J Korean Med Sci.
2023 Jul;38(29):e230. 10.3346/jkms.2023.38.e230.
Current Status and Physicians’ Perspectives of Childhood Cancer Survivorship in Korea: A Nationwide Survey of Pediatric Hematologists/ Oncologists
- Affiliations
-
- 1Department of Pediatrics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2Department of Family Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 3Department of Pediatrics, Chonnam National University Hwasun Hospital, Chonnam National University Medical School, Gwangju, Korea
- 4Department of Pediatrics, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 5National Cancer Control Institute, National Cancer Center, Goyang, Korea
- 6Center for Pediatric Cancer, National Cancer Center, Goyang, Korea
- KMID: 2544945
- DOI: http://doi.org/10.3346/jkms.2023.38.e230
Abstract
- Background
Data on the status of long-term follow-up (LTFU) care for childhood cancer survivors (CCSs) in Korea is lacking. This study was conducted to evaluate the current status of LTFU care for CCSs and relevant physicians’ perspectives.
Methods
A nationwide online survey of pediatric hematologists/oncologists in the Republic of Korea was undertaken.
Results
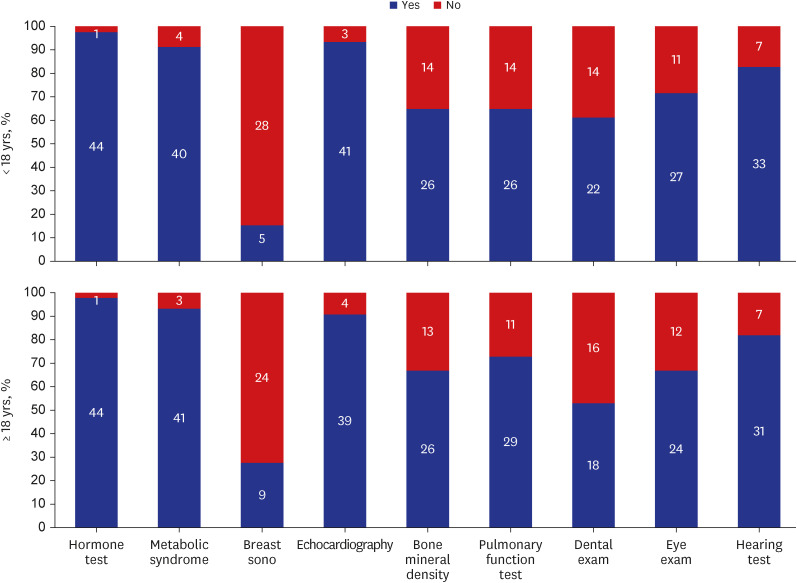
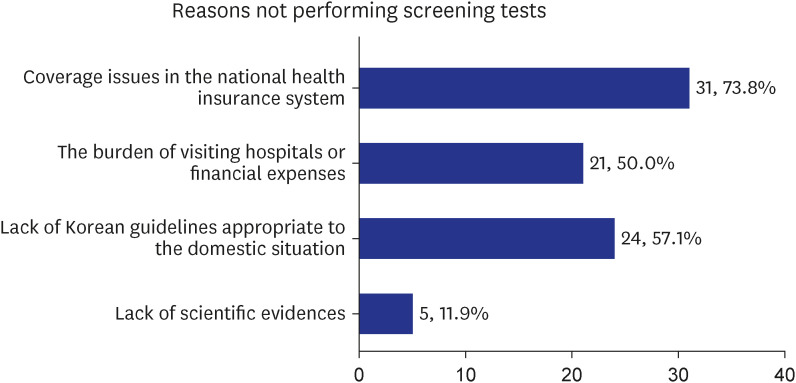
Overall, 47 of the 74 board-certified Korean pediatric hematologists/oncologists currently providing pediatric hematology/oncology care participated in the survey (response rate = 63.5%). Forty-five of the 47 respondents provided LTFU care for CCSs five years after the completion of primary cancer treatment. However, some of the 45 respondents provided LTFU care only for CCS with late complications or CCSs who requested LTFU care. Twenty of the 45 respondents oversaw LTFU care for adult CCSs, although pediatric hematologists/ oncologists experienced more difficulties managing adult CCSs. Many pediatric hematologists/oncologists did not perform the necessary screening test, although CCSs had risk factors for late complications, mostly because of insurance coverage issues and the lack of Korean LTFU guidelines. Regarding a desirable LTFU care system for CCSs in Korea, 27 of the 46 respondents (58.7%) answered that it is desirable to establish a multidisciplinary CCSs care system in which pediatric hematologists/oncologists and adult physicians cooperate.
Conclusion
The LTFU care system for CCS is underdeveloped in the Republic of Korea. It is urgent to establish an LTFU care system to meet the growing needs of Korean CCSs, which should include Korean CCSs care guidelines, provider education plans, the establishment of multidisciplinary care systems, and a supportive national healthcare policy.
