Ann Rehabil Med.
2023 Oct;47(5):337-347. 10.5535/arm.23101.
Sarcopenic Dysphagia and Simplified Rehabilitation Nutrition Care Process: An Update
- Affiliations
-
- 1Department of Rehabilitation Medicine, Tokyo Women’s Medical University Hospital, Tokyo, Japan
- KMID: 2548393
- DOI: http://doi.org/10.5535/arm.23101
Abstract
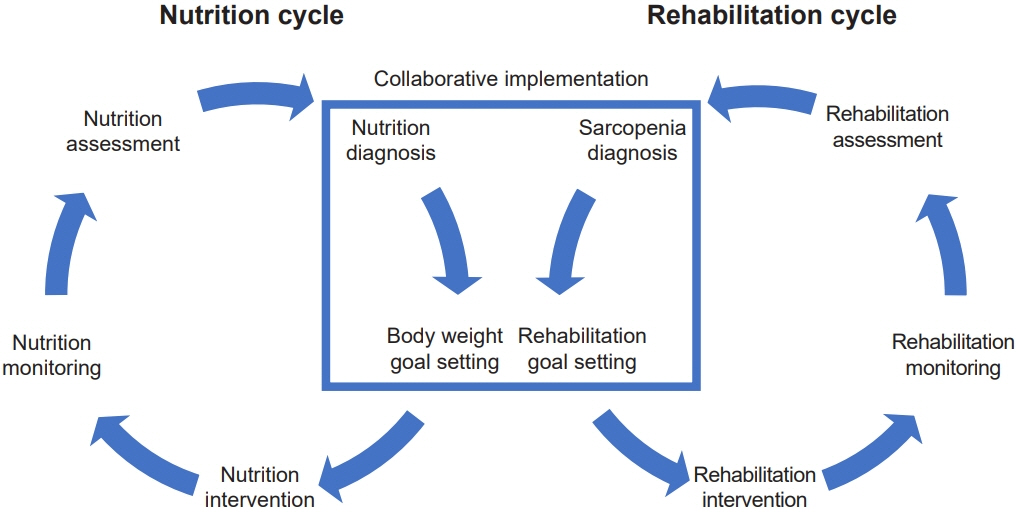
- Sarcopenic dysphagia is characterized by weakness of swallowing-related muscles associated with whole-body sarcopenia. As the number of patients with sarcopenia increases with the aging of the world, the number of patients with sarcopenic dysphagia is also increasing. The prevalence of sarcopenic dysphagia is high in the institutionalized older people and in patients hospitalized for pneumonia with dysphagia in acute care hospitals. Prevention, early detection and intervention of sarcopenic dysphagia with rehabilitation nutrition are essential. The diagnosis of sarcopenic dysphagia is based on skeletal and swallowing muscle strength and muscle mass. A reliable and validated diagnostic algorithm for sarcopenic dysphagia is used. Sarcopenic dysphagia is associated with malnutrition, which leads to mortality and Activities of Daily Living (ADL) decline. The rehabilitation nutrition approach improves swallowing function, nutrition status, and ADL. A combination of aggressive nutrition therapy to improve nutrition status, dysphagia rehabilitation, physical therapy, and other interventions can be effective for sarcopenic dysphagia. The rehabilitation nutrition care process is used to assess and problem solve the patient’s pathology, sarcopenia, and nutrition status. The simplified rehabilitation nutrition care process consists of a nutrition cycle and a rehabilitation cycle, each with five steps: assessment, diagnosis, goal setting, intervention, and monitoring. Nutrition professionals and teams implement the nutrition cycle. Rehabilitation professionals and teams implement the rehabilitation cycle. Both cycles should be done simultaneously. The nutrition diagnosis of undernutrition, overnutrition/obesity, sarcopenia, and goal setting of rehabilitation and body weight are implemented collaboratively.
