Anat Cell Biol.
2023 Sep;56(3):350-359. 10.5115/acb.23.015.
An anatomical investigation of the suboccipitaland inferior suboccipital triangles
- Affiliations
-
- 1Department of Anatomy, Faculty of Medicine, University of Pretoria, Pretoria, South Africa
- KMID: 2546463
- DOI: http://doi.org/10.5115/acb.23.015
Abstract
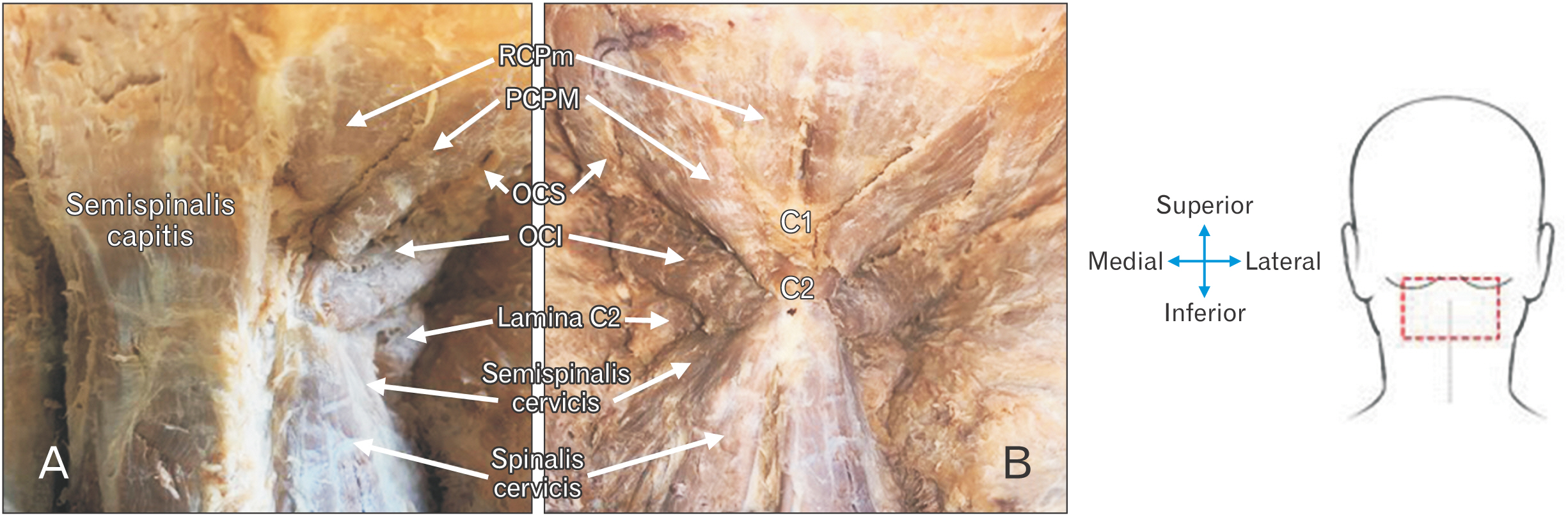
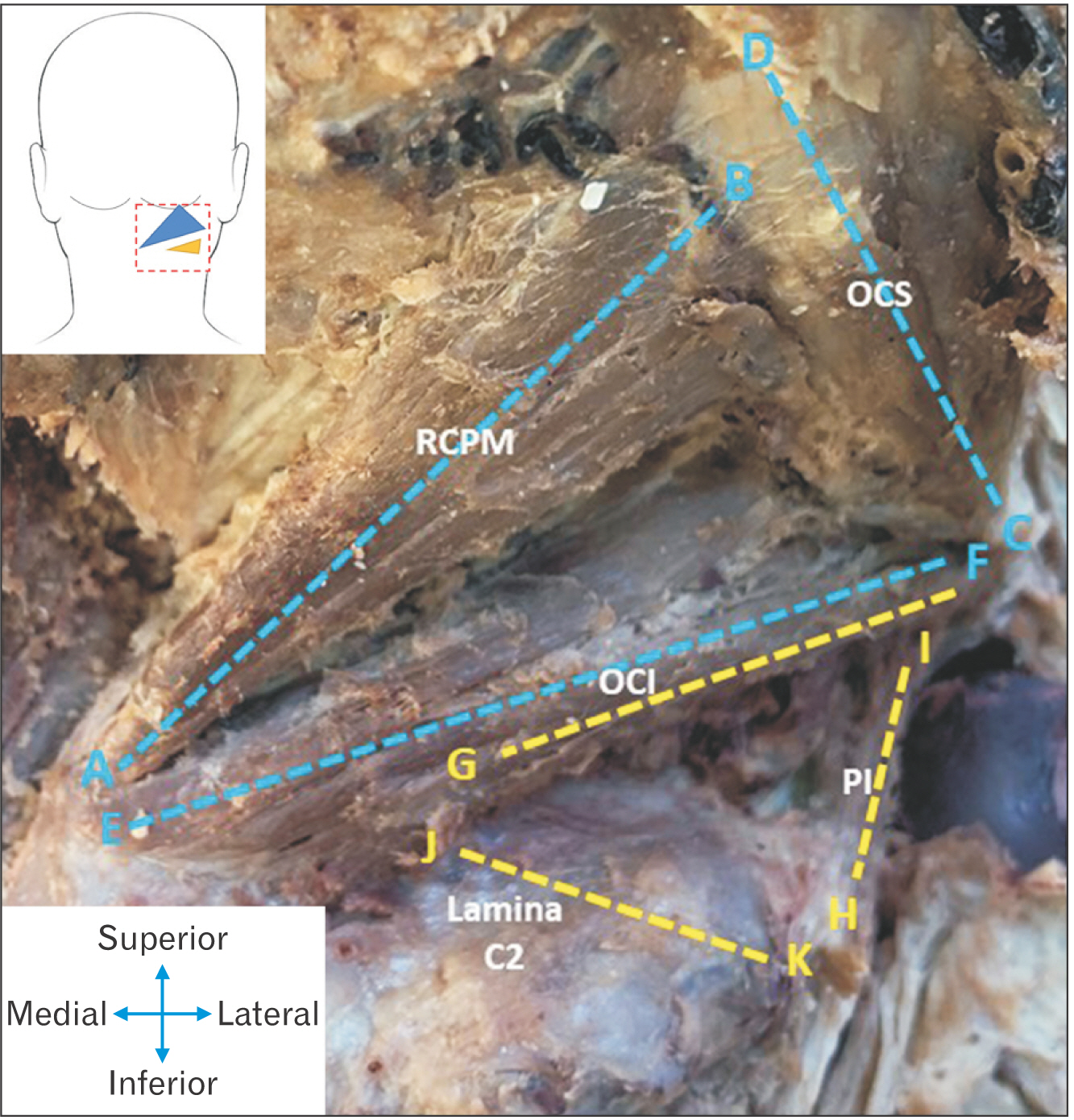
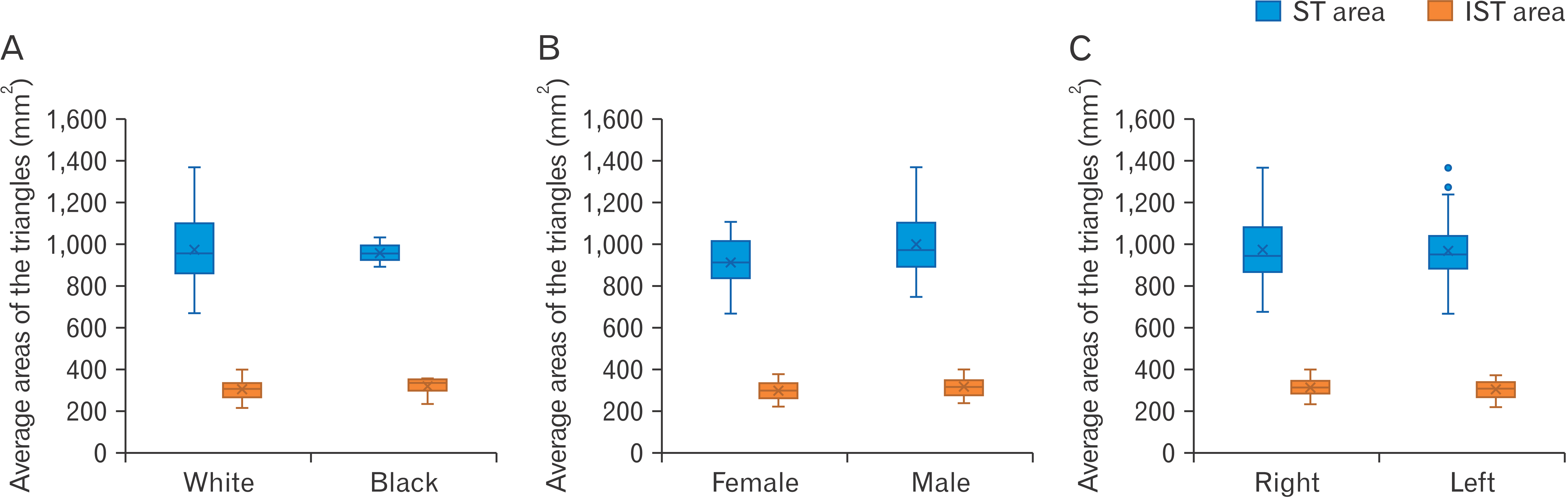
- The suboccipital triangle (ST) is a clinically relevant landmark in the posterior aspect of the neck and is used to locate and mobilize the horizontal segment of the third part of the vertebral artery before it enters the cranium. Unfortunately, this space is not always a viable option for vertebral artery exposition, and consequently a novel triangle, the inferior suboccipital triangle (IST) has been defined. This alternative triangle will allow surgeons to locate the artery more proximally, where its course is more predictable. The purpose of this study was to better define the anatomy of both triangles by measuring their borders