Acute Crit Care.
2023 Feb;38(1):68-75. 10.4266/acc.2022.01375.
Risk factors for hospital mortality in intensive care unit survivors: a retrospective cohort study
- Affiliations
-
- 1Universidade Estadual de Londrina, Londrina, Brazil
- 2Departamento de Clínica Médica, Universidade Estadual de Londrina, Londrina, Brazil
- 3Universidade de São Paulo, São Paulo, Brzail
- 4Departamento de Fisioterapia, Universidade Estadual de Londrina, São Paulo, Brazil
- KMID: 2540316
- DOI: http://doi.org/10.4266/acc.2022.01375
Abstract
- Background
Deaths can occur after a patient has survived treatment for a serious illness in an intensive care unit (ICU). Mortality rates after leaving the ICU can be considered indicators of health care quality. This study aims to describe risk factors and mortality of surviving patients discharged from an ICU in a university hospital.
Methods
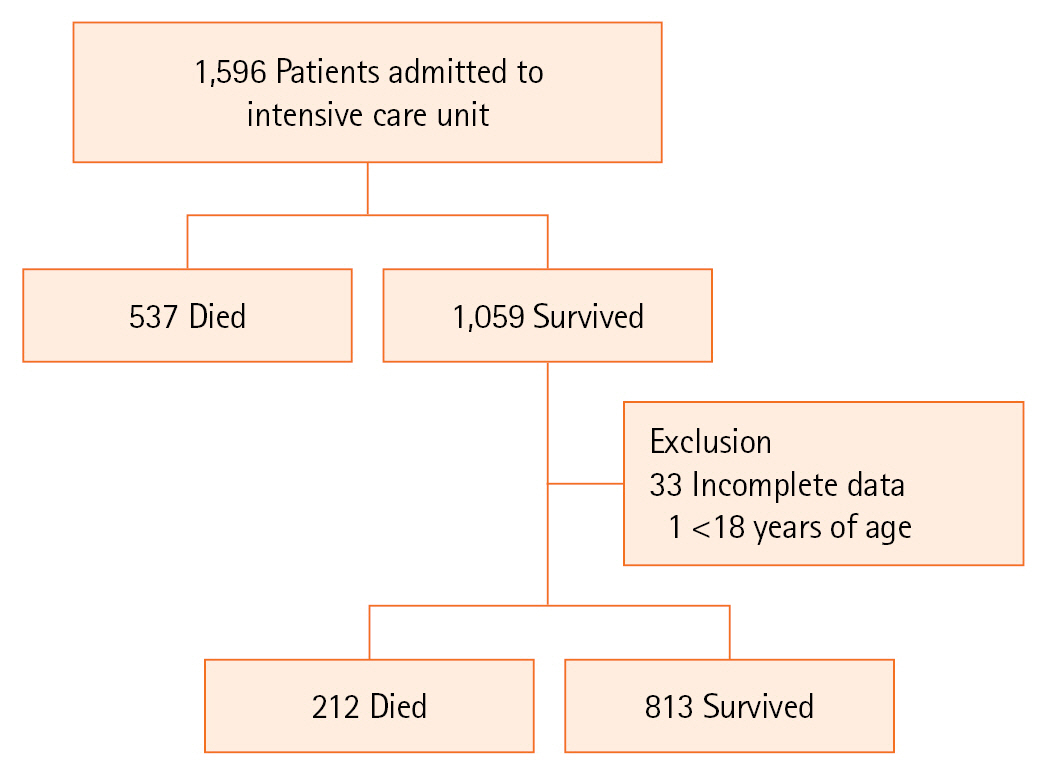
Retrospective cohort study carried out from January 2017 to December 2018. Data on age, sex, length of hospital stay, diagnosis on admission to the ICU, hospital discharge outcome, presence of infection, and Simplified Acute Physiology Score III (SAPS 3) prognostic score were collected. Infected patients were considered as those being treated for an infection on discharge from the ICU. Patients were divided into survivors and non-survivors on leaving the hospital. The association between the studied variables was performed using the logistic regression model.
