J Korean Neurosurg Soc.
2023 Sep;66(5):605-608. 10.3340/jkns.2023.0148.
Letter to the Editor : Classifying the Anatomical Location of the Ureter after Retroperitoneal Dissection
- Affiliations
-
- 1Department of Neurosurgery, Pusan National University Yangsan Hospital, Research Institute for Convergence of Biomedical Science and Technology, Pusan National University Yangsan Hospital, Yangsan, Korea
- 2Department of Neurosurgery, School of Medicine, Pusan National University, Yangsan, Korea
- KMID: 2545352
- DOI: http://doi.org/10.3340/jkns.2023.0148
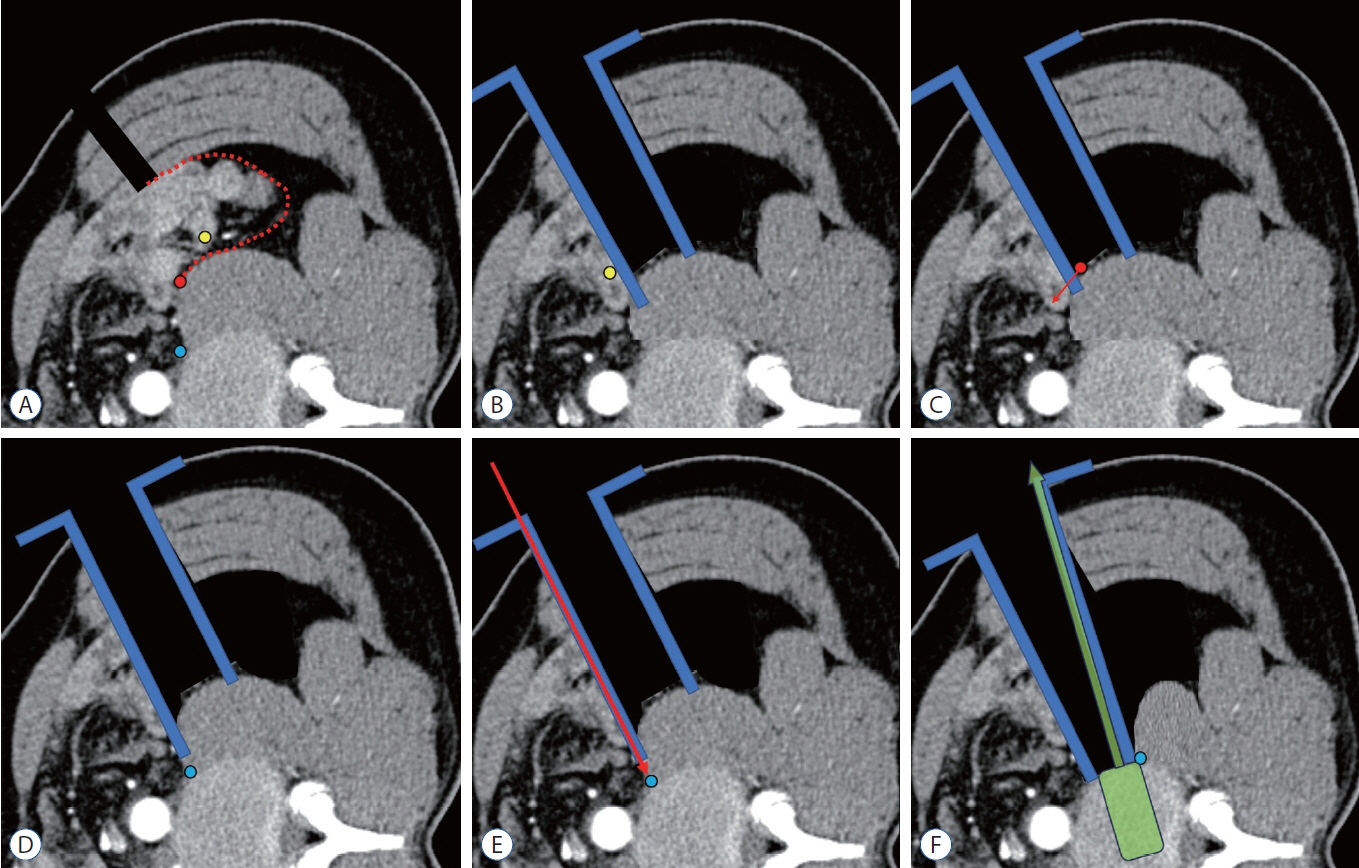
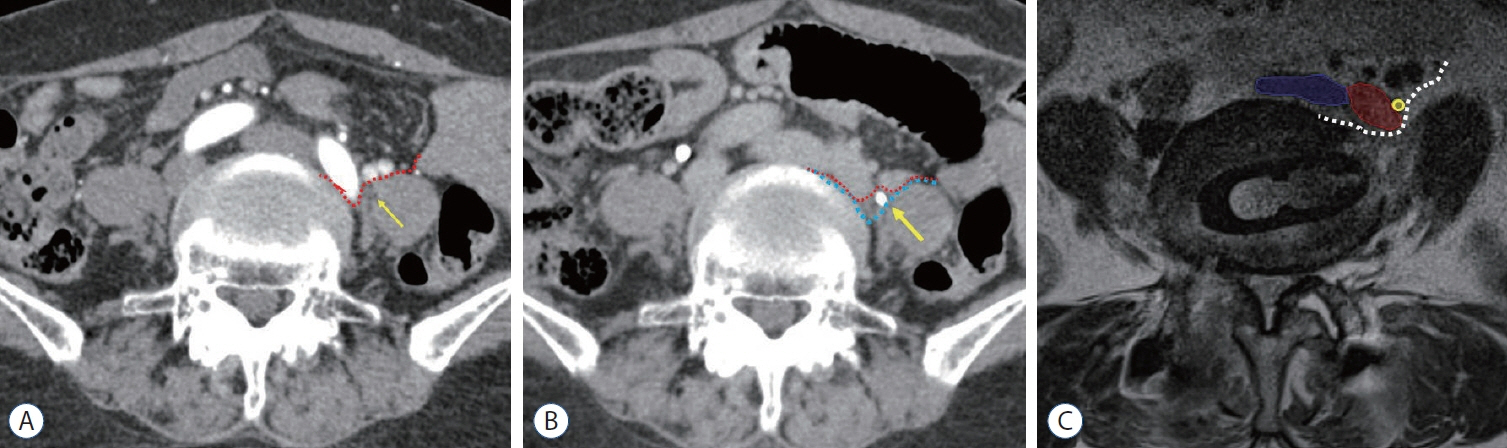
Figure
Reference
-
References
1. Abe K, Orita S, Mannoji C, Motegi H, Aramomi M, Ishikawa T, et al. Perioperative complications in 155 patients who underwent oblique lateral interbody fusion surgery: perspectives and indications from a retrospective, multicenter survey. Spine (Phila Pa 1976). 42:55–62. 2017.2. Bjurlin MA, Rousseau LA, Vidal PP, Hollowell CM. Iatrogenic ureteral injury secondary to a thoracolumbar lateral revision instrumentation and fusion. Spine J. 9:e13–e15. 2009.3. Fujibayashi S, Otsuki B, Kimura H, Tanida S, Masamoto K, Matsuda S. Preoperative assessment of the ureter with dual-phase contrastenhanced computed tomography for lateral lumbar interbody fusion procedures. J Orthop Sci. 22:420–424. 2017.4. Huang C, Bian Z, Zhu L. Morphometric analysis of the ureter with respect to lateral lumbar interbody fusion using contrast-enhanced computed tomography. J Korean Neurosurg Soc. 66:155–161. 2023.5. Kim H, Chang BS, Chang SY. Pearls and pitfalls of oblique lateral interbody fusion: a comprehensive narrative review. Neurospine. 19:163–176. 2022.6. Kubota G, Orita S, Umimura T, Takahashi K, Ohtori S. Insidious intraoperative ureteral injury as a complication in oblique lumbar interbody fusion surgery: a case report. BMC Res Notes. 10:193. 2017.7. Lee HJ, Kim JS, Ryu KS, Park CK. Ureter injury as a complication of oblique lumbar interbody fusion. World Neurosurg. 102:693.e7–693.e14. 2017.8. Lee KH, Son DW, Oh BK, Lee SH, Lee JS, Kim YH, et al. Incidental ureteral complication in single-center consecutive oblique lateral interbody fusion cases. Turk Neurosurg. 