J Korean Med Sci.
2023 Jul;38(27):e214. 10.3346/jkms.2023.38.e214.
Risk Factors for Sudden Death Within 2 Days After Diagnosis of COVID-19 in Korea
- Affiliations
-
- 1Division of Public Health Emergency Response Research, Bureau of Public Health Emergency Preparedness, Korea Disease Control and Prevention Agency, Cheongju, Korea
- 2Division of Healthcare Safety and immunization, Central Disease Control Headquarters, Korea Disease Control and Prevention Agency, Cheongju, Korea
- 3Central Disease Control Headquarters, Korea Disease Control and Prevention Agency, Cheongju, Korea
- KMID: 2544414
- DOI: http://doi.org/10.3346/jkms.2023.38.e214
Abstract
- Background
We aimed to analyze the risk factors for sudden death after diagnosis of coronavirus disease 2019 (COVID-19) in South Korea and to provide evidence for informing prevention and control interventions for patients at risk of sudden death.
Methods
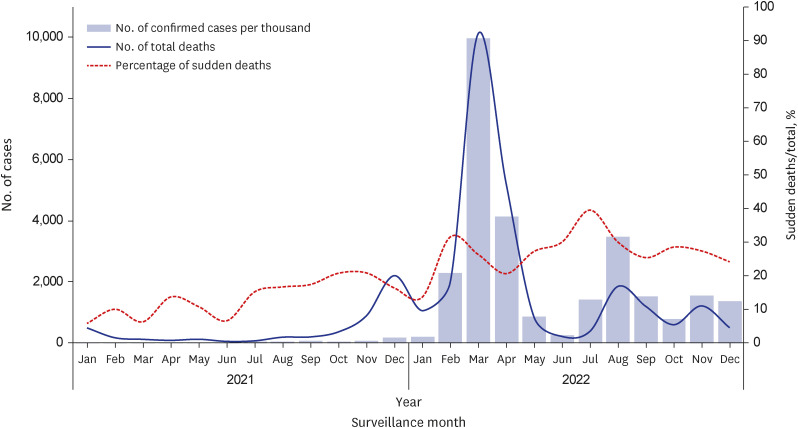
We included 30,302 COVID-19 related deaths registered in the patient management information system (Central Disease Control Headquarters) between January 1, 2021, and December 15, 2022. We collected their epidemiological data recorded by the reporting city, province, or country. We performed multivariate logistic regression analysis to identify risk factors for sudden death after diagnosis of COVID-19.
Results
Among the 30,302 deaths, there were 7,258 (24.0%) and 23,044 (76.0%) sudden and non-sudden deaths, respectively. Sudden death means a person who died within 2 days of diagnosis and who did not receive inpatient treatment. Underlying condition, vaccination status, and place of death were significantly associated with the survival period in all age groups. Moreover, region, sex, and prescription were significantly associated with the survival period only in certain age groups. However, reinfection was not significantly associated with the survival period in any age group.
Conclusion
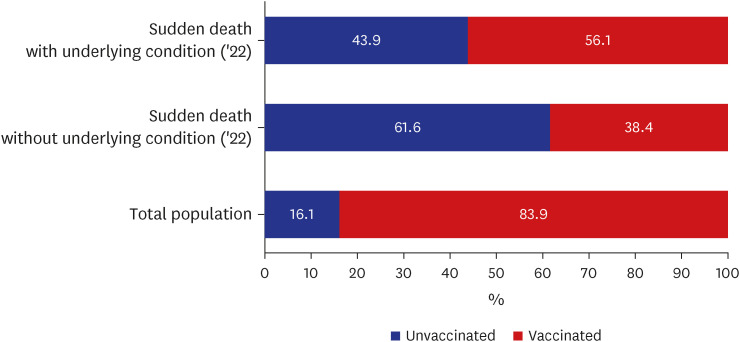
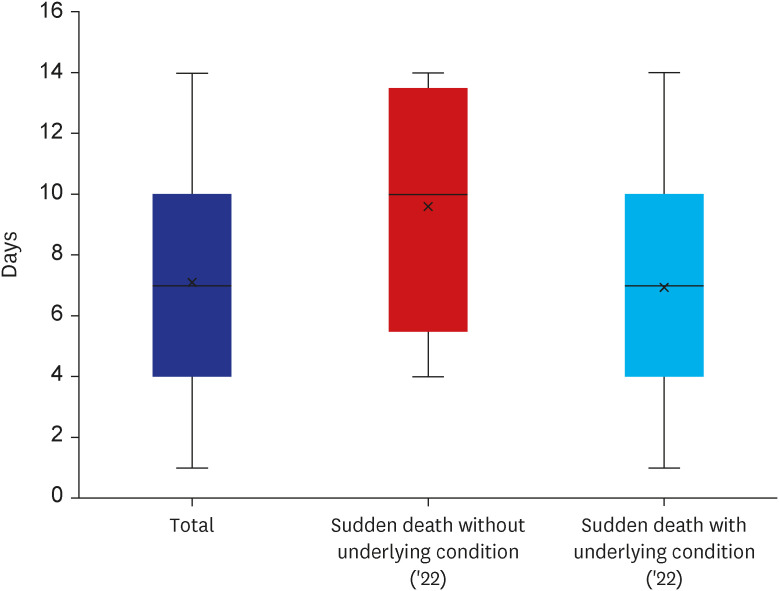
To our knowledge, this is the first study on the risk factors for sudden death after a diagnosis of COVID-19, which included age, underlying condition, vaccination status, and place of death. Additionally, individuals aged < 60 years without an underlying condition were at high risk for sudden death. However, this group has relatively low interest in health, as can be seen from the high non-vaccination rate (16.1% of the general population vs. 61.6% of the corresponding group). Therefore, there is a possibility for the presence of an uncontrolled underlying disease in this population. In addition, many sudden deaths occurred due to delayed hospital visits to continue economic activities even after the onset of COVID-19 symptoms (7 days overall vs. 10 days average for the group). In conclusion, ‘continued interest in health’ is a key factor in avoiding sudden death in the economically active group (under 60 years of age).
