J Korean Neurosurg Soc.
2023 Mar;66(2):199-204. 10.3340/jkns.2022.0165.
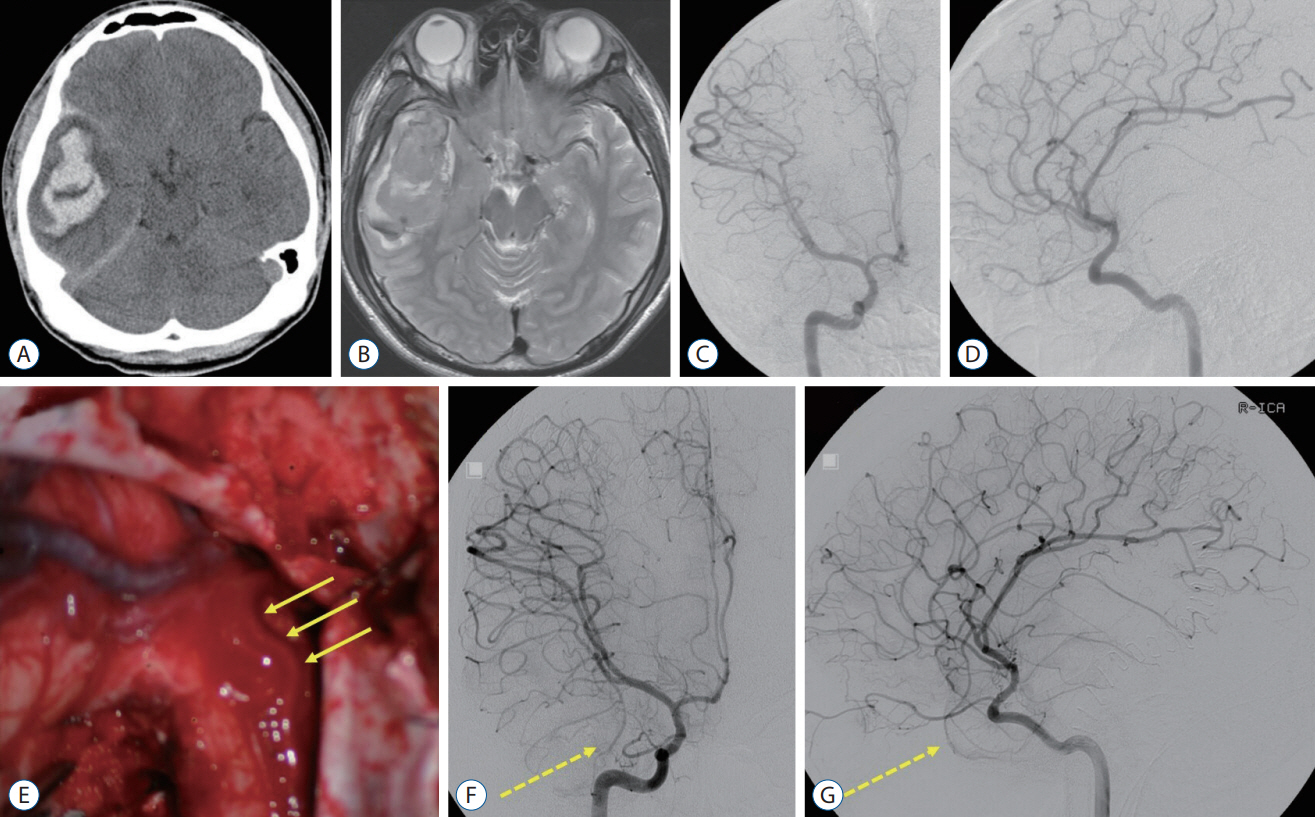
Delayed Appearance of Radiologically Occult Cerebral Arteriovenous Malformation : A Case Report and Literature Review
- Affiliations
-
- 1Department of Neurosurgery, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2539881
- DOI: http://doi.org/10.3340/jkns.2022.0165
Abstract
- It is critical to identify the ruptured cerebral arteriovenous malformations (AVMs) for secondary prevention. However, there are rare cases unidentified on the radiological evaluation. We report on a patient with the delayed appearance of radiologically occult AVM as a probable cause of the previous intracerebral hemorrhage (ICH). An 18-year-old male patient presented with a right temporal ICH. The preoperative radiological examination did not reveal any causative lesions. Because of the intraoperative findings suggesting an AVM, however, only hematoma was evacuated. Disappointedly, there were no abnormal findings on postoperative and follow-up radiographic examinations. Eleven years later, the patient presented with an epileptic seizure, and an AVM was identified in the right temporal lobe where ICH had occurred before. The patient underwent partial glue embolization followed by total surgical resection of the AVM and anterior temporal lobe. Based on the literature review published in the era of magnetic resonance imaging, common clinical presentation of radiologically occult AVMs included headache and seizure. Most of them were confirmed by pathologic examination after surgery. In cases of the ICH of unknown etiology in young patients, long-term follow-up should be considered.
