Cardiovasc Prev Pharmacother.
2023 Apr;5(2):41-48. 10.36011/cpp.2023.5.e4.
Optimal target blood pressure in older patients with hypertension
- Affiliations
-
- 1Division of Geriatrics, Department of Internal Medicine, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2541757
- DOI: http://doi.org/10.36011/cpp.2023.5.e4
Abstract
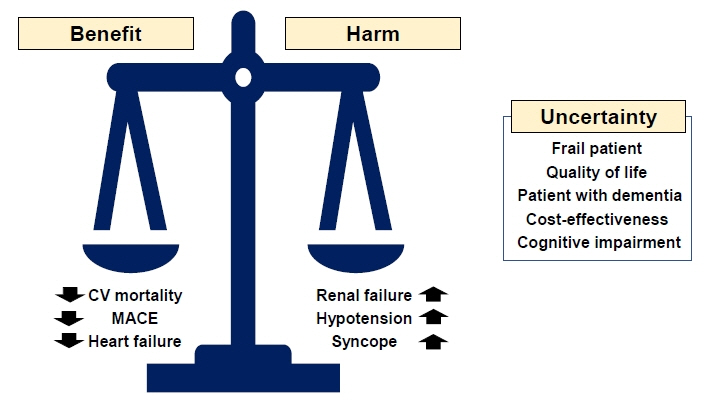
- Hypertension is a common condition among older adults, and blood pressure (BP) control is effective for preventing cardiovascular morbidity and mortality even among the oldest-old adults. However, the optimal target BP for older patients with hypertension has been a subject of debate, with previous clinical trials providing conflicting evidence. Determining the optimal target BP for older adults is a complex issue that requires considering comorbidities, frailty, quality of life, and goals of care. As such, BP targets should be individualized based on each patient's unique health status and risk factors, and treatment should be closely monitored to ensure that it is effective and well-tolerated. The benefits and risks of intensive BP control should be carefully weighed in the context of the patient's overall health status and treatment goals. Ultimately, the decision to pursue intensive BP control should be made through shared decision-making between patients and their healthcare providers.
Keyword
Figure
Reference
-
1. Benetos A, Petrovic M, Strandberg T. Hypertension management in older and frail older patients. Circ Res. 2019; 124:1045–60.2. Bavishi C, Bangalore S, Messerli FH. Outcomes of intensive blood pressure lowering in older hypertensive patients. J Am Coll Cardiol. 2017; 69:486–93.3. Tsao CW, Aday AW, Almarzooq ZI, Alonso A, Beaton AZ, Bittencourt MS, et al. Heart disease and stroke statistics: 2022 update: a report from the American Heart Association. Circulation. 2022; 145:e153–639.4. NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. 2021; 398:957–80.5. Lee JH, Kim KI, Cho MC. Current status and therapeutic considerations of hypertension in the elderly. Korean J Intern Med. 2019; 34:687–95.6. Korean Society of Hypertension (KSH); Hypertension Epidemiology Research Working Group. Korea hypertension fact sheet 2022. KSH; 2022.7. Ungvari Z, Toth P, Tarantini S, Prodan CI, Sorond F, Merkely B, et al. Hypertension-induced cognitive impairment: from pathophysiology to public health. Nat Rev Nephrol. 2021; 17:639–54.8. Hajjar I, Quach L, Yang F, Chaves PH, Newman AB, Mukamal K, et al. Hypertension, white matter hyperintensities, and concurrent impairments in mobility, cognition, and mood: the Cardiovascular Health Study. Circulation. 2011; 123:858–65.9. Benetos A, Bulpitt CJ, Petrovic M, Ungar A, Agabiti Rosei E, Cherubini A, et al. An expert opinion from the European Society of Hypertension-European Union Geriatric Medicine Society Working Group on the management of hypertension in very old, frail subjects. Hypertension. 2016; 67:820–5.10. Rivasi G, Tortu V, D’Andria MF, Turrin G, Ceolin L, Rafanelli M, et al. Hypertension management in frail older adults: a gap in evidence. J Hypertens. 2021; 39:400–7.11. Liao CT, Toh HS, Sun L, Yang CT, Hu A, Wei D, et al. Cost-effectiveness of intensive vs standard blood pressure control among older patients with hypertension. JAMA Netw Open. 2023; 6:e230708.12. JATOS Study Group. Principal results of the Japanese trial to assess optimal systolic blood pressure in elderly hypertensive patients (JATOS). Hypertens Res. 2008; 31:2115–27.13. Williamson JD, Supiano MA, Applegate WB, Berlowitz DR, Campbell RC, Chertow GM, et al. Intensive vs standard blood pressure control and cardiovascular disease outcomes in adults aged ≥75 years: a randomized clinical trial. JAMA. 2016; 315:2673–82.14. Zhang W, Zhang S, Deng Y, Wu S, Ren J, Sun G, et al. Trial of intensive blood-pressure control in older patients with hypertension. N Engl J Med. 