Keyword
Figure
Reference
-
1. Kitamura A, Seino S, Abe T, Nofuji Y, Yokoyama Y, Amano H, et al. Sarcopenia: prevalence, associated factors, and the risk of mortality and disability in Japanese older adults. J Cachexia Sarcopenia Muscle. 2021; 12:30–8.
Article2. United Nations. World population prospects 2022: summary of results [Internet]. United Nations; 2022 [cited 2023 Jun 12]. Available from: https://www.un.org/development/desa/pd/content/World-Population-Prospects-2022.3. Wen Z, Gu J, Chen R, Wang Q, Ding N, Meng L, et al. Handgrip strength and muscle quality: results from the national health and nutrition examination survey database. J Clin Med. 2023; 12:3184.
Article4. Dodds RM, Syddall HE, Cooper R, Kuh D, Cooper C, Sayer AA. Global variation in grip strength: a systematic review and meta-analysis of normative data. Age Ageing. 2016; 45:209–16.
Article5. Yamada M, Moriguch Y, Mitani T, Aoyama T, Arai H. Age-dependent changes in skeletal muscle mass and visceral fat area in Japanese adults from 40 to 79 years-of-age. Geriatr Gerontol Int. 2014; 14 Suppl 1:8–14.6. Keller K, Engelhardt M. Strength and muscle mass loss with aging process. Age and strength loss. Muscles Ligaments Tendons J. 2014; 3:346–50.
Article7. Ho IS, Azcoaga-Lorenzo A, Akbari A, Davies J, Hodgins P, Khunti K, et al. Variation in the estimated prevalence of multimorbidity: systematic review and meta-analysis of 193 international studies. BMJ Open. 2022; 12:e057017.
Article8. Prokopidis K, Giannos P, Reginster JY, Bruyere O, Petrovic M, Cherubini A, et al. Sarcopenia is associated with a greater risk of polypharmacy and number of medications: a systematic review and meta-analysis. J Cachexia Sarcopenia Muscle. 2023; 14:671–83.
Article9. Cruz-Jentoft AJ, Sayer AA. Sarcopenia. Lancet. 2019; 393:2636–46. Erratum in: Lancet 2019;393:2590.
Article10. Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019; 48:16–31. Erratum in: Age Ageing 2019;48:601.
Article11. Nagano A, Wakabayashi H, Maeda K, Kokura Y, Miyazaki S, Mori T, et al. Respiratory sarcopenia and sarcopenic respiratory disability: concepts, diagnosis, and treatment. J Nutr Health Aging. 2021; 25:507–15.
Article12. Thiyagalingam S, Kulinski AE, Thorsteinsdottir B, Shindelar KL, Takahashi PY. Dysphagia in older adults. Mayo Clin Proc. 2021; 96:488–97.
Article13. Fujishima I, Fujiu-Kurachi M, Arai H, Hyodo M, Kagaya H, Maeda K, et al. Sarcopenia and dysphagia: position paper by four professional organizations. Geriatr Gerontol Int. 2019; 19:91–7.
Article14. Yamaguchi K, Nakagawa K, Yoshimi K, Ariya C, Nakane A, Ishii M, et al. Association between characteristics of swallowing-related muscles and trunk muscle mass. Sci Rep. 2023; 13:7814.
Article15. Nakao Y, Uchiyama Y, Honda K, Yamashita T, Saito S, Domen K. Age-related composition changes in swallowing-related muscles: a Dixon MRI study. Aging Clin Exp Res. 2021; 33:3205–13.
Article16. Rech RS, de Goulart BNG, Dos Santos KW, Marcolino MAZ, Hilgert JB. Frequency and associated factors for swallowing impairment in community-dwelling older persons: a systematic review and meta-analysis. Aging Clin Exp Res. 2022; 34:2945–61.
Article17. Rajati F, Ahmadi N, Naghibzadeh ZA, Kazeminia M. The global prevalence of oropharyngeal dysphagia in different populations: a systematic review and meta-analysis. J Transl Med. 2022; 20:175.
