J Cerebrovasc Endovasc Neurosurg.
2023 Dec;25(4):440-446. 10.7461/jcen.2023.E2022.12.004.
Iatrogenic mixed pial and dural arteriovenous fistula after pterional approach for surgical clipping of aneurysm: A case report
- Affiliations
-
- 1Department of Neurosurgery, Dongsan Medical Center, Keimyung University School of Medicine, Daegu, Korea
- KMID: 2549450
- DOI: http://doi.org/10.7461/jcen.2023.E2022.12.004
Abstract
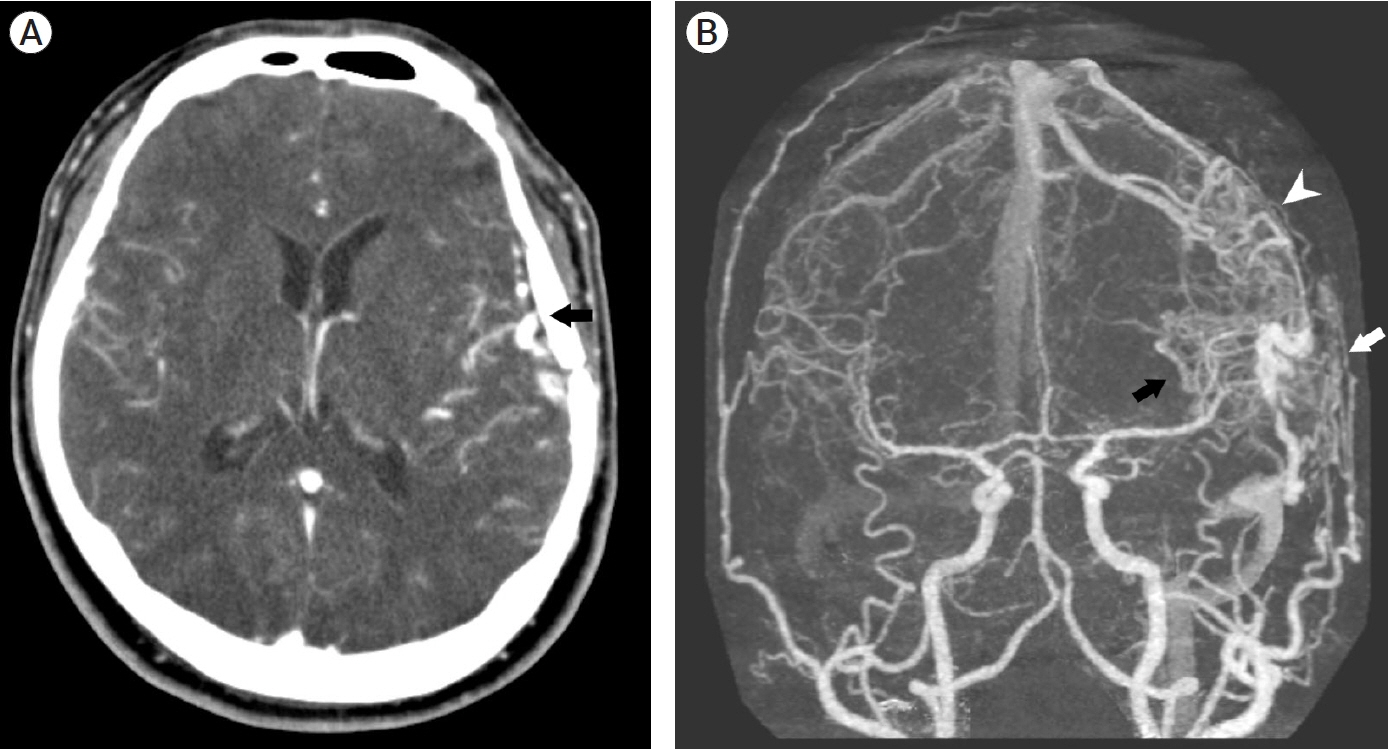
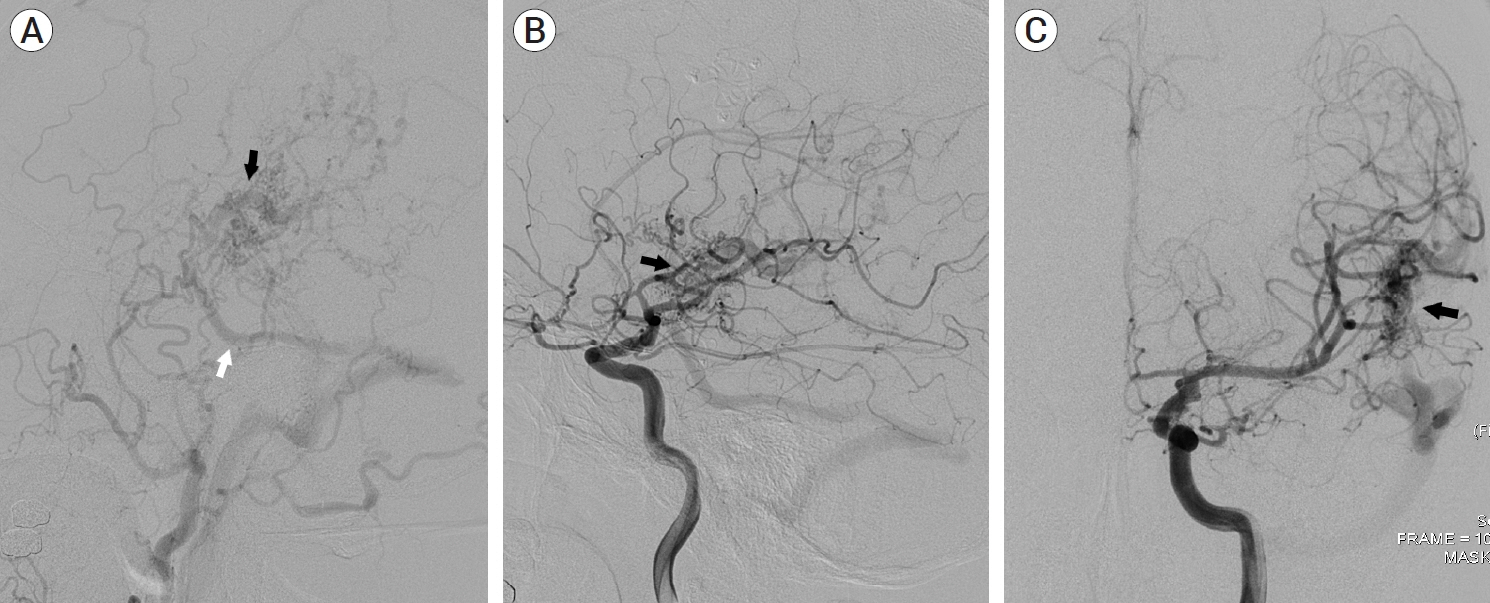
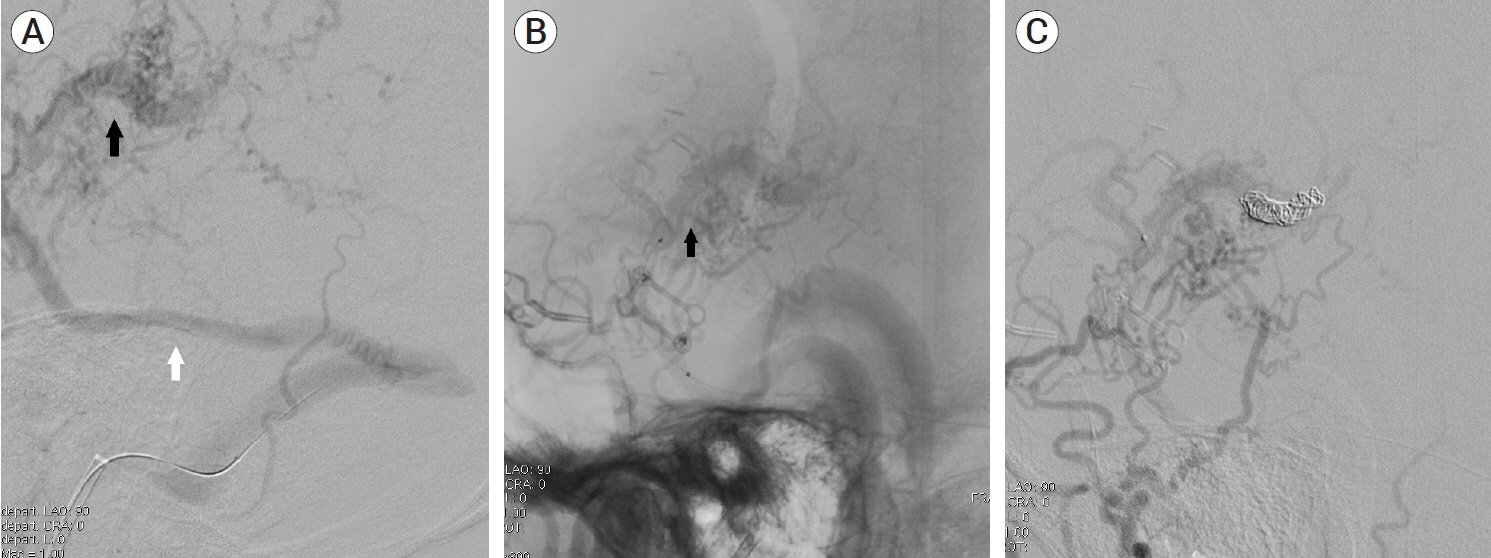
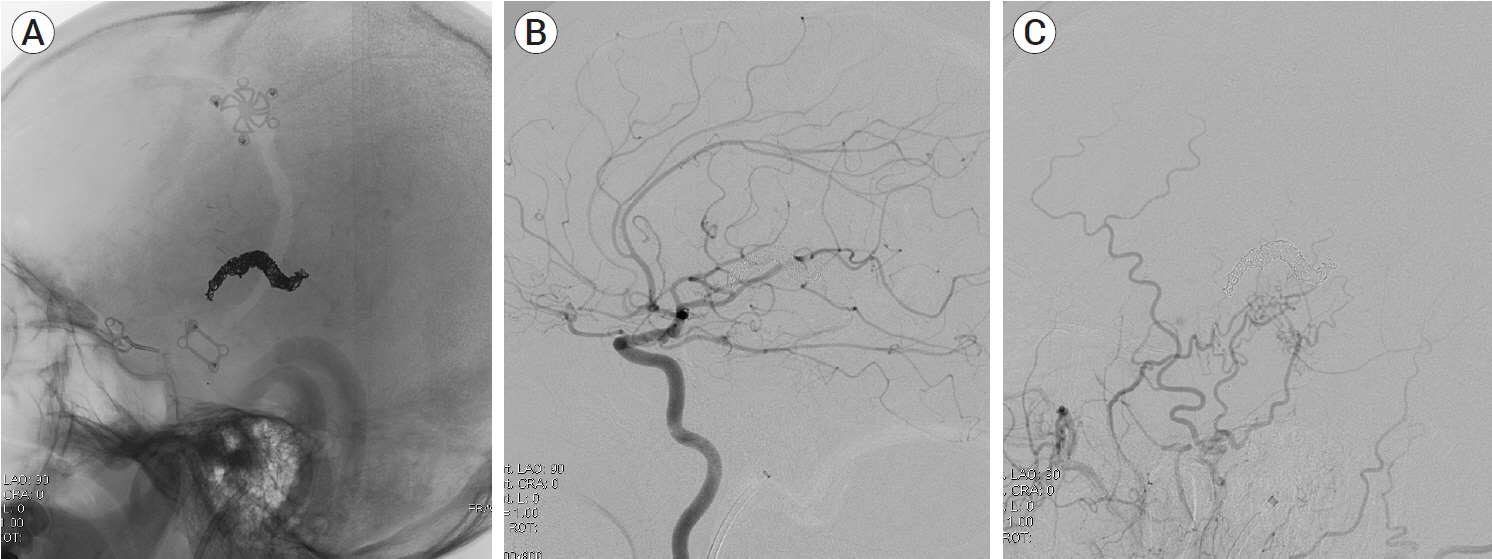
- Craniotomy is known as a cause of iatrogenic dural cerebral arteriovenous fistula (AVF). However, mixed pial and dural AVFs after craniotomy are extremely rare and require accurate diagnosis and prompt treatment due to their aggressiveness. We present a case of an iatrogenic mixed pial and dural AVF diagnosed 2 years after pterional craniotomy for surgical clipping of a ruptured anterior choroidal aneurysm. The lesion was successfully treated using single endovascular procedure of transvenous coil embolization through the engorged vein of Labbe and the superficial middle cerebral vein. The possibility of the AVF formation after the pterional approach should always be kept in mind because it usually occurs at the middle cranial fossa, which frequently has an aggressive nature owing to direct cortical venous or leptomeningeal drainage patterns. This complication is believed to be caused by angiogenetic conditions due to coagulation, retraction, and microinjuries of the perisylvian vessels, and can be prevented by performing careful sylvian dissection according to patient-specific perisylvian venous anatomy.
