Restor Dent Endod.
2022 Nov;47(4):e35. 10.5395/rde.2022.47.e35.
Endodontic micro-resurgery and guided tissue regeneration of a periapical cyst associated to recurrent root perforation: a case report
- Affiliations
-
- 1Department of Endodontics, Cayetano Heredia Peruvian University (UPCH), Lima, Peru
- 2Department of Restorative Dentistry, Araraquara School of Dentistry, São Paulo State University (UNESP), Araraquara, SP, Brazil
- 3Academic Department of Stomatological Clinic, Cayetano Heredia Peruvian University (UPCH), Lima, Peru
- KMID: 2548139
- DOI: http://doi.org/10.5395/rde.2022.47.e35
Abstract
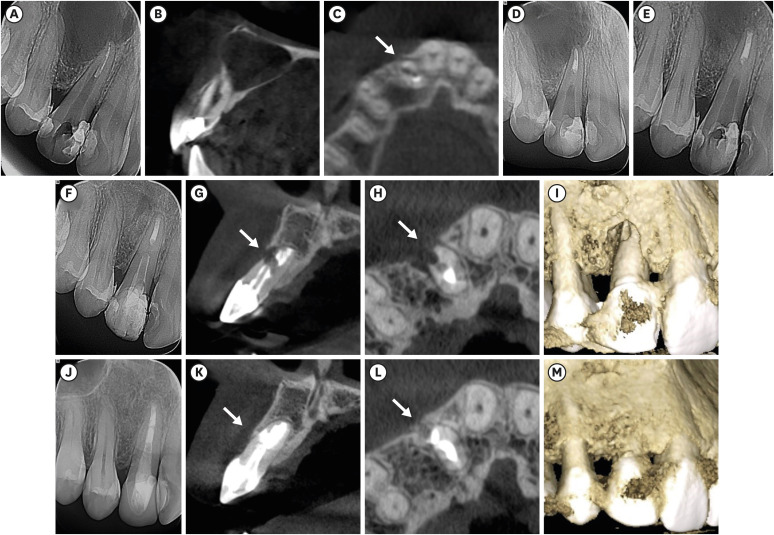
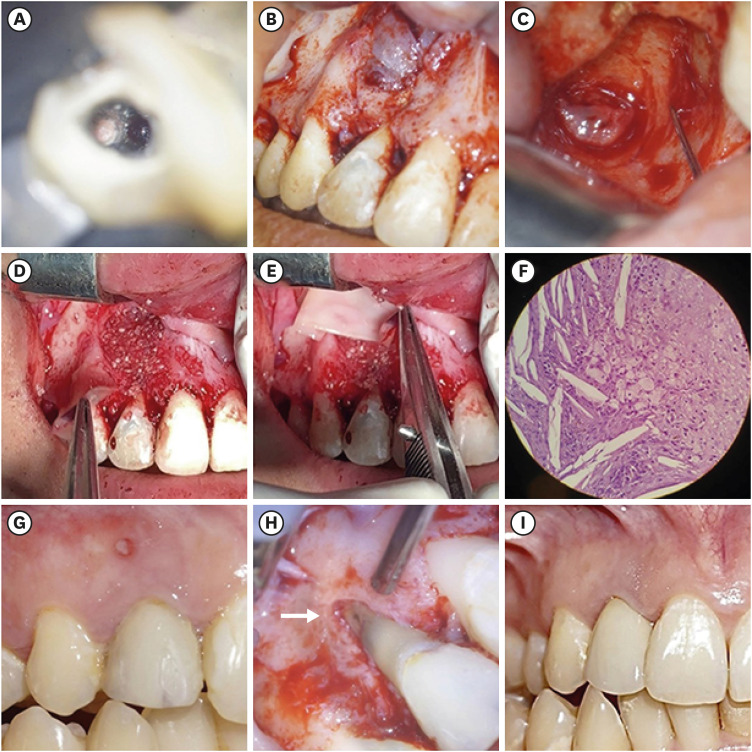
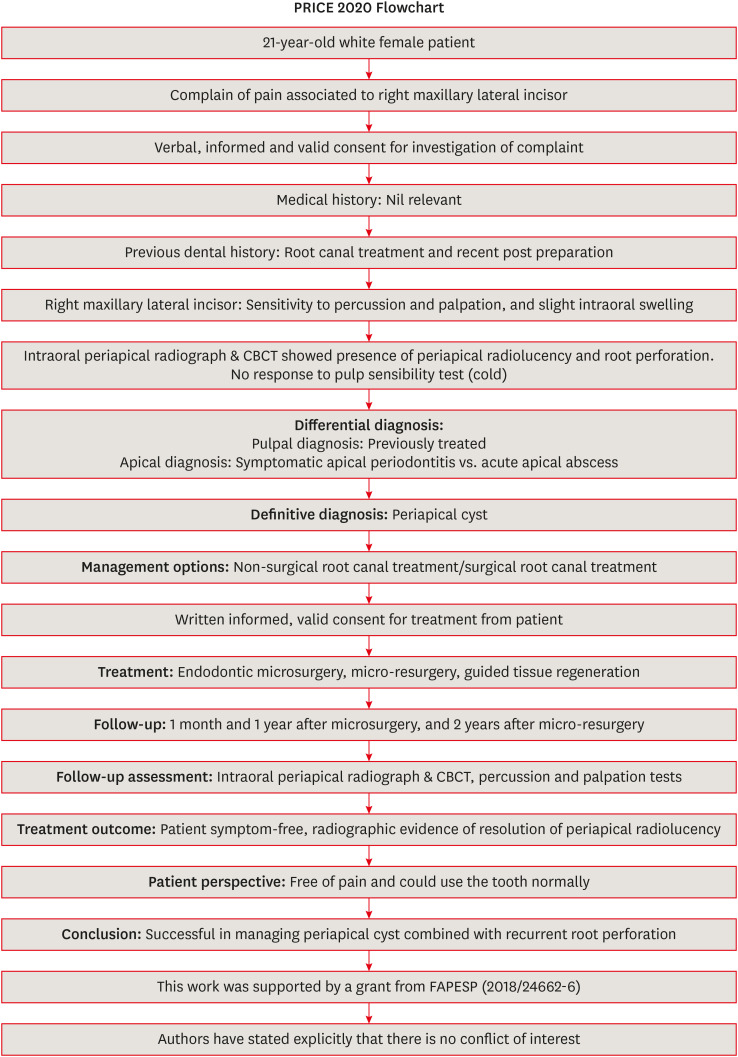
- Although the success rates of microsurgery and micro-resurgery are very high, the influence of a recurrent perforation combined with radicular cyst remains unclear. A 21-year-old white female patient had a history of root perforation in a previously treated right maxillary lateral incisor. Analysis using cone-beam computed tomography (CBCT) revealed an extensive and well-defined periapical radiolucency, involving the buccal and palatal bone plate. The perforation was sealed with bioceramic material (Biodentine) in the pre-surgical phase. In the surgical phase, guided tissue regeneration (GTR) was performed by combining xenograft (lyophilized bovine bone) and autologous platelet-rich fibrin applied to the bone defect. The root-end preparation was done using an ultrasonic tip. The retrograde filling was performed using a bioceramic material (Biodentine). Histopathological analysis confirmed a radicular cyst. The patient returned to her referring practitioner to continue the restorative procedures. CBCT analysis after 1-year recall revealed another perforation in the same place as the first intervention, ultimately treated by micro-resurgery using the same protocol with GTR, and a bioceramic material (MTA Angelus). The 2-year recall showed healing and bone neoformation. In conclusion, endodontic micro-resurgery with GTR showed long-term favorable results when a radicular cyst and a recurrent perforation compromised the success.
