Acute Crit Care.
2023 Feb;38(1):41-48. 10.4266/acc.2022.01235.
Predicting factors associated with prolonged intensive care unit stay of patients with COVID-19
- Affiliations
-
- 1Department of Critical Care Medicine, National Cancer Center, Goyang, Korea
- 2Department of Surgery, National Cancer Center, Goyang, Korea
- 3Department of Internal Medicine, National Cancer Center, Goyang, Korea
- 4Department of Anesthesiology, National Cancer Center, Goyang, Korea
- 5Biostatistics Collaboration Team, National Cancer Center, Goyang, Korea
- KMID: 2540313
- DOI: http://doi.org/10.4266/acc.2022.01235
Abstract
- Background
Predicting the length of stay (LOS) for coronavirus disease 2019 (COVID-19) patients in the intensive care unit (ICU) is essential for efficient use of ICU resources. We analyzed the clinical characteristics of patients with severe COVID-19 based on their clinical care and determined the predictive factors associated with prolonged LOS.
Methods
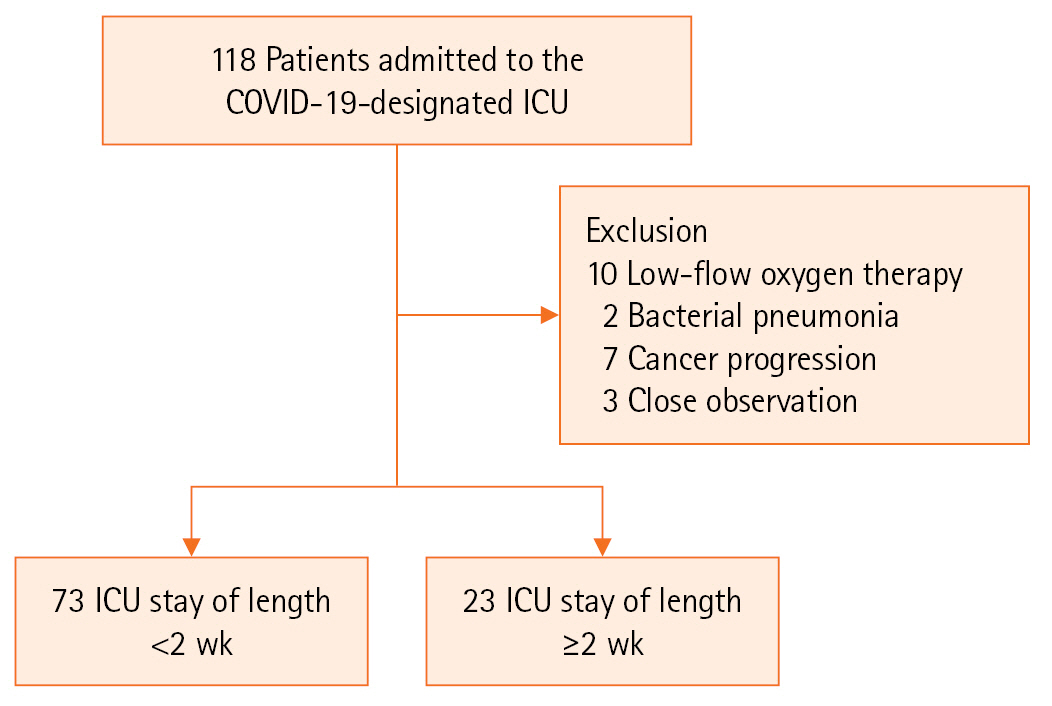
We included 96 COVID-19 patients who received oxygen therapy at a high-flow nasal cannula level or above after ICU admission during March 2021 to February 2022. The demographic characteristics at the time of ICU admission and results of severity analysis (Sequential Organ Failure Assessment [SOFA], Acute Physiology and Chronic Health Evaluation [APACHE] II), blood tests, and ICU treatments were analyzed using a logistic regression model. Additionally, blood tests (C-reactive protein, D-dimer, and the PaO2 to FiO2 ratio [P/F ratio]) were performed on days 3 and 5 of ICU admission to identify factors associated with prolonged LOS.