Keyword
Figure
Reference
-
1. World Health Organization. WHO Director-General’s opening remarks at the media briefing on COVID-19. Updated 2020. Accessed January 15, 2023. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 .2. World Health Organization. WHO Coronavirus (COVID-19) dashboard. Updated 2023. Accessed January 15, 2023. https://covid19.who.int/ .3. Mathieu E, Ritchie H, Rodés-Guirao L, Appel C, Giattino C, Hasell J, et al. Coronavirus pandemic (COVID-19). Updated 2020. Accessed January 15, 2023. https://ourworldindata.org/coronavirus .4. Hashim MJ, Alsuwaidi AR, Khan G. Population risk factors for COVID-19 mortality in 93 countries. J Epidemiol Glob Health. 2020; 10(3):204–208. PMID: 32954710.5. Noor FM, Islam MM. Prevalence and associated risk factors of mortality among COVID-19 patients: a meta-analysis. J Community Health. 2020; 45(6):1270–1282. PMID: 32918645.6. Sousa GJ, Garces TS, Cestari VR, Florêncio RS, Moreira TM, Pereira ML. Mortality and survival of COVID-19. Epidemiol Infect. 2020; 148:e123. PMID: 32580809.7. Arbel R, Sergienko R, Friger M, Peretz A, Beckenstein T, Yaron S, et al. Effectiveness of a second BNT162b2 booster vaccine against hospitalization and death from COVID-19 in adults aged over 60 years. Nat Med. 2022; 28(7):1486–1490. PMID: 35468276.8. Zheng C, Shao W, Chen X, Zhang B, Wang G, Zhang W. Real-world effectiveness of COVID-19 vaccines: a literature review and meta-analysis. Int J Infect Dis. 2022; 114:252–260. PMID: 34800687.9. Andrews N, Stowe J, Kirsebom F, Toffa S, Rickeard T, Gallagher E, et al. Covid-19 vaccine effectiveness against the omicron (B. 1.1. 529) variant. N Engl J Med. 2022; 386(16):1532–1546. PMID: 35249272.10. Emerging COVID-19 success story: South Korea learned the lessons of MERS. Updated 2021. Accessed January 15, 2023. https://ourworldindata.org/covid-exemplar-south-korea .11. Korea Disease Control and Prevention Agency. COVID19 response guidelines for local government (13-2th). Updated 2022. Accessed January 30, 2023. https://ncov.kdca.go.kr/shBoardView.do?brdId=2&brdGubun=28&ncvContSeq=7112 .12. Korea Disease Control and Prevention Agency. [Press release] Coronavirus disease-19, Republic of Korea. Updated 2023. Assessed January 11, 2023. https://kdca.go.kr/board/board.es?mid=a20501020000&bid=0015&list_no=721655&cg_code=C01&act=view&nPage=6 .
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Risk factors for deaths associated with COVID-19 according to the cause of death classification in Republic of Korea
- QTc prolongation in patients with COVID-19: a retrospective chart review
- Sudden Death Associated With Possible Flare-Ups of Multiple Sclerosis After COVID-19 Vaccination and Infection: A Case Report and Literature Review
- Association of Metabolic Syndrome with COVID-19 in the Republic of Korea
- COVID-19 and Cancer: Questions to Be Answered