Figure
Reference
-
References
1. Andaluz N, Myseros JS, Sathi S, Crone KR, Tew JM Jr. Recurrence of cerebral arteriovenous malformations in children: report of two cases and review of the literature. Surg Neurol. 62:324–330. discussion 330-331. 2004.2. Berker M, Ulus A, Palaoglu S, Soylemezoglu F, Ay H, Cekirge S. Intracranial haemorrhage probably due to an angiographically occult avm after carotid stenting. a case report. Interv Neuroradiol. 9:315–320. 2003.3. Choi JH, Mohr JP. Brain arteriovenous malformations in adults. Lancet Neurol. 4:299–308. 2005.4. Crawford JV, Russell DS. Cryptic arteriovenous and venous hamartomas of the brain. J Neurol Neurosurg Psychiatry. 19:1–11. 1956.5. Ebeling JD, Tranmer BI, Davis KA, Kindt GW, DeMasters BK. Thrombosed arteriovenous malformations: a type of occult vascular malformation. magnetic resonance imaging and histopathological correlations. Neurosurgery. 23:605–610. 1988.6. Fujii M, Akimura T, Ozaki S, Kato S, Ito H, Neshige R. An angiographically occult arteriovenous malformation in the medial parietal lobe presenting as seizures of medial temporal lobe origin. Epilepsia. 40:377–381. 1999.7. Gomori JM, Grossman RI, Goldberg HI, Hackney DB, Zimmerman RA, Bilaniuk LT. Occult cerebral vascular malformations: high-field MR imaging. Radiology. 158:707–713. 1986.8. Heit JJ, Thakur NH, Iv M, Fischbein NJ, Wintermark M, Dodd RL, et al. Arterial-spin labeling MRI identifies residual cerebral arteriovenous malformation following stereotactic radiosurgery treatment. J Neuroradiol. 47:13–19. 2020.9. Hofmeister C, Stapf C, Hartmann A, Sciacca RR, Mansmann U, terBrugge K, et al. Demographic, morphological, and clinical characteristics of 1289 patients with brain arteriovenous malformation. Stroke. 31:1307–1310. 2000.10. Kader A, Goodrich JT, Sonstein WJ, Stein BM, Carmel PW, Michelsen WJ. Recurrent cerebral arteriovenous malformations after negative postoperative angiograms. J Neurosurg. 85:14–18. 1996.11. Kirkman MA, Tyrrell PJ, King AT, Patel HC. Imaging in young adults with intracerebral hemorrhage. Clin Neurol Neurosurg. 114:1297–1303. 2012.12. Koivunen RJ, Satopää J, Meretoja A, Strbian D, Haapaniemi E, Niemelä M, et al. Incidence, risk factors, etiology, severity and short-term outcome of non-traumatic intracerebral hemorrhage in young adults. Eur J Neurol. 22:123–132. 2015.13. Kwasi V, Niwa R, Hara T, Holsinger RMD. Diagnostic conundrums in cerebellar cryptic arteriovenous malformations. J Neurol Neurosci. 12:368. 2021.14. Lai SL, Chen ST, Lee TH, Ro LS, Hsu SP. Spontaneous intracerebral hemorrhage in young adults. Eur J Neurol. 12:310–316. 2005.15. Lawton MT, Rutledge WC, Kim H, Stapf C, Whitehead KJ, Li DY, et al. Brain arteriovenous malformations. Nat Rev Dis Primers. 1:15008. 2015.16. Le TT, Fischbein NJ, André JB, Wijman C, Rosenberg J, Zaharchuk G. Identification of venous signal on arterial spin labeling improves diagnosis of dural arteriovenous fistulas and small arteriovenous malformations. AJNR Am J Neuroradiol. 33:61–68. 2012.17. Lobato RD, Perez C, Rivas JJ, Cordobes F. Clinical, radiological, and pathological spectrum of angiographically occult intracranial vascular malformations. Analysis of 21 cases and review of the literature. J Neurosurg. 68:518–531. 