Article18. Tagliaferri S, Lauretani F, Pelá G, Meschi T, Maggio M. The risk of dysphagia is associated with malnutrition and poor functional outcomes in a large population of outpatient older individuals. Clin Nutr. 2019; 38:2684–9.
Article19. Blanař V, Hödl M, Lohrmann C, Amir Y, Eglseer D. Dysphagia and factors associated with malnutrition risk: a 5-year multicentre study. J Adv Nurs. 2019; 75:3566–76.
Article20. Almirall J, Rofes L, Serra-Prat M, Icart R, Palomera E, Arreola V, et al. Oropharyngeal dysphagia is a risk factor for community-acquired pneumonia in the elderly. Eur Respir J. 2013; 41:923–8.
Article21. Patel DA, Krishnaswami S, Steger E, Conover E, Vaezi MF, Ciucci MR, et al. Economic and survival burden of dysphagia among inpatients in the United States. Dis Esophagus. 2018; 31:1–7.
Article22. Yang RY, Yang AY, Chen YC, Lee SD, Lee SH, Chen JW. Association between dysphagia and frailty in older adults: a systematic review and meta-analysis. Nutrients. 2022; 14:1812.
Article23. Sakai K, Nakayama E, Yoneoka D, Sakata N, Iijima K, Tanaka T, et al. Association of oral function and dysphagia with frailty and sarcopenia in community-dwelling older adults: a systematic review and meta-analysis. Cells. 2022; 11:2199.
Article24. Maeda K, Takaki M, Akagi J. Decreased skeletal muscle mass and risk factors of sarcopenic dysphagia: a prospective observational cohort study. J Gerontol A Biol Sci Med Sci. 2017; 72:1290–4.
Article25. Wakabayashi H, Kishima M, Itoda M, Fujishima I, Kunieda K, Ohno T, et al. Diagnosis and treatment of sarcopenic dysphagia: a scoping review. Dysphagia. 2021; 36:523–31.
Article26. Nagano A, Nishioka S, Wakabayashi H. Rehabilitation nutrition for iatrogenic sarcopenia and sarcopenic dysphagia. J Nutr Health Aging. 2019; 23:256–65.
Article27. Wakabayashi H. Rehabilitation nutrition in general and family medicine. J Gen Fam Med. 2017; 18:153–4.
Article28. Nishioka S, Aragane H, Suzuki N, Yoshimura Y, Fujiwara D, Mori T, et al. Clinical practice guidelines for rehabilitation nutrition in cerebrovascular disease, hip fracture, cancer, and acute illness: 2020 update. Clin Nutr ESPEN. 2021; 43:90–103.
Article29. Wakabayashi H, Yoshimura Y, Maeda K, Fujiwara D, Nishioka S, Nagano A. Goal setting for nutrition and body weight in rehabilitation nutrition: position paper by the Japanese Association of Rehabilitation Nutrition (secondary publication). J Gen Fam Med. 2021; 23:77–86.30. Inoue T, Iida Y, Takahashi K, Shirado K, Nagano F, Miyazaki S, et al. Nutrition and physical therapy: a position paper by the physical therapist section of the Japanese Association of Rehabilitation Nutrition (secondary publication). JMA J. 2022; 5:243–51.
Article31. Sato S, Miyazaki S, Tamaki A, Yoshimura Y, Arai H, Fujiwara D, et al. Respiratory sarcopenia: a position paper by four professional organizations. Geriatr Gerontol Int. 2023; 23:5–15.
Article32. Morisaki N. Relationship between swallowing functions and health-related quality of life among community-dwelling dependent older individuals. Jpn J Nurs Sci. 2017; 14:353–63.
Article33. Khanagar SB, Al-Ehaideb A, Shivanna MM, Ul Haq I, Al Kheraif AA, Naik S, et al. Age-related oral changes and their impact on oral health-related quality of life among frail elderly population: a review. J Contemp Dent Pract. 2020; 21:1298–303.