Keyword
Figure
Cited by 1 articles
-
Commentary on "Long-term endocrine sequelae after hematopoietic stem cell transplantation in children and adolescents"
So Yoon Jung
Ann Pediatr Endocrinol Metab. 2024;29(2):73-74. doi: 10.6065/apem.2423023edi02.
Reference
-
1. Gatta G, Botta L, Rossi S, Aareleid T, Bielska-Lasota M, Clavel J, et al. Childhood cancer survival in Europe 1999-2007: results of EUROCARE-5--a population-based study. Lancet Oncol. 2014; 15(1):35–47. PMID: 24314616.2. Park HJ, Moon EK, Yoon JY, Oh CM, Jung KW, Park BK, et al. Incidence and survival of childhood cancer in Korea. Cancer Res Treat. 2016; 48(3):869–882. PMID: 26790965.3. Bhakta N, Liu Q, Ness KK, Baassiri M, Eissa H, Yeo F, et al. The cumulative burden of surviving childhood cancer: an initial report from the St Jude Lifetime Cohort Study (SJLIFE). Lancet. 2017; 390(10112):2569–2582. PMID: 28890157.4. Hudson MM, Mulrooney DA, Bowers DC, Sklar CA, Green DM, Donaldson SS, et al. High-risk populations identified in Childhood Cancer Survivor Study investigations: implications for risk-based surveillance. J Clin Oncol. 2009; 27(14):2405–2414. PMID: 19289611.5. Hudson MM, Ness KK, Gurney JG, Mulrooney DA, Chemaitilly W, Krull KR, et al. Clinical ascertainment of health outcomes among adults treated for childhood cancer. JAMA. 2013; 309(22):2371–2381. PMID: 23757085.6. Armenian SH, Hudson MM, Mulder RL, Chen MH, Constine LS, Dwyer M, et al. Recommendations for cardiomyopathy surveillance for survivors of childhood cancer: a report from the International Late Effects of Childhood Cancer Guideline Harmonization Group. Lancet Oncol. 2015; 16(3):e123–e136. PMID: 25752563.7. Gebauer J, Baust K, Bardi E, Grabow D, Stein A, van der Pal HJ, et al. Guidelines for long-term follow-up after childhood cancer: practical implications for the daily work. Oncol Res Treat. 2020; 43(3):61–69. PMID: 31931503.8. Landier W, Bhatia S, Eshelman DA, Forte KJ, Sweeney T, Hester AL, et al. Development of risk-based guidelines for pediatric cancer survivors: the Children’s Oncology Group Long-Term Follow-Up Guidelines from the Children’s Oncology Group Late Effects Committee and Nursing Discipline. J Clin Oncol. 2004; 22(24):4979–4990. PMID: 15576413.9. Mulder RL, Kremer LC, Hudson MM, Bhatia S, Landier W, Levitt G, et al. Recommendations for breast cancer surveillance for female survivors of childhood, adolescent, and young adult cancer given chest radiation: a report from the International Late Effects of Childhood Cancer Guideline Harmonization Group. Lancet Oncol. 2013; 14(13):e621–e629. PMID: 24275135.10. van Dorp W, Mulder RL, Kremer LC, Hudson MM, van den Heuvel-Eibrink MM, van den Berg MH, et al. Recommendations for premature ovarian insufficiency surveillance for female survivors of childhood, adolescent, and young adult cancer: a report from the International Late Effects of Childhood Cancer Guideline Harmonization Group in Collaboration With the PanCareSurFup Consortium. J Clin Oncol. 2016; 34(28):3440–3450. PMID: 27458300.11. Armstrong GT, Liu Q, Yasui Y, Neglia JP, Leisenring W, Robison LL, et al. Late mortality among 5-year survivors of childhood cancer: a summary from the Childhood Cancer Survivor Study. J Clin Oncol. 2009; 27(14):2328–2338. PMID: 19332714.12. Armstrong GT, Pan Z, Ness KK, Srivastava D, Robison LL. Temporal trends in cause-specific late mortality among 5-year survivors of childhood cancer. J Clin Oncol. 2010; 28(7):1224–1231. PMID: 20124180.13. Bagnasco F, Caruso S, Andreano A, Valsecchi MG, Jankovic M, Biondi A, et al. Late mortality and causes of death among 5-year survivors of childhood cancer diagnosed in the period 1960-1999 and registered in the Italian Off-Therapy Registry. Eur J Cancer. 2019; 110:86–97. PMID: 30772657.14. Han JW, Kwon SY, Won SC, Shin YJ, Ko JH, Lyu CJ. Comprehensive clinical follow-up of late effects in childhood cancer survivors shows the need for early and well-timed intervention. Ann Oncol. 