2021; 385:1268–79.15. SPRINT Research Group, Wright JT Jr, Williamson JD, Whelton PK, Snyder JK, Sink KM, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015; 373:2103–16.16. SPRINT MIND Investigators for the SPRINT Research Group, Williamson JD, Pajewski NM, Auchus AP, Bryan RN, Chelune G, et al. Effect of intensive vs standard blood pressure control on probable dementia: a randomized clinical trial. JAMA. 2019; 321:553–61.17. SPRINT Research Group, Lewis CE, Fine LJ, Beddhu S, Cheung AK, Cushman WC, et al. Final report of a trial of intensive versus standard blood-pressure control. N Engl J Med. 2021; 384:1921–30.18. Xie X, Atkins E, Lv J, Bennett A, Neal B, Ninomiya T, et al. Effects of intensive blood pressure lowering on cardiovascular and renal outcomes: updated systematic review and meta-analysis. Lancet. 2016; 387:435–43.19. Weiss J, Freeman M, Low A, Fu R, Kerfoot A, Paynter R, et al. Benefits and harms of intensive blood pressure treatment in adults aged 60 years or older: a systematic review and meta-analysis. Ann Intern Med. 2017; 166:419–29.20. Takami Y, Yamamoto K, Arima H, Sakima A. Target blood pressure level for the treatment of elderly hypertensive patients: a systematic review and meta-analysis of randomized trials. Hypertens Res. 2019; 42:660–8.21. Dallaire-Theroux C, Quesnel-Olivo MH, Brochu K, Bergeron F, O’Connor S, Turgeon AF, et al. Evaluation of intensive vs standard blood pressure reduction and association with cognitive decline and dementia: a systematic review and meta-analysis. JAMA Netw Open. 2021; 4:e2134553.22. Juraschek SP, Hu JR, Cluett JL, Ishak A, Mita C, Lipsitz LA, et al. Effects of intensive blood pressure treatment on orthostatic hypotension: a systematic review and individual participant-based meta-analysis. Ann Intern Med. 2021; 174:58–68.23. Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018; 71:e13–115.24. Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 Practice guidelines for the management of arterial hypertension of the European Society of Hypertension and the European Society of Cardiology: ESH/ESC Task Force for the Management of Arterial Hypertension. J Hypertens. 2018; 36:2284–309.25. Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese Society of Hypertension guidelines for the management of hypertension (JSH 2019). Hypertens Res. 2019; 42:1235–481.26. Kim HL, Lee EM, Ahn SY, Kim KI, Kim HC, Kim JH, et al. The 2022 focused update of the 2018 Korean Hypertension Society guidelines for the management of hypertension. Clin Hypertens. 2023; 29:11.27. Kim KI, Ihm SH, Kim GH, Kim HC, Kim JH, Lee HY, et al. 2018 Korean society of hypertension guidelines for the management of hypertension: part III: hypertension in special situations. Clin Hypertens. 2019; 25:19.28. Muller M, Smulders YM, de Leeuw PW, Stehouwer CD. Treatment of hypertension in the oldest old: a critical role for frailty? Hypertension. 2014; 63:433–41.29. Forman DE, Maurer MS, Boyd C, Brindis R, Salive ME, Horne FM, et al. Multimorbidity in older adults with cardiovascular disease. J Am Coll Cardiol. 2018; 71:2149–61.30. Choi JY, Chun S, Kim H, Jung YI, Yoo S, Kim KI. Analysis of blood pressure and blood pressure variability pattern among older patients in long-term care hospitals: an observational study analysing the Health-RESPECT (integrated caRE Systems for elderly PatiEnts using iCT) dataset. Age Ageing. 2022; 51:afac018.31. Jung HW, Kim KI. Blood pressure variability and cognitive function in the elderly. Pulse (Basel). 2013; 1:29–34.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Stroke Update: Optimal Blood Pressure Management for Stroke Prevention
- Target goal blood pressure in hypertension management
- Blood pressure and heart failure
- Recent Guideline for the Management of Hypertension in Patients with Diabetes
- Current Controversies over the Management of Elderly Hypertension with Impaired Renal Function