Figure
Reference
-
1. Ahn JY, Kim OJ, Joo YJ, Joo JY. Dural arteriovenous malformation occurring after craniotomy for pial arteriovenous malformation. J Clin Neurosci. 2003; Jan. 10(1):134–6.2. Atsushi S, Mikawa S, Akamatsu Y, Saito H, Seki H. A case of multiple pial arteriovenous fistulas associated with dural arteriovenous fistula. J Neurosurg. 2008; Dec. 109(6):1103–7.3. Bhogal P, Yeo LL, Henkes H, Krings T, Soderman M. The role of angiogenesis in dural arteriovenous fistulae: The story so far. Interv Neuroradiol. 2018; Aug. 24(4):450–4.4. Demartini Z Jr, Laurenti M, Oliveira T, Koppe G, Santos M, Francisco A. Postoperative dural arteriovenous fistula after clipping of ruptured saccular aneurysm of pericallosal artery. Arq Bras Neurocir. 2016; 35(3):248–52.5. Ding D, Brew S, McGuinness B, Mee EW. Iatrogenic dural arteriovenous fistula after surgical resection of a ruptured brain arteriovenous malformation. J Neurosci Rural Pract. 2016; Oct-Dec. 7(4):604–6.6. Doi K, Otani N, Hayashi M, Takeuchi S, Toyooka T, Wada K. Mixed pial and dural arteriovenous fistula after craniotomy: Case report and literature review. Br J Neurosurg. 2019; Oct. 1–4.7. Funakoshi Y, Hatano T, Saka M, Ando M, Chihara H, Takita W, et al. Dural and pial arteriovenous fistulas connected to the same drainer in the middle cranial fossa: A case report. World Neurosurg. 2018; Oct. 118:47–52.8. Ghali MGZ. Sphenoid dural arteriovenous fistulas. Neurosurg Rev. 2021; Feb. 44(1):77–96.9. Higashida T. Delayed postoperative dural arteriovenous fistula presenting with progressive dementia. BMJ Case Rep. 2015; Dec. 2015:bcr2015212874.10. Huang MC, Wang YC, Huang JS, Huang KM. Postoperative developmental dural arteriovenous fistula. Formosan Journal of Surgery. 2015; 48(3):102–6.11. Imada Y, Kurisu K, Takumi T, Aoyama H, Sadatomo T, Migita K, et al. Morphological pattern and classification of the superficial middle cerebral vein by cadaver dissections: An embryological viewpoint. Neurol Med Chir (Tokyo). 2019; Jul. 59(7):264–70.12. Imada Y, Mihara C, Kawamoto H, Kurisu K. Dissection of the sylvian fissure in the trans-sylvian approach based on the morphological classification of the superficial middle cerebral vein. Neurol Med Chir (Tokyo). 2021; Dec. 61(12):731–40.13. Kanematsu R, Hanakita J, Takahashi T, Tomita Y, Minami M. An acquired cervical dural arteriovenous fistula after cervical anterior fusion: Case report and literature review. World Neurosurg. 2019; Aug. 128:50–4.14. Kim SW, Chae KS, Shim JH, Rho SJ, Choi HK, Park HS. Iatrogenic dural arteriovenous fistula after superficial temporal artery to middle cerebral artery anastomosis: A case report. Korean J Neurotrauma. 2015; Oct. 11(2):151–3.15. Lee JY, Son YJ, Kim JE. Intracranial pial arteriovenous fistulas. J Korean Neurosurg Soc. 2008; Aug. 44(2):101–4.16. Li Q, Zhang Q, Huang QH, Fang YB, Zhang ZL, Xu Y, et al. A pivotal role of the vascular endothelial growth factor signaling pathway in the formation of venous hypertension-induced dural arteriovenous fistulas. Mol Med Rep. 2014; May. 9(5):1551–8.17. Maekawa H, Hadeishi H. Venous-preserving sylvian dissection. World Neurosurg. 