Results
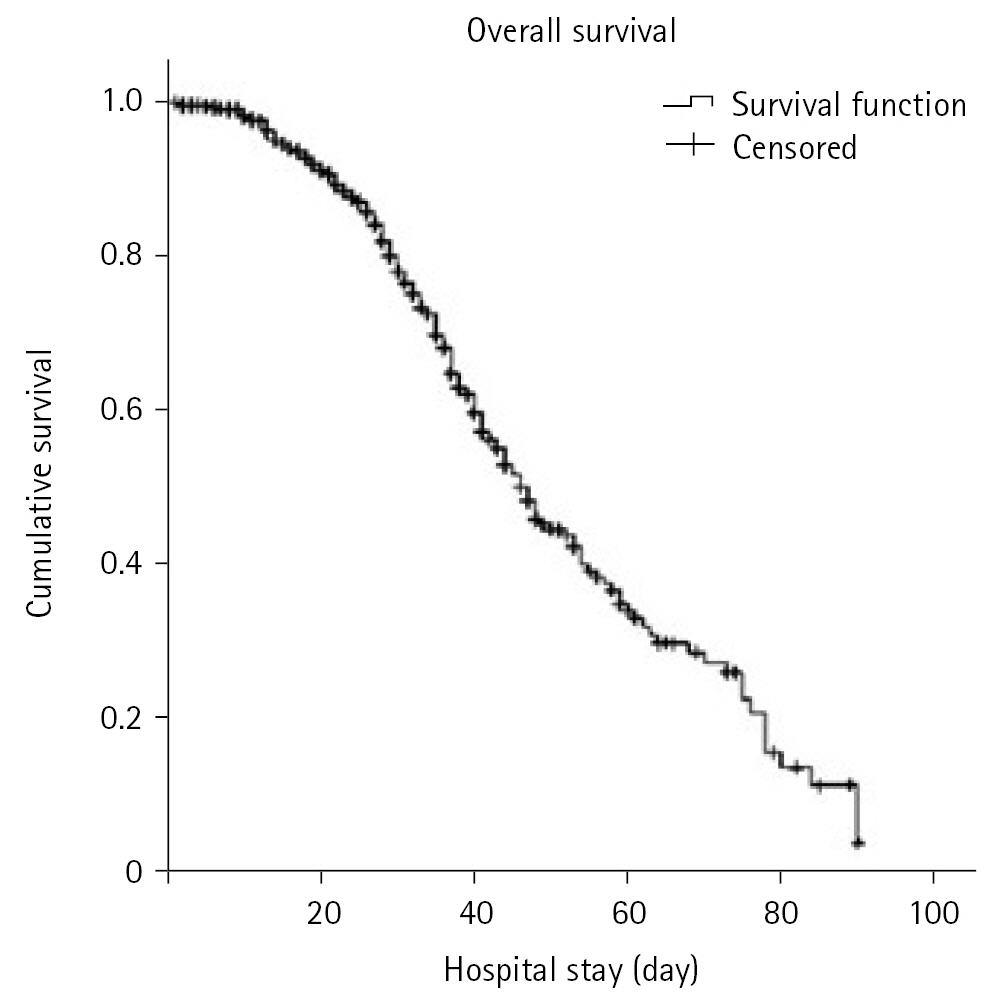
A total of 1,025 patients who survived hospitalization in the ICU were analyzed, of which 212 (20.7%) died after leaving the ICU. When separating the groups of survivors and non-survivors according to hospital outcome, the median age was higher among non-survivors. Longer hospital stays and higher SAPS 3 score values were observed among non-survivors. In the logistic regression, the variables age, length of hospital stay, SAPS 3, presence of infection, and readmission to the ICU were associated with hospital mortality.
Conclusions
Infection on ICU discharge, ICU readmission, age, length of hospital stay, and SAPS 3 score increased risk of death in ICU survivors.