Article34. Veronese N, Koyanagi A, Cereda E, Maggi S, Barbagallo M, Dominguez LJ, et al. Sarcopenia reduces quality of life in the long-term: longitudinal analyses from the English longitudinal study of ageing. Eur Geriatr Med. 2022; 13:633–9.
Article35. Nakahara S, Takasaki M, Abe S, Kakitani C, Nishioka S, Wakabayashi H, et al. Aggressive nutrition therapy in malnutrition and sarcopenia. Nutrition. 2021; 84:111109.
Article36. Wakabayashi H. Presbyphagia and sarcopenic dysphagia: association between aging, sarcopenia, and deglutition disorders. J Frailty Aging. 2014; 3:97–103.
Article37. Kokura Y, Nishioka S, Maeda K, Wakabayashi H. Ultrasound utilized by registered dietitians for body composition measurement, nutritional assessment, and nutritional management. Clin Nutr ESPEN. 2023; 57:173–80.
Article38. Inamoto Y, González-Fernández M, Saitoh E. 3D-CT evaluation of swallowing: metrics of the swallowing response using swallowing CT. Dysphagia. 2022; 37:237–49.
Article39. Nakao Y, Yamashita T, Honda K, Katsuura T, Hama Y, Nakamura Y, et al. Association among age-related tongue muscle abnormality, tongue pressure, and presbyphagia: a 3D MRI study. Dysphagia. 2021; 36:483–91.
Article40. Ogawa N, Mori T, Fujishima I, Wakabayashi H, Itoda M, Kunieda K, et al. Ultrasonography to measure swallowing muscle mass and quality in older patients with sarcopenic dysphagia. J Am Med Dir Assoc. 2018; 19:516–22.
Article41. Allen JE, Clunie GM, Winiker K. Ultrasound: an emerging modality for the dysphagia assessment toolkit? Curr Opin Otolaryngol Head Neck Surg. 2021; 29:213–8.
Article42. Mori T, Fujishima I, Wakabayashi H, Oshima F, Itoda M, Kunieda K, et al. Development, reliability, and validity of a diagnostic algorithm for sarcopenic dysphagia. JCSM Clin Rep. 2017; 2:1–10.
Article43. Chen LK, Woo J, Assantachai P, Auyeung TW, Chou MY, Iijima K, et al. Asian Working Group for Sarcopenia: 2019 consensus update on sarcopenia diagnosis and treatment. J Am Med Dir Assoc. 2020; 21:300–7.e2.
Article44. Mori T, Wakabayashi H, Ogawa N, Fujishima I, Oshima F, Itoda M, et al. The mass of geniohyoid muscle is associated with maximum tongue pressure and tongue area in patients with sarcopenic dysphagia. J Nutr Health Aging. 2021; 25:356–60.
Article45. Machida N, Tohara H, Hara K, Kumakura A, Wakasugi Y, Nakane A, et al. Effects of aging and sarcopenia on tongue pressure and jaw-opening force. Geriatr Gerontol Int. 2017; 17:295–301.
Article46. Murakami T, Kamide N, Ando M, Hata W, Sakamoto M. Association between tongue pressure and skeletal muscle mass and muscle function in community-dwelling older people without sarcopenia. Eur Geriatr Med. 2022; 13:649–53.
Article47. Shimizu A, Maeda K, Wakabayashi H, Nishioka S, Ohno T, Nomoto A, et al. Sarcopenic dysphagia with low tongue pressure is associated with worsening of swallowing, nutritional status, and activities of daily living. J Nutr Health Aging. 2021; 25:883–8.
Article48. Shimizu A, Fujishima I, Maeda K, Wakabayashi H, Nishioka S, Ohno T, et al. Effect of low tongue pressure on nutritional status and improvement of swallowing function in sarcopenic dysphagia. Nutrition. 2021; 90:111295.
