic Area: an analysis of surveillance data from 2002-2011. Euro Surveill. 2015; 20(49):25. Caraux-Paz P, Diamantis S, de Wazières B, Gallien S. Tuberculosis in the Elderly. J Clin Med. 2021; 10(24):5888. PMID: 34945187.26. Hase I, Toren KG, Hirano H, Sakurai K, Horne DJ, Saito T, et al. Pulmonary tuberculosis in older adults: increased mortality related to tuberculosis within two months of treatment initiation. Drugs Aging. 2021; 38(9):807–815. PMID: 34224105.27. Rajagopalan S. Tuberculosis and aging: a global health problem. Clin Infect Dis. 2001; 33(7):1034–1039. PMID: 11528577.28. Mok J, An D, Kim S, Lee M, Kim C, Son H. Treatment outcomes and factors affecting treatment outcomes of new patients with tuberculosis in Busan, South Korea: a retrospective study of a citywide registry, 2014-2015. BMC Infect Dis. 2018; 18(1):655. PMID: 30545315.29. Mkopi A, Range N, Lwilla F, Egwaga S, Schulze A, Geubbels E, et al. Adherence to tuberculosis therapy among patients receiving home-based directly observed treatment: evidence from the United Republic of Tanzania. PLoS One. 2012; 7(12):e51828. PMID: 23284782.30. Jesus GS, Pescarini JM, Silva AF, Torrens A, Carvalho WM, Junior EP, et al. The effect of primary health care on tuberculosis in a nationwide cohort of 7·3 million Brazilian people: a quasi-experimental study. Lancet Glob Health. 2022; 10(3):e390–e397. PMID: 35085514.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Risk Factors of Unfavorable Outcomes, Major Bleeding, and All-Cause Mortality in Patients with Venous Thromboembolism
- A descriptive study on the tuberculosis mortality in a tuberculosis- centered hospital
- The Influence of Unfavorable Aortoiliac Anatomy on Short-Term Outcomes after Endovascular Aortic Repair
- Risk Factors Predicting Unfavorable Neurological Outcome during the Early Period after Traumatic Brain Injury
- Relationships among Person-centered Care Environment, Patient Engagement, and Patient Outcomes in Stroke Rehabilitation Patients: A Path Model Analysis