Diabetes Metab J.
2023 Sep;47(5):632-642. 10.4093/dmj.2023.0135.
Dyslipidemia Fact Sheet in South Korea, 2022
- Affiliations
-
- 1Department of Cardiology, Kyung Hee University Hospital at Gangdong, College of Medicine, Kyung Hee University, Seoul, Korea
- 2Department of Preventive Medicine, Yonsei University College of Medicine, Seoul, Korea
- 3Division of Cardiology, Department of Internal Medicine, Kangdong Sacred Heart Hospital, College of Medicine, Hallym University, Seoul, Korea
- 4Department of Internal Medicine, Korea University Anam Hospital, Korea University College of Medicine, Seoul, Korea
- 5Department of Internal Medicine, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- 6Department of Internal Medicine, Inje University Sanggye Paik Hospital, College of Medicine, Inje University, Seoul, Korea
- 7School of Biosystem and Biomedical Science, Korea University, Seoul, Korea
- 8Division of Endocrinology and Metabolism, Department of Internal Medicine, Jeonbuk National University Medical School, Jeonju, Korea
- 9Department of Public Health, Yonsei University Graduate School, Seoul, Korea
- 10Department of Endocrinology and Metabolism, Kyung Hee University Hospital at Gangdong, College of Medicine, Kyung Hee University, Seoul, Korea
- KMID: 2546122
- DOI: http://doi.org/10.4093/dmj.2023.0135
Abstract
- Background
This study aimed to investigate the prevalence and status of dyslipidemia management among South Korean adults, as performed by the Korean Society of Lipid and Atherosclerosis under the name Dyslipidemia Fact Sheet 2022.
Methods
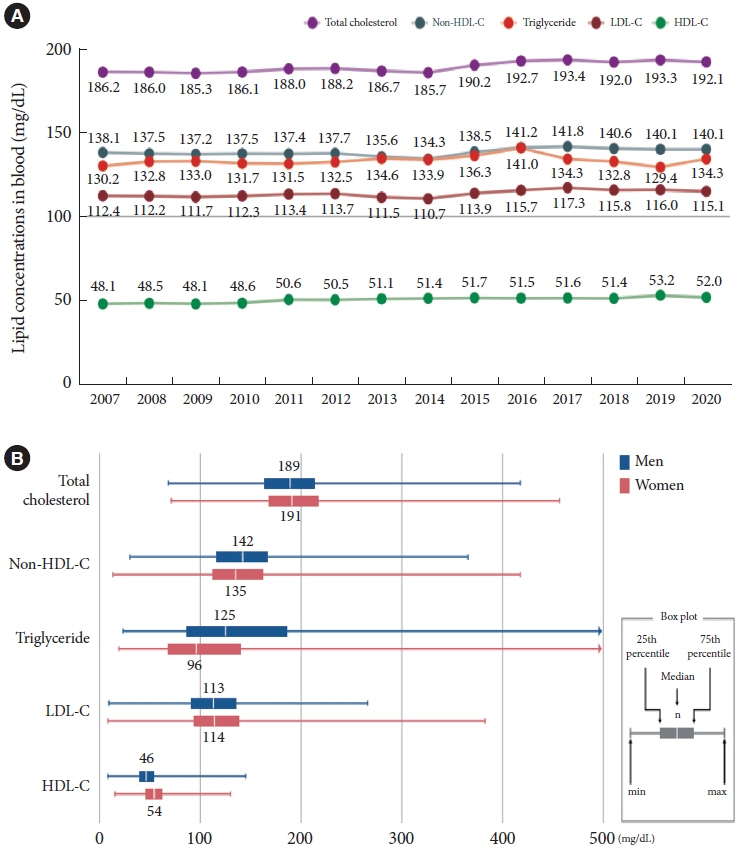
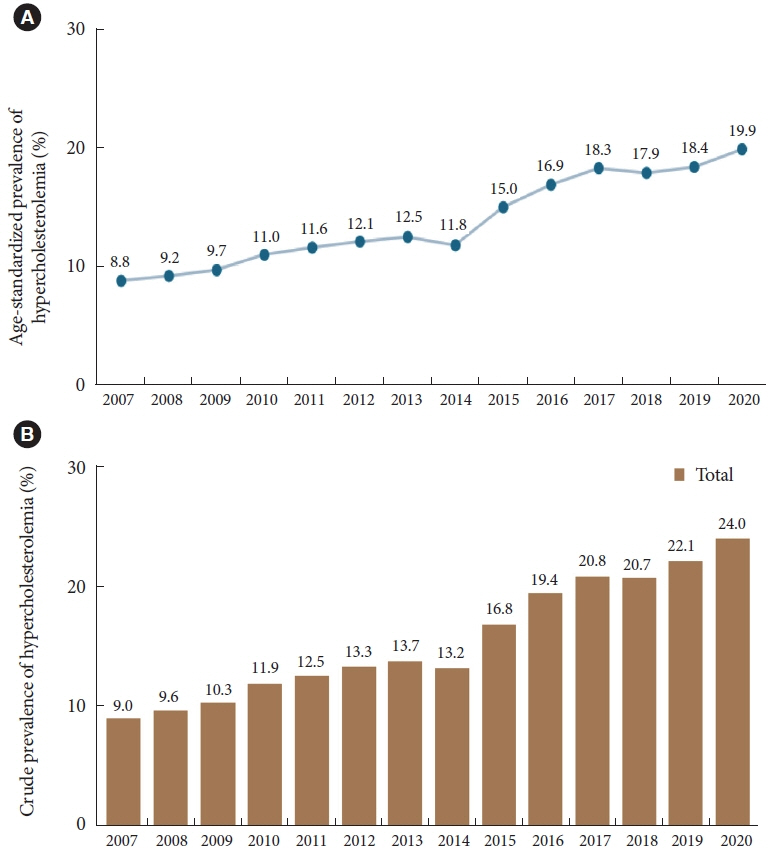
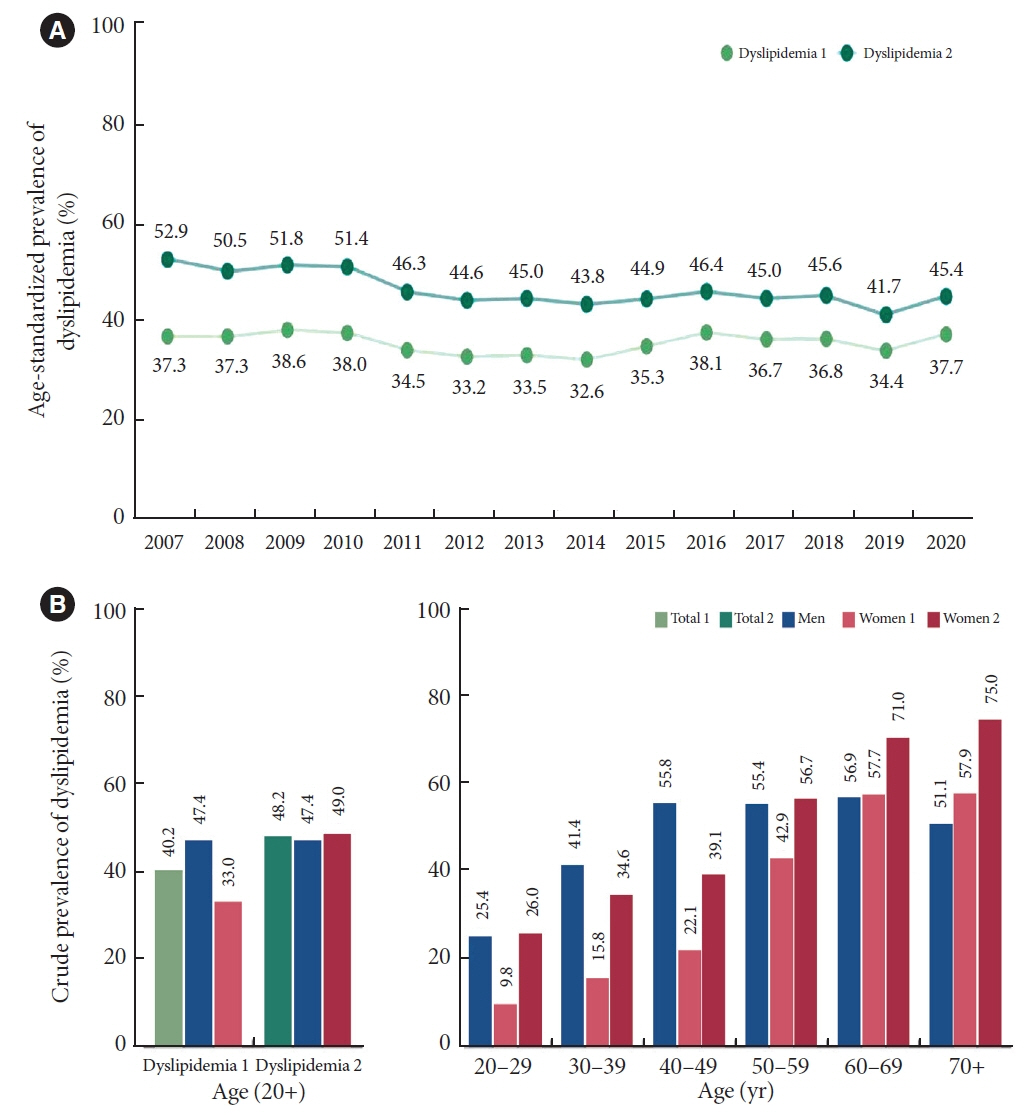