Results
Univariable analyses showed statistically significant results for SOFA score at the time of ICU admission, C-reactive protein level, high-dose steroids, mechanical ventilation (MV) care, continuous renal replacement therapy, extracorporeal membrane oxygenation, and prone position. Multivariable analysis showed that MV care and P/F ratio on hospital day 5 were independent factors for prolonged ICU LOS. For D-dimer, no significant variation was observed at admission; however, after days 3 and 5 days of admission, significant between-group variation was detected.
Conclusions
MV care and P/F ratio on hospital day 5 are independent factors that can predict prolonged LOS for COVID-19 patients.
Figure
Reference
-
1. Choi JY. COVID-19 in South Korea. Postgrad Med J. 2020; 96:399–402.2. Bouadma L, Lescure FX, Lucet JC, Yazdanpanah Y, Timsit JF. Severe SARS-CoV-2 infections: practical considerations and management strategy for intensivists. Intensive Care Med. 2020; 46:579–82.3. Chen J, Qi T, Liu L, Ling Y, Qian Z, Li T, et al. Clinical progression of patients with COVID-19 in Shanghai, China. J Infect. 2020; 80:e1–6.4. Duggal A, Pinto R, Rubenfeld G, Fowler RA. Global variability in reported mortality for critical illness during the 2009-10 influenza A(H1N1) pandemic: a systematic review and meta-regression to guide reporting of outcomes during disease outbreaks. PLoS One. 2016; 11:e0155044.5. Elhadi M, Msherghi A, Alkeelani M, Alsuyihili A, Khaled A, Buzreg A, et al. Concerns for low-resource countries, with under-prepared intensive care units, facing the COVID-19 pandemic. Infect Dis Health. 2020; 25:227–32.6. Lai CC, Wang CY, Wang YH, Hsueh SC, Ko WC, Hsueh PR. Global epidemiology of coronavirus disease 2019 (COVID-19): disease incidence, daily cumulative index, mortality, and their association with country healthcare resources and economic status. Int J Antimicrob Agents. 2020; 55:105946.7. Bravata DM, Perkins AJ, Myers LJ, Arling G, Zhang Y, Zillich AJ, et al. Association of intensive care unit patient load and demand with mortality rates in us department of veterans affairs hospitals during the COVID-19 pandemic. JAMA Netw Open. 2021; 4:e2034266.8. Wilde H, Mellan T, Hawryluk I, Dennis JM, Denaxas S, Pagel C, et al. The association between mechanical ventilator compatible bed occupancy and mortality risk in intensive care patients with COVID-19: a national retrospective cohort study. BMC Med. 2021; 19:213.9. Kim JH, An JA, Min PK, Bitton A, Gawande AA. How South Korea responded to the COVID-19 outbreak in Daegu. NEJM Catal Innov Care Deliv. 2020. 1:1–4.10. Sen-Crowe B, Sutherland M, McKenney M, Elkbuli A. A closer look into global hospital beds capacity and resource shortages during the COVID-19 pandemic. J Surg Res. 2021; 260:56–63.11. Jain V, Yuan JM. Predictive symptoms and comorbidities for severe COVID-19 and intensive care unit admission: a systematic review and meta-analysis. Int J Public Health. 