Article49. Chang KV, Wu WT, Chen LR, Wang HI, Wang TG, Han DS. Suboptimal tongue pressure is associated with risk of malnutrition in community-dwelling older individuals. Nutrients. 2021; 13:1821.
Article50. Kunieda K, Fujishima I, Wakabayashi H, Ohno T, Shigematsu T, Itoda M, et al. Relationship between tongue pressure and pharyngeal function assessed using high-resolution manometry in older dysphagia patients with sarcopenia: a pilot study. Dysphagia. 2021; 36:33–40.
Article51. Kaji A, Hashimoto Y, Kobayashi Y, Sakai R, Okamura T, Miki A, et al. Sarcopenia is associated with tongue pressure in older patients with type 2 diabetes: a cross-sectional study of the KAMOGAWA-DM cohort study. Geriatr Gerontol Int. 2019; 19:153–8.
Article52. Maeda K, Akagi J. Decreased tongue pressure is associated with sarcopenia and sarcopenic dysphagia in the elderly. Dysphagia. 2015; 30:80–7. Erratum in: Dysphagia 2015;30:88.
Article53. Kishimoto H, Wakabayashi H, Nishioka S, Momosaki R. Discriminative evaluation of sarcopenic dysphagia using handgrip strength or calf circumference in patients with dysphagia using the area under the receiver operating characteristic curve. J Clin Med. 2022; 12:118.
Article54. Togashi S, Wakabayashi H, Ohinata H, Nishioka S, Kokura Y, Momosaki R. Sensitivity and specificity of body mass index for sarcopenic dysphagia diagnosis among patients with dysphagia: a multi-center cross-sectional study. Nutrients. 2022; 14:4494.
Article55. Moncayo-Hernández BA, Herrera-Guerrero JA, Vinazco S, Ocampo-Chaparro JM, Reyes-Ortiz CA. Sarcopenic dysphagia in institutionalised older adults. Endocrinol Diabetes Nutr (Engl Ed). 2021; 68:602–11.
Article56. Wakabayashi H, Takahashi R, Murakami T. The prevalence and prognosis of sarcopenic dysphagia in patients who require dysphagia rehabilitation. J Nutr Health Aging. 2019; 23:84–8.
Article57. Miyauchi N, Nakamura M, Nakamura I, Momosaki R. Effect of early versus delayed mobilization by physical therapists on oral intake in patients with sarcopenic dysphagia after pneumonia. Eur Geriatr Med. 2019; 10:603–7.
Article58. Nagano A, Maeda K, Shimizu A, Nagami S, Takigawa N, Ueshima J, et al. Association of sarcopenic dysphagia with underlying sarcopenia following hip fracture surgery in older women. Nutrients. 2020; 12:1365.
Article59. Maeda K, Ishida Y, Nonogaki T, Shimizu A, Yamanaka Y, Matsuyama R, et al. Development and predictors of sarcopenic dysphagia during hospitalization of older adults. Nutrients. 2019; 12:70.
Article60. Nagai T, Wakabayashi H, Nishioka S, Momosaki R. Functional prognosis in patients with sarcopenic dysphagia: an observational cohort study from the Japanese sarcopenic dysphagia database. Geriatr Gerontol Int. 2022; 22:839–45.
Article61. Abe S, Kokura Y, Maeda K, Nishioka S, Momosaki R, Matsuoka H, et al. Effects of undernutrition on swallowing function and activities of daily living in hospitalized patients: data from the Japanese Sarcopenic Dysphagia Database. Nutrients. 2023; 15:1291.
Article62. Campo-Rivera N, Ocampo-Chaparro JM, Carvajal-Ortiz R, Reyes-Ortiz CA. Sarcopenic dysphagia is associated with mortality in institutionalized older adults. J Am Med Dir Assoc. 2022; 23:1720.e11–7.
