Nutr Res Pract.
2023 Jun;17(3):529-540. 10.4162/nrp.2023.17.3.529.
Evaluation of medical nutrition therapy using the food-based index of dietary inflammatory potential (FBDI) in diabetes mellitus patients
- Affiliations
-
- 1Department of Food and Nutrition, Wonkwang University, Iksan 54538, Korea
- 2Institute of Life Science and Natural Resources, Wonkwang University, Iksan 54538, Korea
- 3Division of Endocrinology and Metabolism, Department of Medicine, Wonkwang University School of Medicine, Iksan 54538, Korea
- KMID: 2542848
- DOI: http://doi.org/10.4162/nrp.2023.17.3.529
Abstract
- BACKGROUND/OBJECTIVES
Inflammation is often associated with chronic diseases, and numerous studies suggest that certain foods can modulate inflammatory status. This study aimed to assess the impact of intensive nutrition education on glycemic control and inflammation in patients with diabetes mellitus using the Korean food-based index of dietary inflammatory potential (FBDI).
SUBJECTS/METHODS
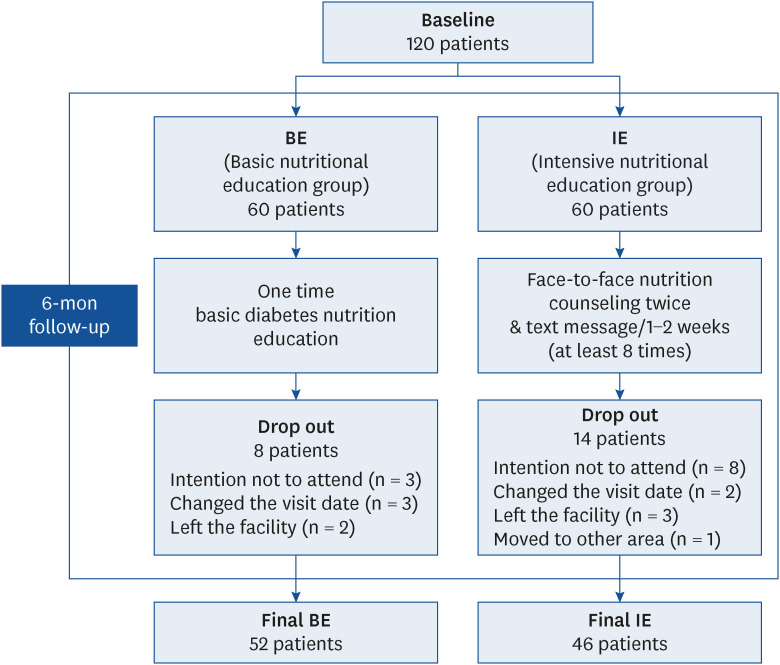
A total of 120 patients (male: 70, 58.3%) were randomly divided into two groups of 60 each, to be given intensive nutritional education (IE) and basic nutritional education (BE), respectively. As part of the nutrition education intervention, basic diabetesrelated nutrition education was provided to both groups initially. In addition, the IE was provided two face-to-face nutrition education sessions based on FBDI over six months, and text transmissions were made at least eight times. We surveyed the anthropometric measurements, biochemical indicators, inflammatory markers, and dietary intake before and after the interventions. We analyzed the effects of the intensive nutrition education using the t-test, χ 2 test and paired t-test.
