Anesth Pain Med.
2023 Apr;18(2):204-209. 10.17085/apm.23002.
Management of unanticipated difficult airway in a patient with well-visualized vocal cords using video laryngoscopy - A case report -
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Inje University Busan Paik Hospital, Inje University College of Medicine, Busan, Korea
- KMID: 2543662
- DOI: http://doi.org/10.17085/apm.23002
Abstract
- Background
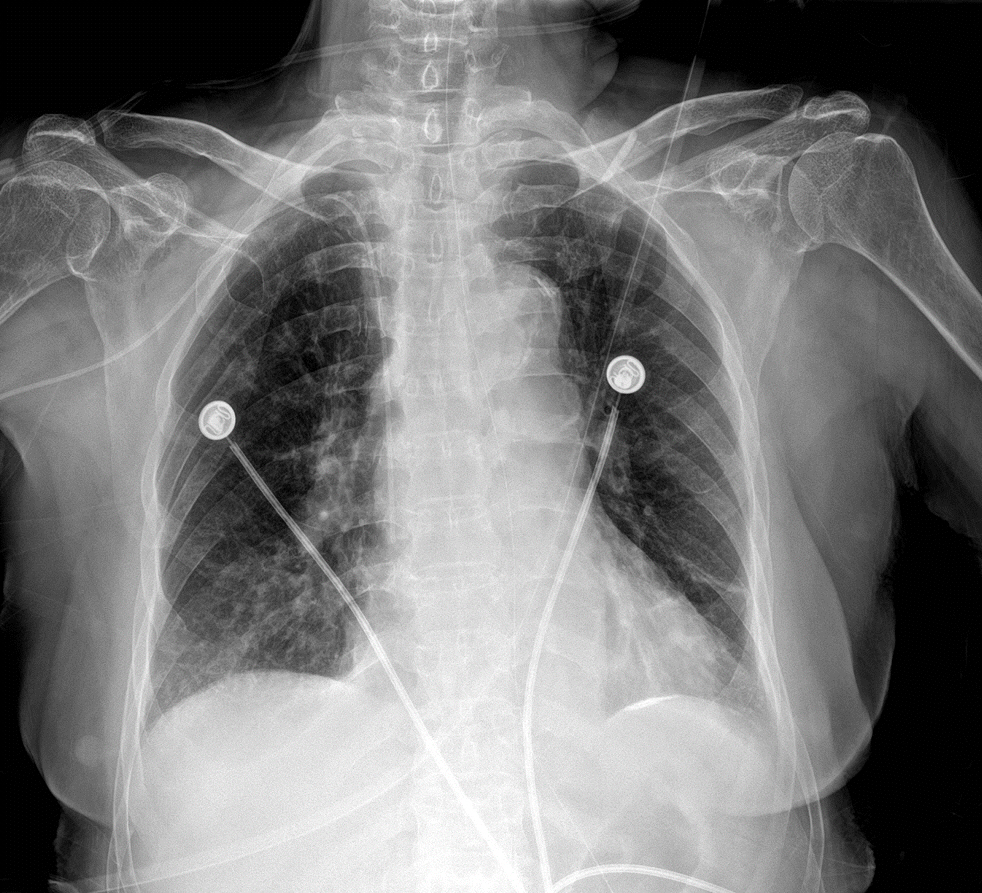
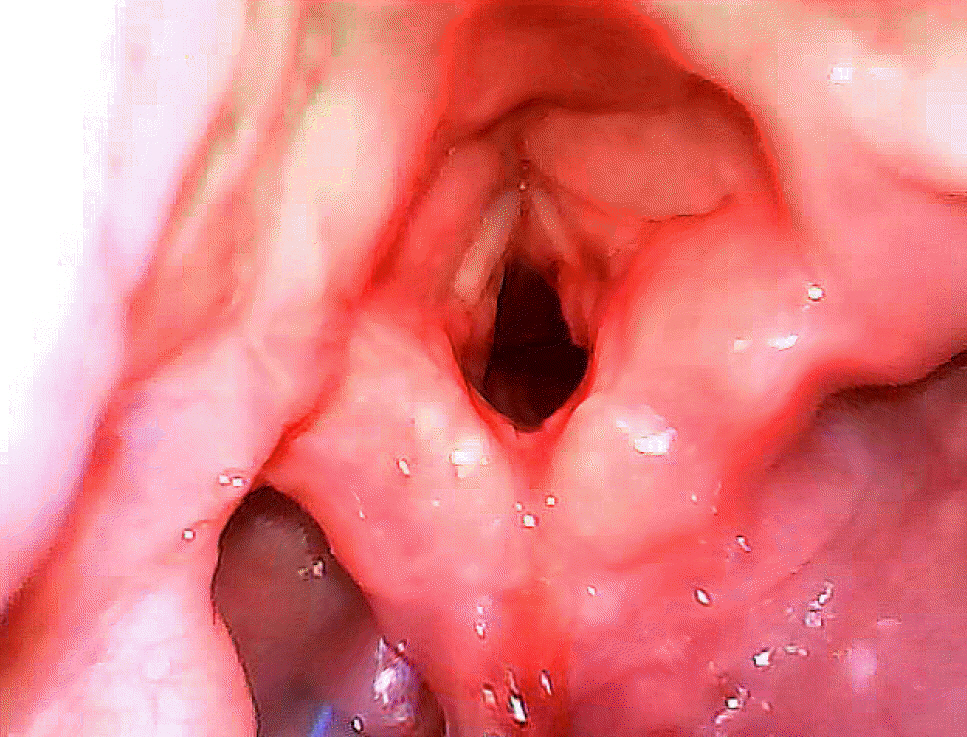
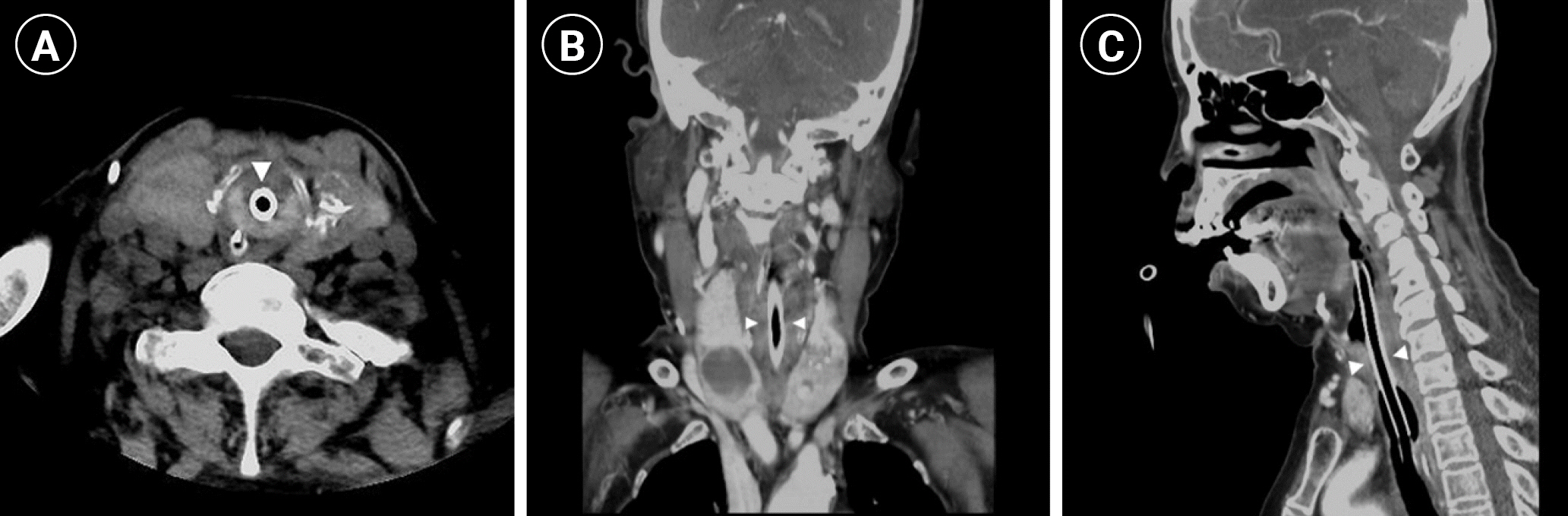
Difficult airway occurs due to anatomical abnormalities of the airway that can be predicted through airway assessments; however, abnormalities beyond the vocal cord can be clinically asymptomatic and undetected until intubation failure to advance the endotracheal tube. Case: We present a case of an unanticipated difficult airway in a stuporous 80-year-old female with a recent history of intracerebral hemorrhage and prolonged intubation. She required emergency ventriculo-peritoneal shunt surgery due to the progression of her hydrocephalus. Under anesthesia, facemask ventilation was easy and video laryngoscopy provided a full view of the glottis; however, endotracheal tube (ETT) entry failed. We suspected stenosis beyond the vocal cord, and a smaller diameter ETT was inserted and maintained for airway management during emergency surgery. Postoperative neck computed tomography findings revealed laryngotracheal stenosis (LTS).