Article63. Nishioka S, Wakabayashi H. Interaction between malnutrition and physical disability in older adults: is there a malnutrition-disability cycle? Nutr Rev. 2023; 81:191–205.
Article64. Mori T, Wakabayashi H, Kishima M, Itoda M, Fujishima I, Kunieda K, et al. Association between inflammation and functional outcome in patients with sarcopenic dysphagia. J Nutr Health Aging. 2022; 26:400–6.
Article65. Nishioka S, Nakahara S, Takasaki M, Shiohama N, Kokura Y, Suzuki T, et al. The concept of aggressive nutrition therapy and clinical indication: a position paper. Clin Nutr ESPEN. 2022; 52:322–30.66. Shimizu A, Fujishima I, Maeda K, Wakabayashi H, Nishioka S, Ohno T, et al. Nutritional management enhances the recovery of swallowing ability in older patients with sarcopenic dysphagia. Nutrients. 2021; 13:596.
Article67. Kagaya H, Inamoto Y. Possible rehabilitation procedures to treat sarcopenic dysphagia. Nutrients. 2022; 14:778.
Article68. Nagano A, Maeda K, Koike M, Murotani K, Ueshima J, Shimizu A, et al. Effects of physical rehabilitation and nutritional intake management on improvement in tongue strength in sarcopenic patients. Nutrients. 2020; 12:3104.
Article69. Wakabayashi H. Hospital-associated sarcopenia, acute sarcopenia, and iatrogenic sarcopenia: prevention of sarcopenia during hospitalization. J Gen Fam Med. 2023; 24:146–7.
Article70. Feng HY, Zhang PP, Wang XW. Presbyphagia: dysphagia in the elderly. World J Clin Cases. 2023; 11:2363–73.
Article71. Yiğman ZA, Umay E, Cankurtaran D, Güzel Ş. Swallowing difficulty in the older adults: presbyphagia or dysphagia with sarcopenia? Int J Rehabil Res. 2021; 44:336–42.
Article72. Labeit B, Muhle P, von Itter J, Slavik J, Wollbrink A, Sporns P, et al. Clinical determinants and neural correlates of presbyphagia in community-dwelling older adults. Front Aging Neurosci. 2022; 14:912691.
Article73. Nienstedt JC, Müller F, Rösler A, Pflug C. Presbyphagia diagnostics using M-mode ultrasound: changes in the tongue movement pattern. Dysphagia. 2020; 35:696–701.
Article74. Namasivayam-MacDonald AM, Riquelme LF. Presbyphagia to dysphagia: multiple perspectives and strategies for quality care of older adults. Semin Speech Lang. 2019; 40:227–42.
Article75. de Lima Alvarenga EH, Dall'Oglio GP, Murano EZ, Abrahão M. Continuum theory: presbyphagia to dysphagia? Functional assessment of swallowing in the elderly. Eur Arch Otorhinolaryngol. 2018; 275:443–9.
Article76. Schindler A, Mozzanica F, Monzani A, Ceriani E, Atac M, Jukic-Peladic N, et al. Reliability and validity of the Italian Eating Assessment Tool. Ann Otol Rhinol Laryngol. 2013; 122:717–24.
Article77. Cheney DM, Siddiqui MT, Litts JK, Kuhn MA, Belafsky PC. The ability of the 10-Item Eating Assessment Tool (EAT-10) to predict aspiration risk in persons with dysphagia. Ann Otol Rhinol Laryngol. 2015; 124:351–4.
Article78. Wakabayashi H, Matsushima M. Dysphagia assessed by the 10-Item Eating Assessment Tool is associated with nutritional status and activities of daily living in elderly individuals requiring long-term care. J Nutr Health Aging. 2016; 20:22–7.