RESULTS
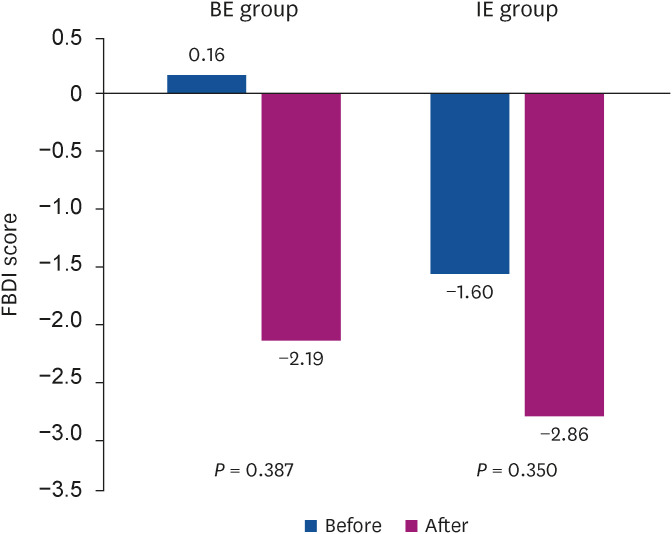
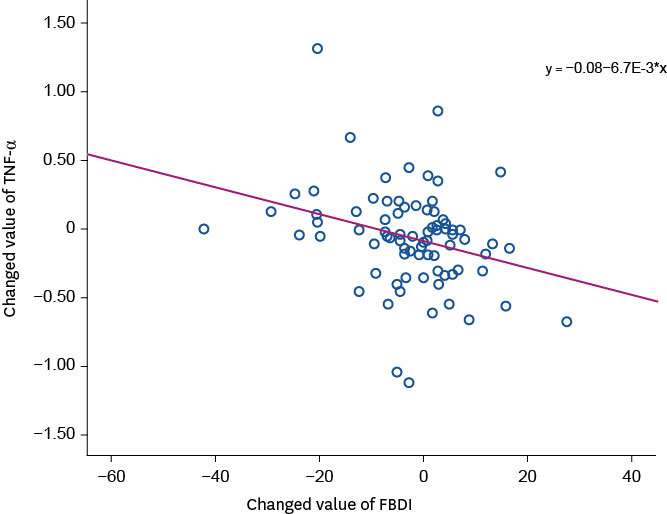
Of the subjects, 76.7% (46/60) of the IE and 86.7% (52/60) of the BE completed the study. The results of the paired t-test to evaluate the effectiveness of nutrition education using FBDI showed that high density lipoprotein-cholesterol increased significantly from 42.6 mg/dL before intervention to 49.2 mg/dL after intervention (P = 0.009), tumor necrosis factor-α significantly decreased from 1.25 pg/mL before intervention to 1.11 pg/mL after intervention (P =.012) in the IE. Also, glycated hemoglobin decreased from 8.0% to 7.5% in the IE but increased from 7.4% to 7.7% in the BE, and the differences between the groups were significant (P= 0.008).
CONCLUSION
These findings suggest that providing intensive FBDI-based education on antiinflammatory foods positively affected glycemic control and inflammatory status in diabetes patients. Therefore, practical dietary plans using FBDI should be considered for diabetes patients to prevent increased inflammation.
Figure
Reference
-
1. Haslam DW, James WP. Obesity. Lancet. 2005; 366:1197–1209. PMID: 16198769.2. Park IB, Baik SH. Epidemiologic characteristics of diabetes mellitus in Korea: Current status of diabetic patients using Korean health insurance database. Korean Diabetes J. 2009; 33:357–362.3. Beck J, Greenwood DA, Blanton L, Bollinger ST, Butcher MK, Condon JE, Cypress M, Faulkner P, Fischl AH, Francis T, et al. 2017 National standards for diabetes self-management education and support. Diabetes Care. 2017; 40:1409–1419. PMID: 28754780.4. American Diabetes Association. Lifestyle management: standards of medical care in diabetes—2019. Diabetes Care. 2019; 42(Suppl 1):S46–S60. PMID: 30559231.5. Davies MJ, D’Alessio DA, Fradkin J, Kernan WN, Mathieu C, Mingrone G, Rossing P, Tsapas A, Wexler DJ, Buse JB. Management of hyperglycemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2018; 41:2669–2701. PMID: 30291106.6. Pawelec G, Goldeck D, Derhovanessian E. Inflammation, ageing and chronic disease. Curr Opin Immunol. 2014; 29:23–28. PMID: 24762450.7. Giugliano D, Ceriello A, Esposito K. The effects of diet on inflammation: emphasis on the metabolic syndrome. J Am Coll Cardiol. 2006; 48:677–685. PMID: 16904534.8. Tsalamandris S, Antonopoulos AS, Oikonomou E, Papamikroulis GA, Vogiatzi G, Papaioannou S, Deftereos S, Tousoulis D. The role of inflammation in diabetes: Current concepts and future perspectives. Eur Cardiol. 2019; 14:50–59. PMID: 31131037.9. Shivappa N, Steck SE, Hurley TG, Hussey JR, Hébert JR. Designing and developing a literature-derived, population-based dietary inflammatory index. Public Health Nutr. 2014; 17:1689–1696. PMID: 23941862.10. Mazidi M, Shivappa N, Wirth MD, Hebert JR, Vatanparast H, Kengne AP. The association between dietary inflammatory properties and bone mineral density and risk of fracture in US adults. Eur J Clin Nutr. 2017; 71:1273–1277. PMID: 29019343.11. Ramallal R, Toledo E, Martínez-González MA, Hernández-Hernández A, García-Arellano A, Shivappa N, Hébert JR, Ruiz-Canela M. Dietary inflammatory index and incidence of cardiovascular disease in the SUN cohort. PLoS One. 2015; 10:e0135221. PMID: 26340022.12. Denova-Gutiérrez E, Muñoz-Aguirre P, Shivappa N, Hébert JR, Tolentino-Mayo L, Batis C, Barquera S. Dietary inflammatory index and type 2 diabetes mellitus in adults: the diabetes mellitus survey of Mexico City. Nutrients. 2018; 10:385. PMID: 29561774.13. Vahid F, Shivappa N, Faghfoori Z, Khodabakhshi A, Zayeri F, Hebert JR, Davoodi SH. Validation of a dietary inflammatory index (DII) and association with risk of gastric cancer: a case-control study. Asian Pac J Cancer Prev. 2018; 19:1471–1477. PMID: 29936717.14. Na W, Yu TY, Sohn C. Development of a food-based index of dietary inflammatory potential for Koreans and its relationship with metabolic syndrome. Nutr Res Pract. 