2020; 65:533–546.12. Burian E, Jungmann F, Kaissis GA, Lohöfer FK, Spinner CD, Lahmer T, et al. Intensive care risk estimation in COVID-19 pneumonia based on clinical and imaging parameters: experiences from the Munich Cohort. J Clin Med. 2020; 9:1514.13. Bertelli M, Fusina F, Prezioso C, Cavallo E, Nencini N, Crisci S, et al. COVID-19 ARDS is characterized by increased dead space ventilation compared with non-COVID ARDS. Respir Care. 2021; 66:1406–15.14. Li X, Ma X. Acute respiratory failure in COVID-19: is it "typical" ARDS? Crit Care. 2020; 24:198.15. Cho YJ, Moon JY, Shin ES, Kim JH, Jung H, Park SY, et al. Clinical practice guideline of acute respiratory distress syndrome. Korean J Crit Care Med. 2016; 31:76–100.16. Alhazzani W, Møller MH, Arabi YM, Loeb M, Gong MN, Fan E, et al. Surviving sepsis campaign: guidelines on the management of critically ill adults with Coronavirus Disease 2019 (COVID-19). Intensive Care Med. 2020; 46:854–87.17. Zawaydeh Q, Husain A, Cotton S, Malhotra A. The effect of steroid dosing on risk of secondary infection in COVID-19 critically ill patients. TP091 epidemiology and translational advances in SARS-COV-2. Am J Respir Crit Care Med. 2021; 203:A3806.18. Huang E, Jordan SC. Tocilizumab for Covid-19: the ongoing search for effective therapies. N Engl J Med. 2020; 383:2387–8.19. Vlachos S, Wong A, Metaxa V, Canestrini S, Lopez Soto C, Periselneris J, et al. Hospital mortality and resource implications of hospitalisation with COVID-19 in London, UK: a prospective cohort study. Crit Care Res Pract. 2021; 2021:8832660.20. Kang SJ, Jung SI. Age-related morbidity and mortality among patients with COVID-19. Infect Chemother. 2020; 52:154–64.21. Reddy RK, Charles WN, Sklavounos A, Dutt A, Seed PT, Khajuria A. The effect of smoking on COVID-19 severity: a systematic review and meta-analysis. J Med Virol. 2021; 93:1045–56.22. Beigmohammadi MT, Amoozadeh L, Rezaei Motlagh F, Rahimi M, Maghsoudloo M, Jafarnejad B, et al. Mortality predictive value of APACHE II and SOFA scores in COVID-19 patients in the intensive care unit. Can Respir J. 2022; 2022:5129314.23. Tapaskar N, Colon Hidalgo D, Koo G, Shingada K, Rao S, Rodriguez R, et al. Sedation usage in COVID-19 acute respiratory distress syndrome: a multicenter study. Ann Pharmacother. 2022; 56:117–23.24. Lee BY, Lee SI, Baek MS, Baek AR, Na YS, Kim JH, et al. Lower driving pressure and neuromuscular blocker use are associated with decreased mortality in patients with COVID-19 ARDS. Respiratory Care. 2022; Feb. 1. 67:216–26.25. Yang AP, Liu JP, Tao WQ, Li HM. The diagnostic and predictive role of NLR, d-NLR and PLR in COVID-19 patients. Int Immunopharmacol. 2020; 84:106504.26. Shang W, Dong J, Ren Y, Tian M, Li W, Hu J, et al. The value of clinical parameters in predicting the severity of COVID-19. J Med Virol. 2020; 92:2188–92.27. Prediletto I, D'Antoni L, Carbonara P, Daniele F, Dongilli R, Flore R, et al. Standardizing PaO2 for PaCO2 in P/F ratio predicts in-hospital mortality in acute respiratory failure due to Covid-19: a pilot prospective study. Eur J Intern Med. 2021; 92:48–54.28. Rostami M, Mansouritorghabeh H. D-dimer level in COVID-19 infection: a systematic review. Expert Rev Hematol. 2020; 13:1265–75.29. Iba T, Levy JH, Connors JM, Warkentin TE, Thachil J, Levi M. The unique characteristics of COVID-19 coagulopathy. Crit Care. 2020; 24:360.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prolonged intensive care: muscular functional, and nutritional insights from the COVID-19 pandemic
- The effect of COVID-19 pandemic on the length of stay and outcomes in the emergency department
- New-Onset Seizures in Patients With COVID-19: A Case Series From a Single Public Hospital in Korea
- Risk factors for intensive care unit admission and mortality in hospitalized COVID-19 patients
- Evaluation of the Clinical Effect of Intravenous Glutamine on Intensive Care Unit Patients