and calculating their areas. Ethical clearance was obtained from the University of Pretoria (reference number: 222/2021) and both triangles were subsequently dissected out on both the left and right sides of 33 formalin-fixed human adult cadavers. The borders of each triangle were measured using a digital calliper and the areas were calculated using Herons Formula. The average area of the ST is 969.82±153.15 mm 2 , while the average area of the IST is 307.48±41.31 mm 2 . No statistically significant differences in the findings were observed between the sides of the body, ancestry, or sex of the cadavers. Measurement and analysis of these triangles provided important anatomical information and speak to their clinical relevance as surgical landmarks with which to locate the vertebral artery. Of particular importance here is the IST, which allows for mobilisation of this artery more proximally, should the ST be occluded.
Keyword
Figure
Reference
-
References
1. Standring S. 2016. Gray's anatomy: the anatomical basis of clinical practice. 41st ed. Elsevier;p. 457–8. p. 744–5.2. Kikuta S, Iwanaga J, Kusukawa J, Tubbs RS. 2019; Triangles of the neck: a review with clinical/surgical applications. Anat Cell Biol. 52:120–7. DOI: 10.5115/acb.2019.52.2.120. PMID: 31338227. PMCID: PMC6624334.
Article3. Yamauchi M, Yamamoto M, Kitamura K, Morita S, Nagakura R, Matsunaga S, Abe S. 2017; Morphological classification and comparison of suboccipital muscle fiber characteristics. Anat Cell Biol. 50:247–54. DOI: 10.5115/acb.2017.50.4.247. PMID: 29354295. PMCID: PMC5768560.
Article4. George T, Tadi P. 2022. Anatomy, head and neck, suboccipital muscles [Internet]. StatPearls;Available from: https://www.ncbi.nlm.nih.gov/books/NBK567762/. cited 2022 Nov 25.5. Sriamornrattanakul K, Akharathammachote N, Chonhenchob A, Mongkolratnan A, Niljianskul N, Phoominaonin IS, Ariyaprakai C, Wongsuriyanan S. 2022; Course of the V3 segment of the vertebral artery relative to the suboccipital triangle as an anatomical marker for a safe far lateral approach: a retrospective clinical study. Surg Neurol Int. 13:304. DOI: 10.25259/SNI_346_2022. PMID: 35928311. PMCID: PMC9345113.