Conclusions
Anesthesiologists should be aware that LTS may be asymptomatic and consider difficult airway guidelines in patients with history of prolonged endotracheal intubation.
Keyword
Figure
Reference
-
1. Apfelbaum JL, Hagberg CA, Connis RT, Abdelmalak BB, Agarkar M, Dutton RP, et al. 2022 American Society of Anesthesiologists practice guidelines for management of the difficult airway. Anesthesiology. 2022; 136:31–81.
Article2. Kheterpal S, Han R, Tremper KK, Shanks A, Tait AR, O'Reilly M, et al. Incidence and predictors of difficult and impossible mask ventilation. Anesthesiology. 2006; 105:885–91.
Article3. Gelbard A, Francis DO, Sandulache VC, Simmons JC, Donovan DT, Ongkasuwan J. Causes and consequences of adult laryngotracheal stenosis. Laryngoscope. 2015; 125:1137–43.
Article4. Brodsky MB, Levy MJ, Jedlanek E, Pandian V, Blackford B, Price C, et al. Laryngeal injury and upper airway symptoms after oral endotracheal intubation with mechanical ventilation during critical care: a systematic review. Crit Care Med. 2018; 46:2010–7.
Article5. Ajit E, Banur A, Bondade K, Raykar P. Postintubation tracheal stenosis: report of two cases and literature review. Indian J Respir Care. 2019; 8:127–9.
Article6. Karmali S, Rose P. Tracheal tube size in adults undergoing elective surgery - a narrative review. Anaesthesia. 2020; 75:1529–39.
Article7. Vogelhut MM, Downs JB. Prolonged endotracheal intubation. Chest. 1979; 76:110–1.
Article8. Adly A, Youssef TA, El-Begermy MM, Younis HM. Timing of tracheostomy in patients with prolonged endotracheal intubation: a systematic review. Eur Arch Otorhinolaryngol. 2018; 275:679–90.
Article9. Parmet JL, Colonna-Romano P, Horrow JC, Miller F, Gonzales J, Rosenberg H. The laryngeal mask airway reliably provides rescue ventilation in cases of unanticipated difficult tracheal intubation along with difficult mask ventilation. Anesth Analg. 1998; 87:661–5.
Article10. Agarwal A, Shobhana N. LMA in neurosurgery. Can J Anaesth. 1995; 42:750.
Article11. Kumar SS, Chaterjee N, Kamath S. LMA and ventriculo-peritoneal shunt surgery: is it the ideal airway? J Neurosurg Anesthesiol. 2009; 21:66.
Article12. Frerk C, Mitchell VS, McNarry AF, Mendonca C, Bhagrath R, Patel A, et al. Difficult Airway Society Intubation Guidelines Working Group. Difficult Airway Society 2015 guidelines for management of unanticipated difficult intubation in adults. Br J Anaesth. 2015; 115:827–48.13. Song SH, Lee WH, Chung WS, Lee JY, Ann MY. Acute traumatic injury and delayed airway obstruction after the use of a GlideScope in a patient with a difficult airway: a case report. Anesth Pain Med. 2017; 12:187–90.
Article14. Popat M, Mitchell V, Dravid R, Patel A, Swampillai C, Higgs A. Difficult Airway Society guidelines for the management of tracheal extubation. Anaesthesia. 2012; 67:318–40.
Article15. Hasegawa S, Koda K, Uzawa M, Kimura H, Kimura R, Kitamura T. Successful airway management with combined use of a McGRATHTM MAC videolaryngoscope and fiberoptic bronchoscope in a patient with congenital tracheal stenosis diagnosed in adulthood. JA Clin Rep. 2021; 7:47.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Unilateral vocal cord palsy occurred after difficult endotracheal intubation using intubating laryngeal mask airway: A case report
- Use of laryngeal mask after repeated endotracheal intubation failure in a patient with tracheobronchopathia osteochondroplastica: case report
- Combined use of a McGrath(R) MAC video laryngoscope and Frova Intubating Introducer in a patient with Pierre Robin syndrome: a case report
- Unanticipated Difficult Intubation in Patient with Undiagnosed Posterior Glottic Stenosis
- Difficult Airway Management with Fiberoptic Bronchoscopy Combined with Video Laryngoscope in a Patient with Ludwig Angina