We analyzed the lipid profiles, age-standardized and crude prevalence, management status of hypercholesterolemia and dyslipidemia, and health behaviors among Korean adults aged ≥20 years, using the Korea National Health and Nutrition Examination Survey data between 2007 and 2020.
Results
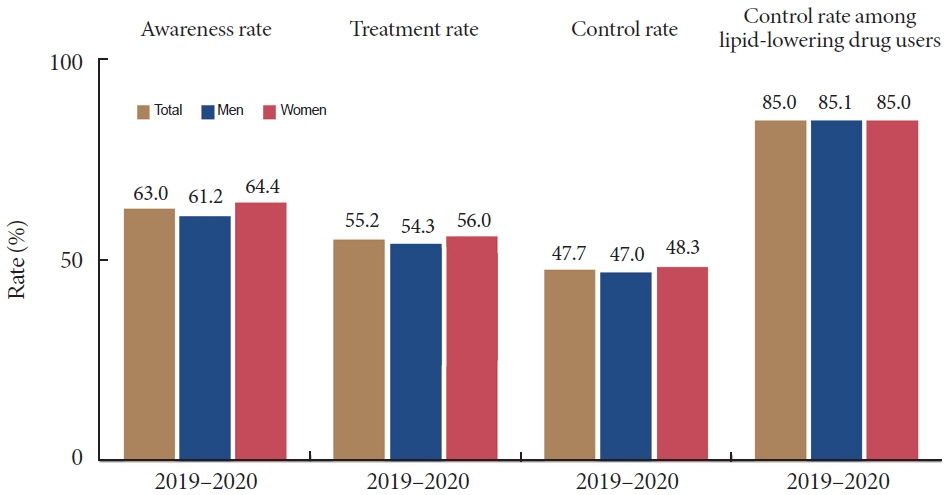
In South Korea, the crude prevalence of hypercholesterolemia (total cholesterol ≥240 mg/dL or use of a lipid-lowering drug) in 2020 was 24%, and the age-standardized prevalence of hypercholesterolemia more than doubled from 2007 to 2020. The crude treatment rate was 55.2%, and the control rate was 47.7%. The crude prevalence of dyslipidemia—more than one out of three conditions (low-density lipoprotein cholesterol ≥160 or the use of a lipid-lowering drug, triglycerides ≥200, or high-density lipoprotein cholesterol [HDL-C] [men and women] <40 mg/dL)—was 40.2% between 2016 and 2020. However, it increased to 48.2% when the definition of hypo-HDL-cholesterolemia in women changed from <40 to <50 mg/dL.