2009; 20(7):1170–1177. PMID: 19270031.15. Mertens AC, Liu Q, Neglia JP, Wasilewski K, Leisenring W, Armstrong GT, et al. Cause-specific late mortality among 5-year survivors of childhood cancer: the Childhood Cancer Survivor Study. J Natl Cancer Inst. 2008; 100(19):1368–1379. PMID: 18812549.16. Geenen MM, Cardous-Ubbink MC, Kremer LC, van den Bos C, van der Pal HJ, Heinen RC, et al. Medical assessment of adverse health outcomes in long-term survivors of childhood cancer. JAMA. 2007; 297(24):2705–2715. PMID: 17595271.17. Oeffinger KC, Mertens AC, Sklar CA, Kawashima T, Hudson MM, Meadows AT, et al. Chronic health conditions in adult survivors of childhood cancer. N Engl J Med. 2006; 355(15):1572–1582. PMID: 17035650.18. Robison LL, Hudson MM. Survivors of childhood and adolescent cancer: life-long risks and responsibilities. Nat Rev Cancer. 2014; 14(1):61–70. PMID: 24304873.19. United Kingdom Children’s Cancer Study Group Late Effects Group. Therapy based long term follow up practice statement, 2005. Updated 2005. Accessed February 1, 2023. http://www.cclg.org.uk/write/mediauploads/member%20area/treatment%20guidelines/ltfu-full.pdf .20. Children’s Oncology Group. Long-term follow-up guidelines for survivors of childhood, adolescent, and young adult cancers, version 5.0 (October 2018). Updated 2018. Accessed February 1, 2023. http://www.survivorshipguidelines.org .21. Dutch Childhood Oncology Group. Guidelines for follow-up in survivors of childhood cancer 5 years after diagnosis, 2010. Updated 2014. Accessed February 1, 2023. https://www.skion.nl/workspace/uploads/vertaling-richtlijn-LATER-versie-final-okt2014_2.pdf .22. Hjorth L, Haupt R, Skinner R, Grabow D, Byrne J, Karner S, et al. PanCare Network. Survivorship after childhood cancer: PanCare: a European Network to promote optimal long-term care. Eur J Cancer. 2015; 51(10):1203–1211. PMID: 25958037.23. Landier W, Skinner R, Wallace WH, Hjorth L, Mulder RL, Wong FL, et al. Surveillance for late effects in childhood cancer survivors. J Clin Oncol. 2018; 36(21):2216–2222. PMID: 29874139.24. Kremer LC, Mulder RL, Oeffinger KC, Bhatia S, Landier W, Levitt G, et al. A worldwide collaboration to harmonize guidelines for the long-term follow-up of childhood and young adult cancer survivors: a report from the International Late Effects of Childhood Cancer Guideline Harmonization Group. Pediatr Blood Cancer. 2013; 60(4):543–549. PMID: 23281199.25. Poplack DG, Fordis M, Landier W, Bhatia S, Hudson MM, Horowitz ME. Childhood cancer survivor care: development of the Passport for Care. Nat Rev Clin Oncol. 2014; 11(12):740–750. PMID: 25348788.26. American Academy of Pediatrics Section on Hematology/Oncology Children’s Oncology Group. Long-term follow-up care for pediatric cancer survivors. Pediatrics. 2009; 123(3):906–915. PMID: 19255020.27. Ginsberg JP, Hobbie WL, Carlson CA, Meadows AT. Delivering long-term follow-up care to pediatric cancer survivors: transitional care issues. Pediatr Blood Cancer. 2006; 46(2):169–173. PMID: 16320315.28. Kenney LB, Melvin P, Fishman LN, O’Sullivan-Oliveira J, Sawicki GS, Ziniel S, et al. Transition and transfer of childhood cancer survivors to adult care: a national survey of pediatric oncologists. Pediatr Blood Cancer. 2017; 64(2):346–352. PMID: 27463688.29. Sadak KT, Szalda D, Lindgren BR, Kinahan KE, Eshelman-Kent D, Schwartz LA, et al. Transitional care practices, services, and delivery in childhood cancer survivor programs: a survey study of U.S. survivorship providers. Pediatr Blood Cancer. 2019; 66(8):e27793. PMID: 31099145.30. Miyoshi Y, Yorifuji T, Shimizu C, Nagasaki K, Kawai M, Ishiguro H, et al. A nationwide questionnaire survey targeting Japanese pediatric endocrinologists regarding transitional care in childhood, adolescent, and young adult cancer survivors. Clin Pediatr Endocrinol. 2020; 29(2):55–62. PMID: 32313373.31. Marcoux SM, Laverdière C. Optimizing childhood oncology care transition from pediatric to adult settings: a survey of primary care physicians’ and residents’ perspectives. Clin Invest Med. 2020; 43(2):E14–E23. PMID: 32593272.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Long-term follow-up study and long-term care of childhood cancer survivors
- Time to establish multidisciplinary childhood cancer survivorship programs in Korea
- Understanding Cancer Survivorship and Its New Perspectives
- Perceptions and practice patterns of cancer survivorship care among Japanese gynecologic oncologists: The JGOG questionnaire survey
- Oncologists' Experience with Patients with Second Primary Cancer and the Attitudes toward Second Primary Cancer Screening: A Nationwide Survey