Article6. Arnautović KI, Al-Mefty O. 2002; The microsurgical anatomy of the suboccipital vertebral artery and its surrounding structures. Oper Tech Neurosurg. 5:1–10. DOI: 10.1053/otns.2002.31255.
Article7. Tjahjadi M, Rezai Jahromi B, Serrone J, Nurminen V, Choque-Velasquez J, Kivisaari R, Lehto H, Niemelä M, Hernesniemi J. 2017; Simple lateral suboccipital approach and modification for vertebral artery aneurysms: a study of 52 cases over 10 years. World Neurosurg. 108:336–46. DOI: 10.1016/j.wneu.2017.09.014. PMID: 28899830.
Article8. Fisahn C, Burgess B, Iwanaga J, Alonso F, Chapman JR, Oskouian RJ, Tubbs RS. 2017; A previously unreported arterial variant of the suboccipital region based on cadaveric dissection. J Neurol Surg Rep. 78:e40–2. DOI: 10.1055/s-0037-1600136. PMID: 28299248. PMCID: PMC5350074. PMID: 5b510616e1e44ec39f00fbd374421a9f.
Article9. La Rocca G, Altieri R, Ricciardi L, Olivi A, Della Pepa GM. 2017; Anatomical study of occipital triangles: the 'inferior' suboccipital triangle, a useful vertebral artery landmark for safe postero-lateral skull base surgery. Acta Neurochir (Wien). 159:1887–91. DOI: 10.1007/s00701-017-3300-3. PMID: 28828558.
Article10. Molinari RW, Chimenti PC, Molinari R Jr, Gruhn W. 2015; Vertebral artery injury during routine posterior cervical exposure: case reports and review of literature. Global Spine J. 5:528–32. DOI: 10.1055/s-0035-1566225. PMID: 26682106. PMCID: PMC4671909.
Article11. George B, Blanquet A, Alves O. 2002; The V3 segment of the vertebral artery: surgery around the craniocervical junction. Oper Tech Neurosurg. 5:50–74. DOI: 10.1053/otns.2002.000.
Article12. Khanfour AA, El Sekily NM. 2015; Relation of the vertebral artery segment from C1 to C2 vertebrae: an anatomical study. Alex J Med. 51:143–51. DOI: 10.1016/j.ajme.2014.05.007.
Article13. Balik V, Takizawa K. 2019; Safe and bloodless exposure of the third segment of the vertebral artery: a step-by-step overview based on over 50 personal cases. Neurosurg Rev. 42:991–7. DOI: 10.1007/s10143-019-01158-5. PMID: 31410682.
Article14. Detton AJ. 2016. Grant's dissector. 16th ed. Wolters Kluwer;p. 16–7. DOI: 10.1007/springerreference_12767.15. Lowry HV. 1964; Heron's formula. Math Gaz. 48:312–3. DOI: 10.2307/3613028.16. Kalmanson OA, Khayatzadeh S, Germanwala A, Scott-Young M, Havey RM, Voronov LI, Patwardhan AG. 2019; Anatomic considerations in headaches associated with cervical sagittal imbalance: a cadaveric biomechanical study. J Clin Neurosci. 65:140–4. DOI: 10.1016/j.jocn.2019.02.003. PMID: 30876933.
Article17. Muralimohan S, Pande A, Vasudevan MC, Ramamurthi R. 2009; Suboccipital segment of the vertebral artery: a cadaveric study. Neurol India. 57:447–52. DOI: 10.4103/0028-3886.55610. PMID: 19770546.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Triangles of the neck: a review with clinical/surgical applications
- A Study on the Anatomical Position of the Inferior Oblique Muscle Insertion in Primary Inferior Oblique Overaction
- Surgical Treatment by the Far Lateral Inferial Suboccipital Approach for the Distal Vertebral Artery Aneurysm
- A Case of Bilateral Bridges of a Korean Atlas
- Clinical Experiences of Trigeminal Rhizotomy using Suboccipital Approach