2023; [Epub ahead of print].9. Lee YS, Lee DH, Cho DC, Han I, Kim CH, Kwon HD, et al. The change of spinal canal according to oblique lumbar interbody fusion in degenerative spondylolisthesis: a prospective observational study. Neurospine. 19:492–500. 2022.10. Oh BK, Son DW, Lee SH, Lee JS, Sung SK, Lee SW, et al. Learning curve and complications experience of oblique lateral interbody fusion : a single-center 143 consecutive cases. J Korean Neurosurg Soc. 64:447–459. 2021.11. Ouchida J, Kanemura T, Satake K, Nakashima H, Segi N. Anatomic evaluation of retroperitoneal organs for lateral approach surgery: a prospective imaging study using computed tomography in the lateral decubitus position. Eur Spine J. 28:835–841. 2019.12. Park SJ, Hwang JM, Cho DC, Lee S, Kim CH, Han I, et al. Indirect decompression using oblique lumbar interbody fusion revision surgery following previous posterior decompression: comparison of clinical and radiologic outcomes between direct and indirect decompression revision surgery. Neurospine. 19:544–554. 2022.13. Quillo-Olvera J, Lin GX, Jo HJ, Kim JS. Complications on minimally invasive oblique lumbar interbody fusion at L2-L5 levels: a review of the literature and surgical strategies. Ann Transl Med. 6:101. 2018.14. Son D, Lee S. Oblique Lumbar Interbody Fusion (OLIF) in Ahn Y, Park JK, Park CK (eds). Core Techniques of Minimally Invasive Spine Surgery. Singapore: Springer;2023. p. 243–265.15. Yingsakmongkol W, Jitpakdee K, Kerr S, Limthongkul W, Kotheeranurak V, Singhatanadgige W. Successful criteria for indirect decompression with lateral lumbar interbody fusion. Neurospine. 19:805–815. 2022.16. Yoon SG, Kim MS, Kwon SC, Lyo IU, Sim HB. Delayed ureter stricture and kidney atrophy after oblique lumbar interbody fusion. World Neurosurg. 134:137–140. 2020.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ureteral Stricture from Retroperitoneal Fibrosis Caused by Isolated Common Iliac Artery Aneurysm
- Morphometric Analysis of the Ureter with Respect to Lateral Lumbar Interbody Fusion Using Contrast-Enhanced Computed Tomography
- A Case of Unilateral Pelvic Kidney contained a Calculus
- Manufacture of the Serially Sectioned Images of the Whole Body (Fifth Report: Methods for Manufacture of the Three Dimensional Images and Virtual Dissection Software)
- Letter from Editor