Article79. Izaola O, Gómez Hoyos E, López JJ, Ortola A, Torres B, Primo D, et al. The 10-Item Eating Assessment Tool is associated with nutritional status, mortality and hospital stay in elderly individuals requiring hospitalization with acute diseases. Nutr Hosp. 2018; 35:827–32.80. Igarashi K, Kikutani T, Tamura F. Survey of suspected dysphagia prevalence in home-dwelling older people using the 10-Item Eating Assessment Tool (EAT-10). PLoS One. 2019; 14:e0211040.
Article81. Ko D, Oh J, Joo S, Park JY, Cho MS. Dietary habits, food product selection attributes, nutritional status, and depression in middle-aged and older adults with dysphagia. Nutrients. 2022; 14:4045.
Article82. Mizuno S, Wakabayashi H, Wada F. Rehabilitation nutrition for individuals with frailty, disability, sarcopenic dysphagia, or sarcopenic respiratory disability. Curr Opin Clin Nutr Metab Care. 2022; 25:29–36.
Article83. Wakabayashi H. Positive psychology and rehabilitation nutrition. J Gen Fam Med. 2022; 23:293–94.
Article84. Wakabayashi H, Maeda K, Momosaki R, Kokura Y, Yoshimura Y, Fujiwara D, et al. Diagnostic reasoning in rehabilitation nutrition: position paper by the Japanese Association of Rehabilitation Nutrition (secondary publication). J Gen Fam Med. 2022; 23:205–16.
Article85. Brush JE Jr, Sherbino J, Norman GR. How expert clinicians intuitively recognize a medical diagnosis. Am J Med. 2017; 130:629–34.
Article86. Corazza GR, Lenti MV, Howdle PD. Diagnostic reasoning in internal medicine: a practical reappraisal. Intern Emerg Med. 2021; 16:273–9.
Article87. Bovend'Eerdt TJ, Botell RE, Wade DT. Writing SMART rehabilitation goals and achieving goal attainment scaling: a practical guide. Clin Rehabil. 2009; 23:352–61. Erratum in: Clin Rehabil 2010;24:382.88. Chan CH, Conley M, Reeves MM, Campbell KL, Kelly JT. Evaluating the impact of goal setting on improving diet quality in chronic kidney disease. Front Nutr. 2021; 8:627753.
Article89. Barrett KV, Savage PD, Ades PA. Effects of behavioral weight loss and weight loss goal setting in cardiac rehabilitation. J Cardiopulm Rehabil Prev. 2020; 40:383–7.
Article90. Yoshimura Y, Wakabayashi H, Momosaki R, Nagano F, Bise T, Shimazu S, et al. Stored energy increases body weight and skeletal muscle mass in older, underweight patients after stroke. Nutrients. 2021; 13:3274.
Article91. Cederholm T, Jensen GL, Correia MITD, Gonzalez MC, Fukushima R, Higashiguchi T, et al. GLIM criteria for the diagnosis of malnutrition - a consensus report from the global clinical nutrition community. J Cachexia Sarcopenia Muscle. 2019; 10:207–17.
Article92. Wakabayashi H, Kakehi S, Kishima M, Itoda M, Nishioka S, Momosaki R. Impact of registered dietitian and dental hygienist involvement on functional outcomes in patients with dysphagia: triad of rehabilitation, nutrition, and oral management. Eur Geriatr Med. 2023. doi: 10.1007/s41999-023-00833-7 [Epub ahead of print].
Article93. Abu-Ghanem S, Graf A, Govind J. Diagnosis of sarcopenic dysphagia in the elderly: critical review and future perspectives. Dysphagia. 2022; 37:1093–102.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Rehabilitation in a Patient with Sarcopenic Dysphagia on Venovenous Extracorporeal Membrane Oxygenation Support Following COVID-19 Infection: A Case Report
- Interventions for Sarcopenic Dysphagia: A Systematic Review
- Meal Service and Nutritional Management for Dysphagia: A Nationwide Hospital Survey
- Rehabilitation Techniques for Dysphagia
- Update of Guidelines: International Dysphagia Diet Standardization Initiative 2019