Figure
Reference
-
1. Ricucci D, Siqueira JF Jr, Lopes WS, Vieira AR, Rôças IN. Extraradicular infection as the cause of persistent symptoms: a case series. J Endod. 2015; 41:265–273. PMID: 25282379.
Article2. Nair PN. New perspectives on radicular cysts: Do they heal? Int Endod J. 1998; 31:155–160. PMID: 10321160.
Article3. Floratos S, Kim S. Modern endodontic microsurgery concepts: a clinical update. Dent Clin North Am. 2017; 61:81–91. PMID: 27912820.4. Niemczyk SP. Essentials of endodontic microsurgery. Dent Clin North Am. 2010; 54:375–399. PMID: 20433983.
Article5. Setzer FC, Kohli MR, Shah SB, Karabucak B, Kim S. Outcome of endodontic surgery: a meta-analysis of the literature--Part 2: comparison of endodontic microsurgical techniques with and without the use of higher magnification. J Endod. 2012; 38:1–10. PMID: 22152611.
Article6. Kim D, Kim S, Song M, Kang DR, Kohli MR, Kim E. Outcome of endodontic micro-resurgery: retrospective study based on propensity score–matched survival analysis. J Endod. 2018; 44:1632–1640. PMID: 30243664.
Article7. Song M, Shin SJ, Kim E. Outcomes of endodontic micro-resurgery: a prospective clinical study. J Endod. 2011; 37:316–320. PMID: 21329814.
Article8. Yoshikawa G, Murashima Y, Wadachi R, Sawada N, Suda H. Guided bone regeneration (GBR) using membranes and calcium sulphate after apicectomy: a comparative histomorphometrical study. Int Endod J. 2002; 35:255–263. PMID: 11985677.
Article9. Lin L, Chen MY, Ricucci D, Rosenberg PA. Guided tissue regeneration in periapical surgery. J Endod. 2010; 36:618–625. PMID: 20307733.
Article10. Rankow HJ, Krasner PR. Endodontic applications of guided tissue regeneration in endodontic surgery. Oral Health. 1996; 86:33–35.
Article11. Tsesis I, Fuss Z. Diagnosis and treatment of accidental root perforations. Endod Topics. 2006; 13:95–107.
Article12. Estrela C, Decurcio DA, Rossi-Fedele G, Silva JA, Guedes OA, Borges ÁH. Root perforations: a review of diagnosis, prognosis and materials. Braz Oral Res. 2018; 32:e73. PMID: 30365614.
Article13. Nakata TT, Bae KS, Baumgartner JC. Perforation repair comparing mineral trioxide aggregate and amalgam using an anaerobic bacterial leakage model. J Endod. 1998; 24:184–186. PMID: 9558584.
Article14. Fuss Z, Trope M. Root perforations: classification and treatment choices based on prognostic factors. Endod Dent Traumatol. 1996; 12:255–264. PMID: 9206372.
Article15. Silberman JJ, Moldauer BI, Torres J, Gallardo C, Sanabria-Liviac D. Palatal root surgery of a maxillary molar using a piezosurgery transantral approach with simultaneous sinus lift grafting: a case report. Int Endod J. 2021; 54:464–475. PMID: 33012051.
Article16. Nagendrababu V, Chong BS, McCabe P, Shah PK, Priya E, Jayaraman J, Pulikkotil SJ, Setzer FC, Sunde PT, Dummer PM. PRICE 2020 guidelines for reporting case reports in endodontics: a consensus-based development. Int Endod J. 2020; 53:619–626. PMID: 32090342.
Article17. Pallarés-Serrano A, Glera-Suarez P, Tarazona-Alvarez B, Peñarrocha-Diago M, Peñarrocha-Diago M, Peñarrocha-Oltra D. Prognostic factors after endodontic microsurgery: a retrospective study of 111 cases with 5 to 9 years of follow-up. J Endod. 2021; 47:397–403. PMID: 33271177.