1988.18. Morioka T, Nishio S, Hikita T, Chung LH, Soejima T. Marked growth of an angiographically occult arteriovenous malformation: case report. Neurosurgery. 23:101–103. 1988.19. Nagai Y, Anan M, Fujiki M. Cerebral arteriovenous malformations as acquired lesions: case reports and review of the literature. J Stroke Cerebrovasc Dis. 29:105157. 2020.20. Nagata K, Nikaido H, Mori T. Successful removal of cryptic arteriovenous malformation located at the upper ventral pons via subtemporal transtentorial approach. Surg Neurol. 46:116–121. 1996.21. New PF, Ojemann RG, Davis KR, Rosen BR, Heros R, Kjellberg RN, et al. MR and CT of occult vascular malformations of the brain. AJR Am J Roentgenol. 147:985–993. 1986.22. Ogilvy CS, Heros RC, Ojemann RG, New PF. Angiographically occult arteriovenous malformations. J Neurosurg. 69:350–355. 1988.23. Ruíz-Sandoval JL, Cantú C, Barinagarrementeria F. Intracerebral hemorrhage in young people: analysis of risk factors, location, causes, and prognosis. Stroke. 30:537–541. 1999.24. Sakaida H, Sakakura M, Tochio H, Nakao K, Taniguchi A, Yabana T. Chronic encapsulated intracerebral hematoma associated with angiographically occult arteriovenous malformation--case report. Neurol Med Chir (Tokyo). 33:638–642. 1993.25. Sure U, Butz N, Siegel AM, Mennel HD, Bien S, Bertalanffy H. Treatment-induced neoangiogenesis in cerebral arteriovenous malformations. Clin Neurol Neurosurg. 103:29–32. 2001.26. Tamaki M, Ohno K, Asano T, Niimi Y, Uchihara T, Hirakawa K. Cryptic arteriovenous malformation of the choroid plexus of the fourth ventricle--case report. Neurol Med Chir (Tokyo). 34:38–43. 1994.27. Tanaka M, Valavanis A. Role of superselective angiography in the detection and endovascular treatment of ruptured occult arteriovenous malformations. Interv Neuroradiol. 7:303–311. 2001.28. Tasiou A, Tzerefos C, Alleyne CH Jr, Boccardi E, Karlsson B, Kitchen N, et al. Arteriovenous malformations: congenital or acquired lesions? World Neurosurg. 134:e799–e807. 2020.29. Tatlisumak T, Cucchiara B, Kuroda S, Kasner SE, Putaala J. Nontraumatic intracerebral haemorrhage in young adults. Nat Rev Neurol. 14:237–250. 2018.30. Telischak NA, Detre JA, Zaharchuk G. Arterial spin labeling MRI: clinical applications in the brain. J Magn Reson Imaging. 41:1165–1180. 2015.31. Wakabayashi S, Ohno K, Shishido T, Tamaki M, Matsushima Y, Hirakawa K. Marked growth of a cerebral arteriovenous malformation: case report and review of the literature. Neurosurgery. 29:920–923. 1991.32. Wakai S, Okuhata S, Nagai M, Hirata K, Saitoh T, Katayama S, et al. Successful removal of an angiographically occult arteriovenous malformation of the ventral medulla. Br J Neurosurg. 4:429–434. 1990.33. Zhu XL, Chan MS, Poon WS. Spontaneous intracranial hemorrhage: which patients need diagnostic cerebral angiography? A prospective study of 206 cases and review of the literature. Stroke. 28:1406–1409. 1997.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Angiographically Occult Arteriovenous Malformation Mimicking Brain Tumor: Case Report
- Five Cases of Angiographically Occult Arteriovenous Malformation
- Pathophysiology of Cerebral Arteiovenous Malformation
- A Giant Aneurysmal Cerebral Arteriovenous Malformation in Childhood: Case Report
- Angiographically occult arteriovenous malformations causing intracerebral hemorrhage