Conclusion
Although the prevalence of hypercholesterolemia and dyslipidemia has steadily increased in South Korea, the treatment rate remains low. Therefore, continuous efforts are needed to manage dyslipidemia through cooperation between the national healthcare system, patients, and healthcare providers.
Keyword
Figure
Reference
-
1. Rhee EJ, Kim HC, Kim JH, Lee EY, Kim BJ, Kim EM, et al. 2018 Guidelines for the management of dyslipidemia in Korea. J Lipid Atheroscler. 2019; 8:78–131.2. World Health Organization. Fact sheets: cardiovascular diseases (CVDs). Available from: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) (cited 2023 Jul 10).3. Cho SMJ, Lee H, Lee HH, Baek J, Heo JE, Joo HJ, et al. Dyslipidemia fact sheets in Korea 2020: an analysis of nationwide population-based data. J Lipid Atheroscler. 2021; 10:202–9.4. Kweon S, Kim Y, Jang MJ, Kim Y, Kim K, Choi S, et al. Data resource profile: the Korea National Health and Nutrition Examination Survey (KNHANES). Int J Epidemiol. 2014; 43:69–77.5. Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972; 18:499–502.6. Seo MH, Lee WY, Kim SS, Kang JH, Kang JH, Kim KK, et al. 2018 Korean Society for the Study of Obesity guideline for the management of obesity in Korea. J Obes Metab Syndr. 2019; 28:40–5.7. Yun S, Park S, Yook SM, Kim K, Shim JE, Hwang JY, et al. Development of the Korean Healthy Eating Index for adults, based on the Korea National Health and Nutrition Examination Survey. Nutr Res Pract. 2022; 16:233–47.8. Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, et al. 2019 ESC/EAS guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 2020; 41:111–88.9. Yang YS, Kim HL, Kim SH, Moon MK. Lipid management in Korean people with type 2 diabetes mellitus: Korean Diabetes Association and Korean Society of Lipid and Atherosclerosis Consensus Statement. Diabetes Metab J. 2023; 47:1–9.10. Yang YS, Han BD, Han K, Jung JH, Son JW; Taskforce Team of the Obesity Fact Sheet of the Korean Society for the Study of Obesity. Obesity fact sheet in Korea, 2021: trends in obesity prevalence and obesity-related comorbidity incidence stratified by age from 2009 to 2019. J Obes Metab Syndr. 2022; 31:169–77.11. Wilson PW, Grundy SM. The metabolic syndrome: a practical guide to origins and treatment: Part II. Circulation. 2003; 108:1537–40.12. Williams CM. Lipid metabolism in women. Proc Nutr Soc. 2004; 63:153–60.13. Hur KY, Moon MK, Park JS, Kim SK, Lee SH, Yun JS, et al. 2021 Clinical practice guidelines for diabetes mellitus of the Korean Diabetes Association. Diabetes Metab J. 2021; 45:461–81.14. Lingvay I, Sumithran P, Cohen RV, le Roux CW. Obesity management as a primary treatment goal for type 2 diabetes: time to reframe the conversation. Lancet. 2022; 399:394–405.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prevalence and Current Management of Cardiovascular Risk Factors in Korean Adults Based on Fact Sheets
- Dementia Epidemiology Fact Sheet 2022
- Dyslipidemia Fact Sheet in South Korea, 2022
- Obesity Fact Sheet in Korea, 2020: Prevalence of Obesity by Obesity Class from 2009 to 2018
- Fact Sheet on Cardiac Rehabilitation for Cardiovascular Disease in South Korea