Article18. Çalışkan MK, Kaval ME, Tekin U, Ünal T. Radiographic and histological evaluation of persistent periapical lesions associated with endodontic failures after apical microsurgery. Int Endod J. 2016; 49:1011–1019. PMID: 26384024.
Article19. Trasatti C, Spears R, Gutmann JL, Opperman LA. Increased Tgf-β1 production by rat osteoblasts in the presence of PepGen P-15 in vitro . J Endod. 2004; 30:213–217. PMID: 15085048.
Article20. Bashutski JD, Wang HL. Periodontal and endodontic regeneration. J Endod. 2009; 35:321–328. PMID: 19249588.
Article21. Taschieri S, Del Fabbro M, Testori T, Saita M, Weinstein R. Efficacy of guided tissue regeneration in the management of through-and-through lesions following surgical endodontics: a preliminary study. Int J Periodontics Restorative Dent. 2008; 28:265–271. PMID: 18605602.22. Taschieri S, Del Fabbro M, Testori T, Weinstein R. Efficacy of xenogeneic bone grafting with guided tissue regeneration in the management of bone defects after surgical endodontics. J Oral Maxillofac Surg. 2007; 65:1121–1127. PMID: 17517295.
Article23. Dietrich T, Zunker P, Dietrich D, Bernimoulin JP. Periapical and periodontal healing after osseous grafting and guided tissue regeneration treatment of apicomarginal defects in periradicular surgery: results after 12 months. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003; 95:474–482. PMID: 12686934.
Article24. Dhiman M, Kumar S, Duhan J, Sangwan P, Tewari S. Effect of platelet-rich fibrin on healing of apicomarginal defects: a randomized controlled trial. J Endod. 2015; 41:985–991. PMID: 25963290.
Article25. Karan NB, Aricioğlu B. Assessment of bone healing after mineral trioxide aggregate and platelet-rich fibrin application in periapical lesions using cone-beam computed tomographic imaging. Clin Oral Investig. 2020; 24:1065–1072.
Article26. Christensen CE, McNeal SF, Eleazer P. Effect of lowering the pH of sodium hypochlorite on dissolving tissue in vitro . J Endod. 2008; 34:449–452. PMID: 18358894.
Article27. Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, Gogly B. Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part III: leucocyte activation: a new feature for platelet concentrates? Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006; 101:e51–e55. PMID: 16504851.
Article28. Soto-Peñaloza D, Peñarrocha-Diago M, Cervera-Ballester J, Peñarrocha-Diago M, Tarazona-Alvarez B, Peñarrocha-Oltra D. Pain and quality of life after endodontic surgery with or without advanced platelet-rich fibrin membrane application: a randomized clinical trial. Clin Oral Investig. 2020; 24:1727–1738.
Article29. Makhlouf M, Zogheib C, Makhlouf AC, Kaloustian MK, El Hachem C, Habib M. Sealing ability of calcium silicate-based materials in the repair of furcal perforations: a laboratory comparative study. J Contemp Dent Pract. 2020; 21:1091–1097. PMID: 33686028.
Article30. da Fonseca TS, Silva GF, Guerreiro-Tanomaru JM, Delfino MM, Sasso-Cerri E, Tanomaru-Filho M, Cerri PS. Biodentine and MTA modulate immunoinflammatory response favoring bone formation in sealing of furcation perforations in rat molars. Clin Oral Investig. 2019; 23:1237–1252.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Guided tissue regeneration therapy after root canal therapy for long standing periodontal-endodontic combined lesion in the mandibular anterior area: case report
- Non-surgical treatment of large periapical lesions
- Leukocyte platelet-rich fibrin in endodontic microsurgery: a report of 2 cases
- Endodontic treatment enhances the regenerative potential of teeth with advanced periodontal disease with secondary endodontic involvement
- Progression of periapical cystic lesion after incomplete endodontic treatment