Keyword
Figure
Reference
-
1. Goldhill DR, Sumner A. Outcome of intensive care patients in a group of British intensive care units. Crit Care Med. 1998; 26:1337–45.2. Rowan KM, Kerr JH, Major E, McPherson K, Short A, Vessey MP. Intensive Care Society’s APACHE II study in Britain and Ireland--II: Outcome comparisons of intensive care units after adjustment for case mix by the American APACHE II method. BMJ. 1993; 307:977–81.3. Smith L, Orts CM, O’Neil I, Batchelor AM, Gascoigne AD, Baudouin SV. TISS and mortality after discharge from intensive care. Intensive Care Med. 1999; 25:1061–5.4. Azoulay E, Adrie C, De Lassence A, Pochard F, Moreau D, Thiery G, et al. Determinants of postintensive care unit mortality: a prospective multicenter study. Crit Care Med. 2003; 31:428–32.5. Ranzani OT, Prada LF, Zampieri FG, Battaini LC, Pinaffi JV, Setogute YC, et al. Failure to reduce C-reactive protein levels more than 25% in the last 24 hours before intensive care unit discharge predicts higher in-hospital mortality: a cohort study. J Crit Care. 2012; 27:525.6. Campbell AJ, Cook JA, Adey G, Cuthbertson BH. Predicting death and readmission after intensive care discharge. Br J Anaesth. 2008; 100:656–62.7. Ponzoni CR, Corrêa TD, Filho RR, Serpa Neto A, Assunção MS, Pardini A, et al. Readmission to the intensive care unit: incidence, risk factors, resource use, and outcomes: a retrospective cohort study. Ann Am Thorac Soc. 2017; 14:1312–9.8. Rodrigues CM, Pires EM, Feliciano JP, Vieira JM Jr, Taniguchi LU. Admission factors associated with intensive care unit readmission in critically ill oncohematological patients: a retrospective cohort study. Rev Bras Ter Intensiva. 2016; 28:33–9.9. Lin WT, Chen WL, Chao CM, Lai CC. The outcomes and prognostic factors of the patients with unplanned intensive care unit readmissions. Medicine (Baltimore). 2018; 97:e11124.10. Hosein FS, Roberts DJ, Turin TC, Zygun D, Ghali WA, Stelfox HT. A meta-analysis to derive literature-based benchmarks for readmission and hospital mortality after patient discharge from intensive care. Crit Care. 2014; 18:715.11. Keegan MT, Soares M. What every intensivist should know about prognostic scoring systems and risk-adjusted mortality. Rev Bras Ter Intensiva. 2016; 28:264–9.12. Serpa Neto A, Assunção MS, Pardini A, Silva E. Feasibility of transitioning from APACHE II to SAPS III as prognostic model in a Brazilian general intensive care unit: a retrospective study. Sao Paulo Med J. 2015; 133:199–205.13. Magiorakos AP, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012; 18:268–81.14. Morland M, Haagensen R, Dahl FA, Berdal JE. Epidemiology and prognoses in a medical intermediate care unit. Tidsskr Nor Laegeforen. 2018; 138.15. Capuzzo M, Volta C, Tassinati T, Moreno RP, Valentin A, Guidet B, et al. Hospital mortality of adults admitted to intensive care units in hospitals with and without intermediate care units: a multicentre European cohort study. Crit Care. 2014; 18:551.16. Hosein FS, Bobrovitz N, Berthelot S, Zygun D, Ghali WA, Stelfox HT. A systematic review of tools for predicting severe adverse events following patient discharge from intensive care units. Crit Care. 2013; 17:R102.17. Haniffa R, Isaam I, De Silva AP, Dondorp AM, De Keizer NF. Performance of critical care prognostic scoring systems in low and middle-income countries: a systematic review. Crit Care. 2018; 22:18.18. Fuchs PA, Czech IJ, Krzych ŁJ. The pros and cons of the prediction game: the never-ending debate of mortality in the intensive care unit. Int J Environ Res Public Health. 