2015; 84(6):2043–52.18. Nishiyama Y, Kanemaru K, Yoshioka H, Hanihara M, Horikoshi T, Kniouchi H. Intracranial pial arteriovenous fistula caused by dural tenting: Case report. Neurol Med Chir (Tokyo). 2014; 54(3):242–4.19. Osada T, Krings T. Intracranial dural arteriovenous fistulas with pial arterial supply. Neurosurgery. 2019; Jan. 84(1):104–15.20. Pabaney AH, Robin AM, Basheer A, Malik G. Surgical management of dural arteriovenous fistula after craniotomy: Case report and review of literature. World Neurosurg. 2016; May. 89:731.21. Paramasivam S, Toma N, Niimi Y, Berenstein A. Development, clinical presentation and endovascular management of congenital intracranial pial arteriovenous fistulas. J Neurointerv Surg. 2013; May. 5(3):184–90.22. Park JS, Lee JM. Acquired dural arteriovenous fistula after cerebellopontine angle meningioma: A case report. Medicine (Baltimore). 2022; Jul. 101(28):e29671.23. Shimizu Y, Tokuda K, Park C. Sphenoid wing dural arteriovenous fistula: A case report and literature review. Surg Neurol Int. 2020; Dec. 11:438.24. Tanaka T, Kato N, Arai T, Hasegawa Y, Abe T. Surgical treatment of a sylvian-middle fossa dural arteriovenous fistula draining into the basal vein of rosenthal with frontotemporal craniotomy. J Stroke Cerebrovasc Dis. 2012; May. 21(4):333–7.25. Vadivelu S, Xin X, Loven T, Restrepo G, Chalif DJ, Setton A. Iatrogenic dural arteriovenous fistula and aneurysmal subarachnoid hemorrhage. Neurosurg Focus. 2012; May. 32(5):e1.26. Yamashita K, Ohe N, Yochimura S, Iwama T. Intracranial pial arteriovenous fistula. Neurol Med Chir (Tokyo). 2007; Dec. 47(12):550–4.27. Yasargil MG. Microneurosurgery. NewYork: Georg Thieme Verlag;1984. p. 5-168, 215-33.28. Yassari R, Jahromi B, Macdonald R. Dural arteriovenous fistula after craniotomy for pilocytic astrocytoma in a patient with protein S deficiency. Surg Neurol. 2002; Jul. 58(1):59–64. discussion 64.29. Yokoyama S, Nakagawa I, Kotsugi M, Wajima D, Wada T, Kichikawa K, et al. Dural arteriovenous fistula arising after intracranial surgery in posterior fossa of nondominant sinus: Two cases and literature review. Asian J Neurosurg. 2019; Apr. 14(2):602–6.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Borden Type I Sigmoid Sinus Dural Arteriovenous Fistula Presenting as Subarachnoid Hemorrhage from a Feeding Artery Aneurysm of the Anterior Inferior Cerebellar Artery: A Case Report
- Cortical versus Pial Venous Drainage in Dural Arteriovenous Fistula
- Successful Treatment of Intracranial Small Pial Single-Channel Arteriovenous Fistula Using N-butyl Cyanoacrylate: Report of 2 Cases
- Embolization of Cerebral Pial Arteriovenous Fistula Under Balloon-assisted Flow Control Using NBCA: a Case Report
- A Case of Mixed Pial and Dural Arteriovenous Malformation in the Left Frontal Convexity