2019; 13:150–158. PMID: 30984359.15. Cho YY, Lee MK, Jang HC, Rha MY, Kim JY, Park YM, Sohn CM. The clinical and cost effectiveness of medical nutrition therapy for patients with type 2 diabetes mellitus. J Nutr Health. 2008; 41:147–155.16. Bouhaidar CM, DeShazo JP, Puri P, Gray P, Robins JL, Salyer J. Text messaging as adjunct to community-based weight management program. Comput Inform Nurs. 2013; 31:469–476. PMID: 24141325.17. Kim JY, Oh S, Steinhubl S, Kim S, Bae WK, Han JS, Kim JH, Lee K, Kim MJ. Effectiveness of 6 months of tailored text message reminders for obese male participants in a worksite weight loss program: randomized controlled trial. JMIR Mhealth Uhealth. 2015; 3:e14. PMID: 25648325.18. Livingstone KM, Celis-Morales C, Navas-Carretero S, San-Cristobal R, Macready AL, Fallaize R, Forster H, Woolhead C, O’Donovan CB, Marsaux CF, et al. Effect of an Internet-based, personalized nutrition randomized trial on dietary changes associated with the Mediterranean diet: the Food4Me Study. Am J Clin Nutr. 2016; 104:288–297. PMID: 27357094.19. Mann S, Beedie C, Balducci S, Zanuso S, Allgrove J, Bertiato F, Jimenez A. Changes in insulin sensitivity in response to different modalities of exercise: a review of the evidence. Diabetes Metab Res Rev. 2014; 30:257–268. PMID: 24130081.20. Bruunsgaard H. Physical activity and modulation of systemic low-level inflammation. J Leukoc Biol. 2005; 78:819–835. PMID: 16033812.21. Pickup JC, Chusney GD, Thomas SM, Burt D. Plasma interleukin-6, tumour necrosis factor α and blood cytokine production in type 2 diabetes. Life Sci. 2000; 67:291–300. PMID: 10983873.22. Dick SA, Epelman S. Chronic heart failure and inflammation: what do we really know? Circ Res. 2016; 119:159–176. PMID: 27340274.23. Rexrode KM, Pradhan A, Manson JE, Buring JE, Ridker PM. Relationship of total and abdominal adiposity with CRP and IL-6 in women. Ann Epidemiol. 2003; 13:674–682. PMID: 14599731.24. Forsythe LK, Wallace JM, Livingstone MB. Obesity and inflammation: the effects of weight loss. Nutr Res Rev. 2008; 21:117–133. PMID: 19087366.25. Bianchi VE. Weight loss is a critical factor to reduce inflammation. Clin Nutr ESPEN. 2018; 28:21–35. PMID: 30390883.26. Mirza S, Hossain M, Mathews C, Martinez P, Pino P, Gay JL, Rentfro A, McCormick JB, Fisher-Hoch SP. Type 2-diabetes is associated with elevated levels of TNF-alpha, IL-6 and adiponectin and low levels of leptin in a population of Mexican Americans: a cross-sectional study. Cytokine. 2012; 57:136–142. PMID: 22035595.27. Wirth MD, Shivappa N, Khan S, Vyas S, Beresford L, Sofge J, Hébert JR. Impact of a 3-month anti-inflammatory dietary intervention focusing on watermelon on body habitus, inflammation, and metabolic markers: a pilot study. Nutr Metab Insights. 2020; 13:1178638819899398. PMID: 31975781.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Erratum: Evaluation of medical nutrition therapy using the food-based index of dietary inflammatory potential (FBDI) in diabetes mellitus patients
- Effects of Korean Food-based Dietary Inflammatory Index Potential on the incidence of diabetes and HbA1c level in Korean adults aged 40 years and older
- Development of a food-based index of dietary inflammatory potential for Koreans and its relationship with metabolic syndrome
- Food Nutrition Information, Where Can We Get Sources of Nutrition Information in Food?
- Evaluation of Nutrition Education for Diabetes Mellitus Management of Older Adults