2019; 16:3394.19. Donnelly JP, Wang XQ, Iwashyna TJ, Prescott HC. Readmission and death after initial hospital discharge among patients with COVID-19 in a large multihospital system. JAMA. 2021; 325:304–6.20. Madotto F, McNicholas B, Rezoagli E, Pham T, Laffey JG, Bellani G, et al. Death in hospital following ICU discharge: insights from the LUNG SAFE study. Crit Care. 2021; 25:144.21. Santamaria JD, Duke GJ, Pilcher DV, Cooper DJ, Moran J, Bellomo R, et al. The timing of discharge from the intensive care unit and subsequent mortality: a prospective, multicenter study. Am J Respir Crit Care Med. 2015; 191:1033–9.22. Azoulay E, Alberti C, Legendre I, Buisson CB, Le Gall JR, European Sepsis Group. Post-ICU mortality in critically ill infected patients: an international study. Intensive Care Med. 2005; 31:56–63.23. Barrasa-Villar JI, Aibar-Remón C, Prieto-Andrés P, Mareca-Doñate R, Moliner-Lahoz J. Impact on morbidity, mortality, and length of stay of hospital-acquired infections by resistant microorganisms. Clin Infect Dis. 2017; 65:644–52.24. Serra-Burriel M, Keys M, Campillo-Artero C, Agodi A, Barchitta M, Gikas A, et al. Impact of multi-drug resistant bacteria on economic and clinical outcomes of healthcare-associated infections in adults: systematic review and meta-analysis. PLoS One. 2020; 15:e0227139.25. Rosa RG, Falavigna M, Robinson CC, Sanchez EC, Kochhann R, Schneider D, et al. Early and late mortality following discharge from the ICU: a multicenter prospective cohort study. Crit Care Med. 2020; 48:64–72.26. Taniguchi LU, Ramos FJ, Momma AK, Martins Filho AP, Bartocci JJ, Lopes MF, et al. Subjective score and outcomes after discharge from the intensive care unit: a prospective observational study. J Int Med Res. 2019; 47:4183–93.27. Kołpa M, Wałaszek M, Gniadek A, Wolak Z, Dobroś W. Incidence, microbiological profile and risk factors of healthcare-associated infections in intensive care units: a 10 year observation in a provincial hospital in Southern Poland. Int J Environ Res Public Health. 2018; 15:112.28. Ferreira LL, Azevedo LM, Salvador PT, Morais SH, Paiva RM, Santos VE. Nursing care in healthcare-associated infections: a scoping review. Rev Bras Enferm. 2019; 72:476–83.29. Mota EC, Oliveira SP, Silveira BR, Silva PL, Oliveira AC. Incidência da pneumonia associada à ventilação mecânica em unidade de terapia intensiva. Medicina (Ribeirão Preto). 2017; 50:39–46.30. Navon-Venezia S, Kondratyeva K, Carattoli A. Klebsiella pneumoniae: a major worldwide source and shuttle for antibiotic resistance. FEMS Microbiol Rev. 2017; 41:252–75.31. de Maio Carrilho CM, de Oliveira LM, Gaudereto J, Perozin JS, Urbano MR, Camargo CH, et al. A prospective study of treatment of carbapenem-resistant Enterobacteriaceae infections and risk factors associated with outcome. BMC Infect Dis. 2016; 16:629.32. Breijyeh Z, Jubeh B, Karaman R. Resistance of Gram-negative bacteria to current antibacterial agents and approaches to resolve it. Molecules. 2020; 25:1340.33. Tejerina Álvarez EE, Gómez Mediavilla KA, Rodríguez Solís C, Valero González N, Lorente Balanza JÁ. Risk factors for readmission to ICU and analysis of intra-hospital mortality. Med Clin (Barc). 2022; 158:58–64.34. Londoño Restrepo J, Macias Ospina IC, Ochoa Jaramillo FL. Factores de riesgo asociados a infecciones por bacterias multirresistentes derivadas de la atención en salud en una institución hospitalaria de la ciudad de Medellín 2011-2014. Infect. 2016; 20:77–83.35. Bergamasco E Paula R, Tanita MT, Festti J, Queiroz Cardoso LT, Carvalho Grion CM. Analysis of readmission rates to the intensive care unit after implementation of a rapid response team in a University Hospital. Med Intensiva. 2017; 41:411–7.36. Jung B, Daurat A, De Jong A, Chanques G, Mahul M, Monnin M, et al. Rapid response team and hospital mortality in hospitalized patients. Intensive Care Med. 2016; 42:494–504.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Risk Factors for Cognitive Impairment in Intensive Care Unit Survivors
- Factors associated with mortality after asthma admission in the intensive care unit of a tertiary referral hospital
- Comment on “Risk factors for intensive care unit readmission after lung transplantation: a retrospective cohort study”
- Rehabilitation in Intensive Care Unit
- Impacts of Financial Coverage on Long-Term Outcome of Intensive Care Unit Survivors in South Korea